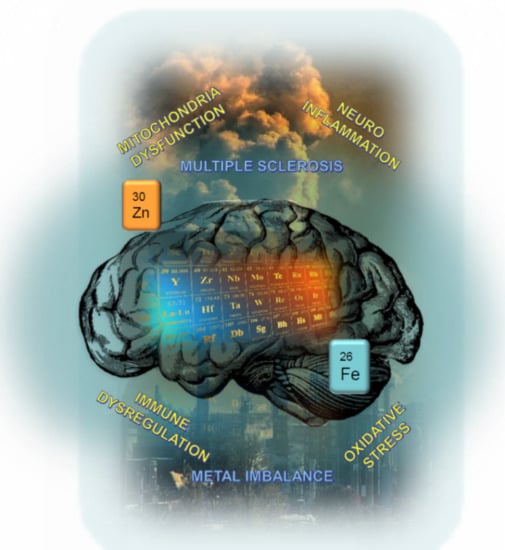
Metal Imbalance in Neurodegenerative Diseases with a Specific Concern to the Brain of Multiple Sclerosis Patients
Abstract
:1. Introduction
2. Essential Metals in the Normal Brain
2.1. Metal Homeostasis and Global Content
2.2. Regional Heterogeneity in Brain Parenchyma
3. Metals in Neurodegenerative Diseases and Neuroinflammation
3.1. Essential Metal Dyshomeostasis: A Cause or a Consequence?
3.2. Xenobiotic and Essential Metals Interplay
4. Metals Imbalance in Multiple Sclerosis Patients
4.1. Metals in the Blood or Serum
4.2. Iron in the Central Nervous System
4.3. Other Metals (Magnesium, Copper, Manganese, Zinc, Aluminum) in the Central Nervous System
5. Elemental Imaging for Understanding the Complexity of Metal Biochemistry?
6. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Madsen, E.; Gitlin, J.D. Copper and Iron Disorders of the Brain. Annu. Rev. Neurosci. Juill. 2007, 30, 317–337. [Google Scholar] [CrossRef]
- Zecca, L.; Youdim, M.B.H.; Riederer, P.; Connor, J.R.; Crichton, R.R. Iron, brain ageing and neurodegenerative disorders. Nat. Rev. Neurosci. 2004, 5, 863–873. [Google Scholar] [CrossRef] [PubMed]
- Que, E.L.; Domaille, D.W.; Chang, C.J. Metals in Neurobiology: Probing Their Chemistry and Biology with Molecular Imaging. Chem. Rev. 2008, 108, 1517–1549. [Google Scholar] [CrossRef]
- Prüss-Üstün, A.; Wolf, J.; Corvalán, C.; Bos, R.; Neira, M. Preventing Disease Through Healthy Environments: A Global Assessment of The Burden of Disease from Environmental Risks, 2nd ed.; World Health Organization: Geneva, Switzerland, 2016; p. 147. [Google Scholar]
- Earl, C.; Chantry, A.; Mohammad, N.; Glynn, P. Zinc Ions Stabilise the Association of Basic Protein with Brain Myelin Membranes. J. Neurochem. 1988, 51, 718–724. [Google Scholar] [CrossRef]
- Todorich, B.; Pasquini, J.M.; Garcia, C.I.; Paez, P.M.; Connor, J.R. Oligodendrocytes and myelination: The role of iron. Glia 2009, 57, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Tsang, D.; Tsang, Y.S.; Ho, W.K.K.; Wong, R.N.S. Myelin basic protein is a zinc-binding protein in brain: Possible role in myelin compaction. Neurochem. Res. 1997, 22, 811–819. [Google Scholar] [CrossRef]
- Kurien, B.T.; Scofield, R.H. Autoimmunity and oxidatively modified autoantigens. Autoimmun. Rev. 2008, 7, 567–573. [Google Scholar] [CrossRef] [Green Version]
- Fontenot, A.P.; Falta, M.T.; Kappler, J.W.; Dai, S.; McKee, A.S. Beryllium-Induced Hypersensitivity: Genetic Susceptibility and Neoantigen Generation. J. Immunol. 2015, 196, 22–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dexter, D.T.; Carayon, A.; Javoy-Agid, F.; Agid, Y.; Wells, F.R.; Daniel, S.E.; Lees, A.J.; Jenner, P.; Marsden, C.D. Alterations in the levels of iron, ferritin and other trace metals in parkinson’s disease and other neurodegenerative diseases affecting the basal ganglia. Brain 1991, 114, 1953–1975. [Google Scholar] [CrossRef] [PubMed]
- Dexter, D.T.; Sian, J.; Jenner, P.; Marsden, C.D. Implications of alterations in trace element levels in brain in Parkinson’s disease and other neurological disorders affecting the basal ganglia. Adv. Neurol. 1993, 60, 273–281. [Google Scholar] [PubMed]
- Dexter, D.T.; Wells, F.R.; Lee, A.J.; Agid, F.; Agid, Y.; Jenner, P.; Marsden, C.D. Increased Nigral Iron Content and Alterations in Other Metal Ions Occurring in Brain in Parkinson’s Disease. J. Neurochem. 1989, 52, 1830–1836. [Google Scholar] [CrossRef] [PubMed]
- Garza-Lombó, C.; Posadas, Y.; Quintanar, L.; Gonsebatt, M.E.; Franco, R. Neurotoxicity Linked to Dysfunctional Metal Ion Homeostasis and Xenobiotic Metal Exposure: Redox Signaling and Oxidative Stress. Antioxidants Redox Signal. 2018, 28, 1669–1703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bénardais, K.; Kotsiari, A.; Škuljec, J.; Koutsoudaki, P.N.; Gudi, V.; Singh, V.; Vulinovic, F.; Skripuletz, T.; Stangel, M. Cuprizone [Bis(Cyclohexylidenehydrazide)] is Selectively Toxic for Mature Oligodendrocytes. Neurotox. Res. 2013, 24, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Bates, M.N. Health effects of dental amalgam exposure: A retrospective cohort study. Int. J. Epidemiol. 2004, 33, 894–902. [Google Scholar] [CrossRef] [Green Version]
- Aminzadeh, K.K.; Etminan, M. Dental Amalgam and Multiple Sclerosis: A Systematic Review and Meta-Analysis. J. Public Health Dent. 2007, 67, 64–66. [Google Scholar] [CrossRef] [PubMed]
- Exley, C.; Mamutse, G.; Korchazhkina, O.; Pye, E.; Strekopytov, S.; Polwart, A.; Hawkins, C. Elevated urinary excretion of aluminium and iron in multiple sclerosis. Mult. Scler. J. 2006, 12, 533–540. [Google Scholar] [CrossRef]
- Jones, K.; Linhart, C.; Hawkins, C.; Exley, C. Urinary Excretion of Aluminium and Silicon in Secondary Progressive Multiple Sclerosis. EBioMedicine 2017, 26, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Hametner, S.; Wimmer, I.; Haider, L.; Pfeifenbring, S.; Brück, W.; Lassmann, H. Iron and neurodegeneration in the multiple sclerosis brain: Iron in the MS Brain. Ann. Neurol. 2013, 74, 848–861. [Google Scholar] [CrossRef]
- LeVine, S.M.; Lynch, S.G.; Ou, C.-N.; Wulser, M.J.; Tam, E.; Boo, N. Ferritin, transferrin and iron concentrations in the cerebrospinal fluid of multiple sclerosis patients. Brain Res. 1999, 821, 511–515. [Google Scholar] [CrossRef]
