The Effects of a Combination of Ion Channel Inhibitors in Female Rats Following Repeated Mild Traumatic Brain Injury
Abstract
:1. Introduction
2. Results
2.1. Behavioural Outcomes