- Ristori, G.; Brescianini, S.; Pino, A.; Visconti, A.; Vittori, D.; Coarelli, G.; Cotichini, R.; Bocca, B.; Forte, G.; Pozzilli, C.; et al. Serum elements and oxidative status in clinically isolated syndromes: Imbalance and predictivity. Neurology 2011, 76, 549–555. [Google Scholar] [CrossRef]
- Chang, C.J. Searching for harmony in transition-metal signaling. Nat. Chem. Biol. 2015, 11, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Barnham, K.J.; Bush, A.I. Biological metals and metal-targeting compounds in major neurodegenerative diseases. Chem. Soc. Rev. 2014, 43, 6727–6749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortiz, E.; Pasquini, J.M.; Thompson, K.; Felt, B.; Butkus, G.; Beard, J.; Connor, J.R. Effect of manipulation of iron storage, transport, or availability on myelin composition and brain iron content in three different animal models. J. Neurosci. Res. 2004, 77, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Kursula, P.; Meriläinen, G.; Lehto, V.P.; Heape, A.M. The small myelin-associated glycoprotein is a zinc-binding protein. J. Neurochem. 1999, 73, 2110–2118. [Google Scholar] [PubMed]
- Hametner, S.; Dal Bianco, A.; Trattnig, S.; Lassmann, H. Iron related changes in MS lesions and their validity to characterize MS lesion types and dynamics with Ultra-high field magnetic resonance imaging. Brain Pathol. 2018, 28, 743–749. [Google Scholar] [CrossRef] [Green Version]
- Connor, J.R.; Menzies, S.L. Cellular management of iron in the brain. J. Neurol. Sci. 1995, 134, 33–44. [Google Scholar] [CrossRef]
- Gaier, E.D.; Eipper, B.A.; Mains, R.E. Copper signaling in the mammalian nervous system: Synaptic effects. J. Neurosci. Res. 2013, 91, 2–19. [Google Scholar] [CrossRef] [Green Version]
- Lutsenko, S.; Bhattacharjee, A.; Hubbard, A.L. Copper handling machinery of the brain. Metallomics 2010, 2, 596. [Google Scholar] [CrossRef]
- Opazo, C.M.; Greenough, M.A.; Bush, A.I. Copper: From neurotransmission to neuroproteostasis. Front. Aging Neurosci. 2014, 6, 143. [Google Scholar] [CrossRef] [Green Version]
- Aschner, M. Manganese Homeostasis in the CNS. Environ. Res. 1999, 80, 105–109. [Google Scholar] [CrossRef]
- Kirkley, K.S.; Popichak, K.A.; Afzali, M.F.; Legare, M.E.; Tjalkens, R.B. Microglia amplify inflammatory activation of astrocytes in manganese neurotoxicity. J. Neuroinflam. 2017, 14, 99. [Google Scholar] [CrossRef] [PubMed]
- Tjalkens, R.B.; Popichak, K.A.; Kirkley, K.A. Inflammatory Activation of Microglia and Astrocytes in Manganese Neurotoxicity. Adv. Neurobiol. 2017, 18, 159–181. [Google Scholar] [PubMed]
- Takeda, A. Movement of zinc and its functional significance in the brain. Brain Res. Rev. 2000, 34, 137–148. [Google Scholar] [CrossRef]
- Ibs, K.-H.; Rink, L. Zinc-Altered Immune function. J. Nutr. 2003, 133, 1452S–1456S. [Google Scholar] [CrossRef]
- Mohammadi, E.; Qujeq, D.; Taheri, H.; Hajian-Tilaki, K. Evaluation of Serum Trace Element Levels and Superoxide Dismutase Activity in Patients with Inflammatory Bowel Disease: Translating Basic Research into Clinical Application. Biol. Trace Element Res. 2017, 177, 235–240. [Google Scholar] [CrossRef]
- Dean, K.M.; Qin, Y.; Palmer, A.E. Visualizing metal ions in cells: An overview of analytical techniques, approaches, and probes. Biochim. Biophys. Acta (BBA) Bioenerg. 2012, 1823, 1406–1415. [Google Scholar] [CrossRef] [Green Version]
- Krężel, A.; Maret, W. The biological inorganic chemistry of zinc ions. Arch. Biochem. Biophys. 2016, 611, 3–19. [Google Scholar] [CrossRef] [Green Version]
- Outten, F.W.; Twining, B.S.; Begley, T.P. Metal Homeostasis. In Wiley Encyclopedia of Chemical Biology; Wiley: Hoboken, NJ, USA, 2008; p. 324. [Google Scholar]
- Martinez-Finley, E.J.; Chakraborty, S.; Fretham, S.J.B.; Aschner, M. Cellular transport and homeostasis of essential and nonessential metals. Metallomics 2012, 4, 593. [Google Scholar] [CrossRef] [Green Version]
- Skjørringe, T.; Møller, L.B.; Moos, T. Impairment of Interrelated Iron- and Copper Homeostatic Mechanisms in Brain Contributes to the Pathogenesis of Neurodegenerative Disorders. Front. Pharmacol. 2012, 3, 169. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.-L.; Fan, Y.-G.; Yang, Z.-S.; Wang, Z.-Y.; Guo, C. Iron and Alzheimer’s Disease: From Pathogenesis to Therapeutic Implications. Front. Neurosci. 2018, 12, 632. [Google Scholar] [CrossRef] [Green Version]
- Takeda, A. Zinc homeostasis and functions in the brain. BioMetals 2001, 14, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Mocchegiani, E.; Giacconi, R.; Cipriano, C.; Muzzioli, M.; Fattoretti, P.; Bertoni-Freddari, C.; Isani, G.; Zambenedetti, P.; Zatta, P. Zinc-bound metallothioneins as potential biological markers of ageing. Brain Res. Bull. 2001, 55, 147–153. [Google Scholar] [CrossRef]
- Vašák, M.; Meloni, G. Mammalian Metallothionein-3: New Functional and Structural Insights. Int. J. Mol. Sci. 2017, 18, 1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liuzzi, J.P.; Cousins, R.J. Mammalian zinc transporters. Annu. Rev. Nutr. 2004, 24, 151–172. [Google Scholar] [CrossRef] [PubMed]
- Kambe, T.; Tsuji, T.; Hashimoto, A.; Itsumura, N. The Physiological, Biochemical, and Molecular Roles of Zinc Transporters in Zinc Homeostasis and Metabolism. Physiol. Rev. 2015, 95, 749–784. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, P.; Vergnano, A.M.; Barbour, B.; Casado, M. Zinc at glutamatergic synapses. Neuroscience 2009, 158, 126–136. [Google Scholar] [CrossRef]
- Radford, R.J.; Lippard, S.J. Chelators for investigating zinc metalloneurochemistry. Curr. Opin. Chem. Biol. 2013, 17, 129–136. [Google Scholar] [CrossRef]
- Grochowski, C.; Blicharska, E.; Krukow, P.; Jonak, K.; Maciejewski, M.; Szczepanek, D.; Jonak, K.; Flieger, J.; Maciejewski, R. Analysis of Trace Elements in Human Brain: Its Aim, Methods, and Concentration Levels. Front. Chem. 2019, 7, 115. [Google Scholar] [CrossRef] [Green Version]
- Krebs, N.; Langkammer, C.; Goessler, W.; Ropele, S.; Fazekas, F.; Yen, K.; Scheurer, E. Assessment of trace elements in human brain using inductively coupled plasma mass spectrometry. J. Trace Elem. Med. Biol. 2014, 28, 1–7. [Google Scholar] [CrossRef]
- Markesbery, W.R.; Ehmann, W.D.; Alauddin, M.; Hossain, T.I.M. Brain trace element concentrations in aging. Neurobiol. Aging 1984, 5, 19–28. [Google Scholar] [CrossRef]
- Connor, J.R.; Menzies, S.L.; Martin, S.S.; Mufson, E.J. Cellular distribution of transferrin, ferritin, and iron in normal and aged human brains. J. Neurosci. Res. 1990, 27, 595–611. [Google Scholar] [CrossRef] [PubMed]
- Dringen, R.; Bishop, G.M.; Koeppe, M.; Dang, T.N.; Robinson, S.R. The Pivotal Role of Astrocytes in the Metabolism of Iron in the Brain. Neurochem. Res. 2007, 32, 1884–1890. [Google Scholar] [CrossRef] [PubMed]
- Harrison, W.W.; Netsky, M.G.; Brown, M.D. Trace elements in human brain: Copper, zinc, iron, and magnesium. Clin. Chim. Acta 1968, 21, 55–60. [Google Scholar] [CrossRef]
- Hare, D.J.; Lee, J.K.; Beavis, A.D.; van Gramberg, A.; George, J.; Adlard, P.A.; Finkelstein, D.I.; Doble, P.A. Three-Dimensional Atlas of Iron, Copper, and Zinc in the Mouse Cerebrum and Brainstem. Anal. Chem. 2012, 84, 3990–3997. [Google Scholar] [CrossRef] [PubMed]
- Duflou, H.; Maenhaut, W.; De Reuck, J. Regional distribution of potassium, calcium, and six trace elements in normal human brain. Neurochem. Res. 1989, 14, 1099–1112. [Google Scholar] [CrossRef]
- Gh Popescu, B.F.; George, M.J.; Bergmann, U.; Garachtchenko, A.V.; Kelly, M.E.; McCrea, R.P.E.; Lüning, K.; Devon, R.M.; George, G.N.; Hanson, A.D.; et al. Mapping metals in Parkinson’s and normal brain using rapid-scanning x-ray fluorescence. Phys. Med. Biol. 2009, 54, 651–663. [Google Scholar] [CrossRef]
- Dobrowolska, J.; Dehnhardt, M.; Matusch, A.; Zoriy, M.; Palomero-Gallagher, N.; Koscielniak, P.; Zilles, K.; Becker, J.S. Quantitative imaging of zinc, copper and lead in three distinct regions of the human brain by laser ablation inductively coupled plasma mass spectrometry. Talanta 2008, 74, 717–723. [Google Scholar] [CrossRef]
- Popescu, B.F.G.H.; Robinson, C.A.; Chapman, L.D.; Nichol, H. Synchrotron X-ray Fluorescence Reveals Abnormal Metal Distributions in Brain and Spinal Cord in Spinocerebellar Ataxia: A Case Report. Cerebellum 2009, 8, 340–351. [Google Scholar] [CrossRef]
- Popescu, B.F.G.H.; Robinson, C.A.; Rajput, A.; Rajput, A.H.; Harder, S.L.; Nichol, H. Iron, Copper, and Zinc Distribution of the Cerebellum. Cerebellum 2009, 8, 74–79. [Google Scholar] [CrossRef]
- Goldberg, W.J.; Allen, N. Determination of Cu, Mn, Fe, and Ca in six regions of normal human brain, by atomic absorption spectroscopy. Clin. Chem. 1981, 27, 562–564. [Google Scholar] [CrossRef]
- Warren, P.J.; Earl, C.J.; Thompson, R.H.S. The distribution of copper in human brain. Brain 1960, 83, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Cuajungco, M.P.; Lees, G.J. Zinc Metabolism in the Brain: Relevance to Human Neurodegenerative Disorders. Neurobiol. Dis. 1997, 4, 137–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mocchegiani, E.; Bertoni-Freddari, C.; Marcellini, F.; Malavolta, M. Brain, aging and neurodegeneration: Role of zinc ion availability. Prog. Neurobiol. 2005, 75, 367–390. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Finley, E.J.; Gavin, C.E.; Aschner, M.; Gunter, T.E. Manganese neurotoxicity and the role of reactive oxygen species. Free Radic. Biol. Med. 2013, 62, 65–75. [Google Scholar] [CrossRef] [Green Version]
- Davies, K.M.; Bohic, S.; Carmona, A.; Ortega, R.; Cottam, V.; Hare, D.J.; Finberg, J.P.; Reyes, S.; Halliday, G.M.; Mercer, J.F.; et al. Copper pathology in vulnerable brain regions in Parkinson’s disease. Neurobiol. Aging 2014, 35, 858–866. [Google Scholar] [CrossRef] [Green Version]
- Hung, Y.H.; Bush, A.I.; Cherny, R.A. Copper in the brain and Alzheimer’s disease. JBIC J. Biol. Inorg. Chem. 2010, 15, 61–76. [Google Scholar] [CrossRef]
- Koeppen, A.H.; Ramirez, R.L.; Yu, D.; Collins, S.E.; Qian, J.; Parsons, P.J.; Yang, K.X.; Chen, Z.; Mazurkiewicz, J.E.; Feustel, P.J. Friedreich’s Ataxia Causes Redistribution of Iron, Copper, and Zinc in the Dentate Nucleus. Cerebellum 2012, 11, 845–860. [Google Scholar] [CrossRef] [Green Version]
- Bourassa, M.W.; Miller, L.M. Metal imaging in neurodegenerative diseases. Metallomics 2012, 4, 721. [Google Scholar] [CrossRef] [Green Version]
- Kwakye, G.; Paoliello, M.; Mukhopadhyay, S.; Bowman, A.; Aschner, M. Manganese-Induced Parkinsonism and Parkinson’s Disease: Shared and Distinguishable Features. Int. J. Environ. Res. Public Health 2015, 12, 7519–7540. [Google Scholar] [CrossRef] [Green Version]
- Chtourou, Y.; Trabelsi, K.; Fetoui, H.; Mkannez, G.; Kallel, H.; Zeghal, N. Manganese Induces Oxidative Stress, Redox State Unbalance and Disrupts Membrane Bound ATPases on Murine Neuroblastoma Cells In Vitro: Protective Role of Silymarin. Neurochem. Res. 2011, 36, 1546–1557. [Google Scholar] [CrossRef] [Green Version]
- Kwik-Uribe, C.; Smith, D.R. Temporal responses in the disruption of iron regulation by manganese. J. Neurosci. Res. 2006, 83, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Fitsanakis, V.A.; Au, C.; Erikson, K.M.; Aschner, M. The effects of manganese on glutamate, dopamine and γ-aminobutyric acid regulation. Neurochem. Int. 2006, 48, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Tamm, C.; Sabri, F.; Ceccatelli, S. Mitochondrial-Mediated Apoptosis in Neural Stem Cells Exposed to Manganese. Toxicol. Sci. 2008, 101, 310–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricchelli, F.; Fusi, P.; Tortora, P.; Valtorta, M.; Riva, M.; Tognon, G.; Chieregato, K.; Bolognin, S.; Zatta, P. Destabilization of non-pathological variants of ataxin-3 by metal ions results in aggregation/fibrillogenesis. Int. J. Biochem. Cell Biol. 2007, 39, 966–977. [Google Scholar] [CrossRef]
- Bush, A. Metals and neuroscience. Curr. Opin. Chem. Biol. 2000, 4, 184–191. [Google Scholar] [CrossRef]
- Molina-Holgado, F.; Hider, R.C.; Gaeta, A.; Williams, R.; Francis, P. Metals ions and neurodegeneration. BioMetals 2007, 20, 639–654. [Google Scholar] [CrossRef]
- Sayre, L.; Smith, M.; Perry, G. Chemistry and Biochemistry of Oxidative Stress in Neurodegenerative Disease. Curr. Med. Chem. 2001, 8, 721–738. [Google Scholar] [CrossRef]
- Fridovich, I. Fundamental Aspects of Reactive Oxygen Species, or What’s the Matter with Oxygen? Ann. N. Y. Acad. Sci. 1999, 893, 13–18. [Google Scholar] [CrossRef]
- Valko, M.; Rhodes, C.J.; Moncol, J.; Izakovic, M.; Mazur, M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem. Biol. Interact. 2006, 160, 1–40. [Google Scholar] [CrossRef]
- Lehmann, I.; Sack, U.; Lehmann, J. Metal ions affecting the immune system. Met. Ions Life Sci. 2011, 8, 157–185. [Google Scholar]
- Rossi-George, A.; Guo, C.-J.; Oakes, B.L.; Gow, A.J. Copper modulates the phenotypic response of activated BV2 microglia through the release of nitric oxide. Nitric Oxide 2012, 27, 201–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossi-George, A.; Guo, C.-J. Copper disrupts S-nitrosothiol signaling in activated BV2 microglia. Neurochem. Int. 2016, 99, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Roberts, B.R.; Ryan, T.M.; Bush, A.I.; Masters, C.L.; Duce, J.A. The role of metallobiology and amyloid-β peptides in Alzheimer’s disease: Metal ions, Aβ dimers and Alzheimer’s disease. J. Neurochem. 2012, 120, 149–166. [Google Scholar] [CrossRef] [PubMed]
- Lovell, M.A.; Robertson, J.D.; Teesdale, W.J.; Campbell, J.L.; Markesbery, W.R. Copper, iron and zinc in Alzheimer’s disease senile plaques. J. Neurol. Sci. 1998, 158, 47–52. [Google Scholar] [CrossRef]
- Leskovjan, A.C.; Lanzirotti, A.; Miller, L.M. Amyloid plaques in PSAPP mice bind less metal than plaques in human Alzheimer’s disease. NeuroImage 2009, 47, 1215–1220. [Google Scholar] [CrossRef] [Green Version]
- Guilloreau, L.; Combalbert, S.; Sournia-Saquet, A.; Mazarguil, H.; Faller, P. Redox Chemistry of Copper–Amyloid-β: The Generation of Hydroxyl Radical in the Presence of Ascorbate is Linked to Redox-Potentials and Aggregation State. ChemBioChem 2007, 8, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.C.; Nam, E.; Lee, H.J.; Savelieff, M.G.; Lim, M.H. Towards an understanding of amyloid-β oligomers: Characterization, toxicity mechanisms, and inhibitors. Chem. Soc. Rev. 2017, 46, 310–323. [Google Scholar] [CrossRef]
- Rajan, M.T.; Rao, K.J.; Mamatha, B.M.; Rao, R.V.; Shanmugavelu, P.; Menon, R.B.; Pavithran, M.V. Quantification of trace elements in normal human brain by inductively coupled plasma atomic emission spectrometry. J. Neurol. Sci. 1997, 146, 153–166. [Google Scholar] [CrossRef]
- Cvetkovic, A.; Menon, A.L.; Thorgersen, M.P.; Scott, J.W.; Poole, F.L., II; Jenney, F.E., Jr.; Lancaster, W.A.; Praissman, J.L.; Shanmukh, S.; Vaccaro, B.J.; et al. Microbial metalloproteomes are largely uncharacterized. Nature 2010, 466, 779–782. [Google Scholar] [CrossRef]
- Ng, E.; Lind, P.M.; Lindgren, C.; Ingelsson, E.; Mahajan, A.; Morris, A.; Lind, L. Genome-wide association study of toxic metals and trace elements reveals novel associations. Hum. Mol. Genet. 2015, 24, 4739–4745. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.K.; Goloubinoff, P.; Christen, P. Non-native Proteins as Newly-Identified Targets of Heavy Metals and Metalloids. In Cellular Effects of Heavy Metals; Banfalvi, G., Ed.; Springer: Dordrecht, The Netherlands, 2011; pp. 263–274. [Google Scholar]
- Kern, M.; Wisniewski, M.; Cabell, L.; Audesirk, G. Inorganic lead and calcium interact positively in activation of calmodulin. Neurotoxicology 2000, 21, 353–363. [Google Scholar] [PubMed]
- Bánfalvi, G. Heavy Metals, Trace Elements and Their Cellular Effects. In Cellular Effects of Heavy Metals; Banfalvi, G., Ed.; Springer: Dordrecht, The Netherlands, 2011; pp. 3–28. [Google Scholar]
- Nuran Ercal, B.S.P.; Hande Gurer-Orhan, B.S.P.; Nukhet Aykin-Burns, B.S.P. Toxic Metals and Oxidative Stress Part I: Mechanisms Involved in Me-tal induced Oxidative Damage. Curr. Top. Med. Chem. 2001, 1, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Aschner, M.; Aschner, J.L. Mercury neurotoxicity: Mechanisms of blood-brain barrier transport. Neurosci. Biobehav. Rev. 1990, 14, 169–176. [Google Scholar] [CrossRef]
- Kerper, L.E.; Ballatori, N.; Clarkson, T.W. Methylmercury transport across the blood-brain barrier by an amino acid carrier. Am. J. Physiol. Integr. Comp. Physiol. 1992, 262, R761–R765. [Google Scholar] [CrossRef]
- Wagner, C.; Sudati, J.H.; Nogueira, C.W.; Rocha, J.B.T. In vivo and in vitro inhibition of mice thioredoxin reductase by methylmercury. BioMetals 2010, 23, 1171–1177. [Google Scholar] [CrossRef]
- Ruipérez, F.; Mujika, J.I.; Ugalde, J.M.; Exley, C.; Lopez, X. Pro-oxidant activity of aluminum: Promoting the Fenton reaction by reducing Fe(III) to Fe(II). J. Inorg. Biochem. 2012, 117, 118–123. [Google Scholar] [CrossRef]
- Yokel, R.A. Blood-brain barrier flux of aluminum, manganese, iron and other metals suspected to contribute to metal-induced neurodegeneration. J. Alzheimers Dis. 2006, 10, 223–253. [Google Scholar] [CrossRef]
- Exley, C. Human exposure to aluminium. Environ. Sci. Process Impacts 2013, 15, 1807–1816. [Google Scholar] [CrossRef] [Green Version]
- Ward, R.J.; Zhang, Y.; Crichton, R.R. Aluminium toxicity and iron homeostasis. J. Inorg. Biochem. 2001, 87, 9–14. [Google Scholar] [CrossRef]
- Oteiza, P.I. A Mechanism for the Stimulatory Effect of Aluminum on Iron-Induced Lipid Peroxidation. Arch. Biochem. Biophys. 1994, 308, 374–379. [Google Scholar] [CrossRef]
- Yamanaka, K.; Minato, N.; Iwai, K. Stabilization of iron regulatory protein 2, IRP2, by aluminum. FEBS Lett. 1999, 462, 216–220. [Google Scholar] [CrossRef] [Green Version]
- Van Landeghem, G.F.; D’Haese, P.C.; Lamberts, L.V.; De Broe, M.E. Competition of iron and aluminum for transferrin: The molecular basis for aluminum deposition in iron-overloaded dialysis patients? Exp. Nephrol. 1997, 5, 239–245. [Google Scholar] [PubMed]
- Wu, Z.; Du, Y.; Xue, H.; Wu, Y.; Zhou, B. Aluminum induces neurodegeneration and its toxicity arises from increased iron accumulation and reactive oxygen species (ROS) production. Neurobiol. Aging 2012, 33, e1–e199. [Google Scholar] [CrossRef] [PubMed]
- Guo, G.-W.; Liang, Y.-X. Aluminum-induced apoptosis in cultured astrocytes and its effect on calcium homeostasis. Brain Res. 2001, 888, 221–226. [Google Scholar] [CrossRef]
- Canales, J.J.; Corbalán, R.; Montoliu, C.; Llansola, M.; Monfort, P.; Erceg, S.; Hernandez-Viadel, M.; Felipo, V. Aluminium impairs the glutamate-nitric oxide-cGMP pathway in cultured neurons and in rat brain in vivo: Molecular mechanisms and implications for neuropathology. J. Inorg. Biochem. 2001, 87, 63–69. [Google Scholar] [CrossRef]
- Banks, W.A.; Kastin, A.J. The aluminum-induced increase in blood-brain barrier permeability to delta-sleep-inducing peptide occurs throughout the brain and is independent of phosphorus and acetylcholinesterase levels. Psychopharmacology 1985, 86, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Nehru, B.; Bhalla, P. Reversal of an aluminium induced alteration in redox status in different regions of rat brain by administration of centrophenoxine. Mol. Cell. Biochem. 2006, 290, 185–191. [Google Scholar] [CrossRef]
- Sumathi, T.; Shobana, C.; Thangarajeswari, M.; Usha, R. Protective effect of L-Theanine against aluminium induced neurotoxicity in cerebral cortex, hippocampus and cerebellum of rat brain—Histopathological, and biochemical approach. Drug Chem. Toxicol. 2014, 38, 22–31. [Google Scholar] [CrossRef]
- Kumar, V.; Gill, K.D. Oxidative stress and mitochondrial dysfunction in aluminium neurotoxicity and its amelioration: A review. NeuroToxicology 2014, 41, 154–166. [Google Scholar] [CrossRef]
- Zaky, A.; Mohammad, B.; Moftah, M.Z.; Kandeel, K.M.; Bassiouny, A.R. Apurinic/apyrimidinic endonuclease 1 is a key modulator of aluminum-induced neuroinflammation. BMC Neurosci. 2013, 14, 26. [Google Scholar] [CrossRef] [Green Version]
- Corrigan, F.M.; Reynolds, G.P.; Ward, N.I. Hippocampal tin, aluminum and zinc in Alzheimer’s disease. BioMetals 1993, 6, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wei, X.; Yang, J.; Suo, J.; Chen, J.; Liu, X.; Zhao, X. Chronic exposure to aluminum and risk of Alzheimer’s disease: A meta-analysis. Neurosci. Lett. 2016, 610, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Maret, W. 1. The Bioinorganic Chemistry of Lead in the Context of Its Toxicity. In Lead—Its Effects on Environment and Health; Sigel, A., Sigel, H., Sigel, R.K.O., Eds.; De Gruyter: Berlin, Germany; Boston, MA, USA, 2017; pp. 1–20. [Google Scholar]
- Farkas, E.; Buglyó, P. Lead(II) Complexes of Amino Acids, Peptides, and Other Related Ligands of Biological Interest. In Lead—Its Effects on Environment and Health; Sigel, A., Sigel, H., Sigel, R.K.O., Eds.; De Gruyter: Berlin, Germany; Boston, MA, USA, 2017. [Google Scholar]
- Ahamed, M.; Siddiqui, M.K.J. Low level lead exposure and oxidative stress: Current opinions. Clin. Chim. Acta 2007, 383, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Maret, W.; Moulis, J.-M. The Bioinorganic Chemistry of Cadmium in the Context of Its Toxicity. In Metal Ions in Life Sciences; Springer: Dordrecht, The Netherlands, 2012; Volume 11, pp. 1–29. [Google Scholar]
- Mesna, O.J.; Steffensen, I.-L.; Hjertholm, H.; Andersen, R.A. Accumulation of metallothionein and its multiple forms by zinc, cadmium and dexamethasone in human peripheral T and B lymphocytes and monocytes. Chem. Biol. Interact. 1995, 94, 225–242. [Google Scholar] [CrossRef]
- Krężel, A.; Maret, W. The Functions of Metamorphic Metallothioneins in Zinc and Copper Metabolism. Int. J. Mol. Sci. 2017, 18, 1237. [Google Scholar] [CrossRef] [Green Version]
- Peiser, M.; Tralau, T.; Heidler, J.; Api, A.M.; Arts, J.H.E.; Basketter, D.A.; English, J.; Diepgen, T.L.; Fuhlbrigge, R.C.; Gaspari, A.A.; et al. Allergic contact dermatitis: Epidemiology, molecular mechanisms, in vitro methods and regulatory aspects: Current knowledge assembled at an international workshop at BfR, Germany. Cell Mol. Life Sci. 2012, 69, 763–781. [Google Scholar] [CrossRef] [Green Version]
- Corsini, E.; Oukka, M.; Pieters, R.; Kerkvliet, N.I.; Ponce, R.; Germolec, D.R. Alterations in regulatory T-cells: Rediscovered pathways in immunotoxicology. J. Immunotoxicol. 2011, 8, 251–257. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, D.A.; McCabe, M.J. Immunomodulation by metals. Int. Immunopharmacol. 2002, 2, 293–302. [Google Scholar] [CrossRef]
- Hemdan, N.Y.A.; Emmrich, F.; Adham, K.; Wichmann, G.; Lehmann, I.; El-Massry, A.; Ghoneim, H.; Lehmann, J.; Sack, U. Dose-Dependent Modulation of the In Vitro Cytokine Production of Human Immune Competent Cells by Lead Salts. Toxicol. Sci. 2005, 86, 75–83. [Google Scholar] [CrossRef] [Green Version]
- Hemdan, N.Y.A.; Emmrich, F.; Sack, U.; Wichmann, G.; Lehmann, J.; Adham, K.; Lehmann, I. The in vitro immune modulation by cadmium depends on the way of cell activation. Toxicology 2006, 222, 37–45. [Google Scholar] [CrossRef]
- Hemdan, N.Y.A.; Lehmann, I.; Wichmann, G.; Lehmann, J.; Emmrich, F.; Sack, U. Immunomodulation by mercuric chloride in vitro: Application of different cell activation pathways. Clin. Exp. Immunol. 2007, 148, 325–337. [Google Scholar] [CrossRef]
- Mandelbrote, B.M.; Stanier, M.W.; Thompson, R.H.S.; Thruston, M.N. Studies on copper metabolism in demyelinating diseases of the central nervous system. Brain 1948, 71, 212–228. [Google Scholar] [CrossRef] [PubMed]
- Tamburo, E.; Varrica, D.; Dongarrà, G.; Grimaldi, L.M.E. Trace Elements in Scalp Hair Samples from Patients with Relapsing-Remitting Multiple Sclerosis. PLoS ONE 2015, 10, e0122142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giacoppo, S.; Galuppo, M.; Calabrò, R.S.; D’Aleo, G.; Marra, A.; Sessa, E.; Bua, D.G.; Potorti, A.G.; Dugo, G.; Bramanti, P.; et al. Heavy Metals and Neurodegenerative Diseases: An Observational Study. Biol. Trace Elem. Res. 2014, 161, 151–160. [Google Scholar] [CrossRef] [PubMed]
- Palm, R.; Hallmans, G. Zinc and copper in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1982, 45, 691–698. [Google Scholar] [CrossRef] [Green Version]
- Pawlitzki, M.; Uebelhör, J.; Sweeney-Reed, C.; Stephanik, H.; Hoffmann, J.; Lux, A.; Reinhold, D. Lower Serum Zinc Levels in Patients with Multiple Sclerosis Compared to Healthy Controls. Nutrients 2018, 10, 967. [Google Scholar] [CrossRef] [Green Version]
- Nasrabadi, M.N.; Forghani, D.; Shahabi, I.; Shirini, R. Determination of trace elements in blood samples of patients affected by multiple sclerosis from Iran by neutron activation analysis. J. Radioanal. Nucl. Chem. 2012, 293, 479–482. [Google Scholar] [CrossRef]
- De Riccardis, L.; Buccolieri, A.; Muci, M.; Pitotti, E.; De Robertis, F.; Trianni, G.; Manno, D.; Maffia, M. Copper and ceruloplasmin dyshomeostasis in serum and cerebrospinal fluid of multiple sclerosis subjects. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2018, 1864, 1828–1838. [Google Scholar] [CrossRef]
- Ghazavi, A.; Kianbakht, S.; Ghasami, K.; Mosayebi, G. High copper and low zinc serum levels in Iranian patients with multiple sclerosis: A case control study. Clin. Lab. 2012, 58, 161–164. [Google Scholar]
- Juybari, K.B.; Ebrahimi, G.; Momeni Moghaddam, M.A.; Asadikaram, G.; Torkzadeh-Mahani, M.; Akbari, M.; Mirzamohammadi, S.; Karimi, A.; Nematollahi, M.H. Evaluation of serum arsenic and its effects on antioxidant alterations in relapsing-remitting multiple sclerosis patients. Mult. Scler. Relat. Disord. 2018, 19, 79–84. [Google Scholar] [CrossRef]
- Dehghanifiroozabadi, M.; Noferesti, P.; Amirabadizadeh, A.; Nakhaee, S.; Aaseth, J.; Noorbakhsh, F.; Mehrpour, O. Blood lead levels and multiple sclerosis: A case-control study. Mult. Scler. Relat. Disord. 2019, 27, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Attar, A.M.; Kharkhaneh, A.; Etemadifar, M.; Keyhanian, K.; Davoudi, V.; Saadatnia, M. Serum Mercury Level and Multiple Sclerosis. Biol. Trace. Elem. Res. 2012, 146, 150–153. [Google Scholar] [CrossRef]
- Alimonti, A.; Ristori, G.; Giubilei, F.; Stazi, M.A.; Pino, A.; Visconti, A.; Brescianini, S.; Monti, M.S.; Forte, G.; Stanzione, P.; et al. Serum chemical elements and oxidative status in Alzheimer’s disease, Parkinson disease and multiple sclerosis. NeuroToxicology 2007, 28, 450–456. [Google Scholar] [CrossRef]
- Janghorbani, M.; Shaygannejad, V.; Hakimdavood, M.; Salari, M. Trace Elements in Serum Samples of Patients with Multiple Sclerosis. Athens J. Health 2017, 4, 145–154. [Google Scholar] [CrossRef]
- De Oliveira, M.; Gianeti, T.M.R.; da Rocha, F.C.G.; Lisboa-Filho, P.N.; Piacenti-Silva, M. A preliminary study of the concentration of metallic elements in the blood of patients with multiple sclerosis as measured by ICP-MS. Sci. Rep. 2020, 10, 13112. [Google Scholar] [CrossRef] [PubMed]
- Siotto, M.; Filippi, M.M.; Simonelli, I.; Landi, D.; Ghazaryan, A.; Vollaro, S.; Ventriglia, M.; Pasqualetti, P.; Rongioletti, M.C.A.; Squitti, R.; et al. Oxidative Stress Related to Iron Metabolism in Relapsing Remitting Multiple Sclerosis Patients With Low Disability. Front. Neurosci. 2019, 13, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popescu, B.F.; Frischer, J.M.; Webb, S.M.; Tham, M.; Adiele, R.C.; Robinson, C.A.; Fitz-Gibbon, P.D.; Weigand, S.D.; Metz, I.; Nehzati, S.; et al. Pathogenic implications of distinct patterns of iron and zinc in chronic MS lesions. Acta Neuropathol. 2017, 134, 45–64. [Google Scholar] [CrossRef] [Green Version]
- Yao, B.; Hametner, S.; van Gelderen, P.; Merkle, H.; Chen, C.; Lassmann, H.; Duyn, J.H.; Bagnato, F. 7 Tesla Magnetic Resonance Imaging to Detect Cortical Pathology in Multiple Sclerosis. PLoS ONE 2014, 9, e108863. [Google Scholar] [CrossRef] [Green Version]
- Khalil, M.; Langkammer, C.; Pichler, A.; Pinter, D.; Gattringer, T.; Bachmaier, G.; Ropele, S.; Fuchs, S.; Enzinger, C.; Fazekas, F. Dynamics of brain iron levels in multiple sclerosis: A longitudinal 3T MRI study. Neurology 2015, 84, 2396–2402. [Google Scholar] [CrossRef]
- Stephenson, E.; Nathoo, N.; Mahjoub, Y.; Dunn, J.F.; Yong, V.W. Iron in multiple sclerosis: Roles in neurodegeneration and repair. Nat. Rev. Neurol. 2014, 10, 459–468. [Google Scholar] [CrossRef]
- Bagnato, F.; Hametner, S.; Welch, E.B. Visualizing iron in multiple sclerosis. Magn. Reason. Imaging 2013, 31, 376–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dal-Bianco, A.; Grabner, G.; Kronnerwetter, C.; Weber, M.; Höftberger, R.; Berger, T.; Auff, E.; Leutmezer, F.; Trattnig, S.; Lassmann, H.; et al. Slow expansion of multiple sclerosis iron rim lesions: Pathology and 7 T magnetic resonance imaging. Acta Neuropathol. 2017, 133, 25–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bagnato, F.; Hametner, S.; Yao, B.; van Gelderen, P.; Merkle, H.; Cantor, F.K.; Lassmann, H.; Duyn, J.H. Tracking iron in multiple sclerosis: A combined imaging and histopathological study at 7 Tesla. Brain 2011, 134, 3602–3615. [Google Scholar] [CrossRef] [Green Version]
- Magliozzi, R.; Hametner, S.; Facchiano, F.; Marastoni, D.; Rossi, S.; Castellaro, M.; Poli, A.; Lattanzi, F.; Visconti, A.; Nicholas, R. Iron homeostasis, complement, and coagulation cascade as CSF signature of cortical lesions in early multiple sclerosis. Ann. Clin. Transl. Neurol. 2019, 6, 2150–2163. [Google Scholar] [CrossRef] [Green Version]
- Zivadinov, R.; Tavazzi, E.; Bergsland, N.; Hagemeier, J.; Lin, F.; Dwyer, M.G.; Carl, E.; Kolb, C.; Hojnacki, D. Ramasamy, D. Brain Iron at Quantitative MRI Is Associated with Disability in Multiple Sclerosis. Radiology 2018, 289, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Hagemeier, J.; Ramanathan, M.; Schweser, F.; Dwyer, M.G.; Lin, F.; Bergsland, N.; Weinstock-Guttman, B.; Zivadinov, R. Iron-related gene variants and brain iron in multiple sclerosis and healthy individuals. NeuroImage Clin. 2018, 17, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Yasui, M.; Yase, Y.; Ando, K.; Adachi, K.; Mukoyama, M.; Ohsugi, K. Magnesium concentration in brains from multiple sclerosis patients. Acta. Neurol. Scand. 2009, 81, 197–200. [Google Scholar] [CrossRef]
- Melo, T.M.; Larsen, C.; White, L.R.; Aasly, J.; Sjobakk, T.E.; Flaten, T.P.; Sonnewald, U.; Syversen, T. Manganese, Copper, and Zinc in Cerebrospinal Fluid from Patients with Multiple Sclerosis. Biol. Trace Element Res. 2003, 93, 1–8. [Google Scholar] [CrossRef]
- Bredholt, M.; Frederiksen, J.L. Zinc in Multiple Sclerosis: A Systematic Review and Meta-Analysis. ASN Neuro 2016, 8. [Google Scholar] [CrossRef]
- Van Wart, H.E.; Birkedal-Hansen, H. The cysteine switch: A principle of regulation of metalloproteinase activity with potential applicability to the entire matrix metalloproteinase gene family. Proc. Natl. Acad. Sci. USA 1990, 87, 5578–5582. [Google Scholar] [CrossRef] [Green Version]
- Penkowa, M.; Espejo, C.; Ortega-Aznar, A.; Hidalgo, J.; Montalban, X.; Martínez Cáceres, E.M. Metallothionein expression in the central nervous system of multiple sclerosis patients. Cell Mol. Life Sci. 2003, 60, 1258–1266. [Google Scholar] [CrossRef] [PubMed]
- Yong, V.W.; Zabad, R.K.; Agrawal, S.; Goncalves DaSilva, A.; Metz, L.M. Elevation of matrix metalloproteinases (MMPs) in multiple sclerosis and impact of immunomodulators. J. Neurol. Sci. 2007, 259, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Lindberg, R.L.P. The expression profile of matrix metalloproteinases (MMPs) and their inhibitors (TIMPs) in lesions and normal appearing white matter of multiple sclerosis. Brain 2001, 124, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Cossins, J.A.; Clements, J.M.; Ford, J.; Miller, K.M.; Pigott, R.; Vos, W.; Van der Walk, P.; De Groot, C.J. Enhanced expression of MMP-7 and MMP-9 in demyelinating multiple sclerosis lesions. Acta Neuropathol. 1997, 94, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Maeda, A.; Sobel, R.A. Matrix Metalloproteinases in the Normal Human Central Nervous System, Microglial Nodules, and Multiple Sclerosis Lesions. J. Neuropathol. Exp. Neurol. 1996, 55, 300–309. [Google Scholar] [CrossRef] [Green Version]
- Bar-Or, A. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain 2003, 126, 2738–2749. [Google Scholar] [CrossRef] [Green Version]
- Gray, E.; Thomas, T.L.; Betmouni, S.; Scolding, N.; Love, S. Elevated Matrix Metalloproteinase-9 and Degradation of Perineuronal Nets in Cerebrocortical Multiple Sclerosis Plaques. J. Neuropathol. Exp. Neurol. 2008, 67, 888–899. [Google Scholar] [CrossRef] [Green Version]
- Mold, M.; Chmielecka, A.; Rodriguez, M.; Thom, F.; Linhart, C.; King, A.; Exley, C. Aluminium in Brain Tissue in Multiple Sclerosis. Int. J. Environ. Res. Public Health 2018, 15, 1777. [Google Scholar] [CrossRef] [Green Version]
- Linhart, C.; Davidson, D.; Pathmanathan, S.; Kamaladas, T.; Exley, C. Aluminium in Brain Tissue in Non-neurodegenerative/Non-neurodevelopmental Disease: A Comparison with Multiple Sclerosis. Expo Health 2020, 12, 863–868. [Google Scholar] [CrossRef] [Green Version]
- Sensi, S.L.; Granzotto, A.; Siotto, M.; Squitti, R. Copper and Zinc Dysregulation in Alzheimer’s Disease. Trends Pharmacol. Sci. 2018, 39, 1049–1063. [Google Scholar] [CrossRef]
- Pfaender, S.; Grabrucker, A.M. Characterization of biometal profiles in neurological disorders. Metallomics 2014, 6, 960–977. [Google Scholar] [CrossRef] [PubMed]
- Lobinski, R.; Becker, J.S.; Haraguchi, H.; Sarkar, B. Metallomics: Guidelines for terminology and critical evaluation of analytical chemistry approaches (IUPAC Technical Report). Pure Appl. Chem. 2010, 82, 493–504. [Google Scholar] [CrossRef]
- Nakazawa, E.; Ikemoto, T.; Hokura, A.; Terada, Y.; Kunito, T.; Tanabe, S.; Nakai, I. The presence of mercury selenide in various tissues of the striped dolphin: Evidence from μ-XRF-XRD and XAFS analyses. Metallomics 2011, 3, 719. [Google Scholar] [CrossRef] [PubMed]
- Korbas, M.; O’Donoghue, J.L.; Watson, G.E.; Pickering, I.J.; Singh, S.P.; Myers, G.J.; Clarkson, T.W.; George, G.N. The Chemical Nature of Mercury in Human Brain Following Poisoning or Environmental Exposure. ACS. Chem. Neurosci. 2010, 1, 810–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bacquart, T.; Devès, G.; Carmona, A.; Tucoulou, R.; Bohic, S.; Ortega, R. Subcellular Speciation Analysis of Trace Element Oxidation States Using Synchrotron Radiation Micro-X-ray Absorption Near-Edge Structure. Anal. Chem. 2007, 79, 7353–7359. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.J.C.; Milton, M.J.T. Analytical techniques for trace element analysis: An overview. TrAC Trends Anal. Chem. 2005, 24, 266–274. [Google Scholar] [CrossRef]
- Ackerman, C.M.; Lee, S.; Chang, C.J. Analytical Methods for Imaging Metals in Biology: From Transition Metal Metabolism to Transition Metal Signaling. Anal. Chem. 2017, 89, 22–41. [Google Scholar] [CrossRef] [Green Version]
- McRae, R.; Bagchi, P.; Sumalekshmy, S.; Fahrni, C.J. In Situ Imaging of Metals in Cells and Tissues. Chem. Rev. 2009, 109, 4780–4827. [Google Scholar] [CrossRef] [Green Version]
- Stewart, T.J. Across the spectrum: Integrating multidimensional metal analytics for in situ metallomic imaging. Metallomics 2019, 11, 29–49. [Google Scholar] [CrossRef] [Green Version]
- Busser, B.; Moncayo, S.; Coll, J.-L.; Sancey, L.; Motto-Ros, V. Elemental imaging using laser-induced breakdown spectroscopy: A new and promising approach for biological and medical applications. Coord. Chem. Rev. 2018, 358, 70–79. [Google Scholar] [CrossRef]
- Braidy, N.; Poljak, A.; Marjo, C.; Rutlidge, H.; Rich, A.; Jayasena, T.; Inestrosa, N.C.; Sachdev, P. Metal and complementary molecular bioimaging in Alzheimer’s disease. Front. Aging Neurosci. 2014, 6, 138. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.; Cloetens, P.; Devès, G.; Carmona, A.; Bohic, S. Iron Storage within Dopamine Neurovesicles Revealed by Chemical Nano-Imaging. PLoS ONE 2007, 2, e925. [Google Scholar] [CrossRef] [Green Version]
- Keogh, M.J.; Morris, C.M.; Chinnery, P.F. Neuroferritinopathy. Int. Rev. Neurobiol. 2013, 110, 91–123. [Google Scholar] [PubMed]
- Carboni, E.; Nicolas, J.-D.; Töpperwien, M.; Stadelmann-Nessler, C.; Lingor, P.; Salditt, T. Imaging of neuronal tissues by X-ray diffraction and x-ray fluorescence microscopy: Evaluation of contrast and biomarkers for neurodegenerative diseases. Biomed. Opt. Express 2017, 8, 4331. [Google Scholar] [CrossRef] [Green Version]
- Gardner, B.; Dieriks, B.V.; Cameron, S.; Mendis, L.H.S.; Turner, C.; Faull, R.L.M.; Curtis, M.A. Metal concentrations and distributions in the human olfactory bulb in Parkinson’s disease. Sci. Rep. 2017, 7, 10454. [Google Scholar] [CrossRef] [PubMed]
- Portbury, S.; Adlard, P. Zinc Signal in Brain Diseases. Int. J. Mol. Sci. 2017, 18, 2506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weigel, K.J.; Lynch, S.G.; Levine, S.M. Iron Chelation and Multiple Sclerosis. ASN Neuro 2013, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dales, J.-P.; Desplat-Jégo, S. Metal Imbalance in Neurodegenerative Diseases with a Specific Concern to the Brain of Multiple Sclerosis Patients. Int. J. Mol. Sci. 2020, 21, 9105. https://doi.org/10.3390/ijms21239105
Dales J-P, Desplat-Jégo S. Metal Imbalance in Neurodegenerative Diseases with a Specific Concern to the Brain of Multiple Sclerosis Patients. International Journal of Molecular Sciences. 2020; 21(23):9105. https://doi.org/10.3390/ijms21239105
Chicago/Turabian StyleDales, Jean-Philippe, and Sophie Desplat-Jégo. 2020. "Metal Imbalance in Neurodegenerative Diseases with a Specific Concern to the Brain of Multiple Sclerosis Patients" International Journal of Molecular Sciences 21, no. 23: 9105. https://doi.org/10.3390/ijms21239105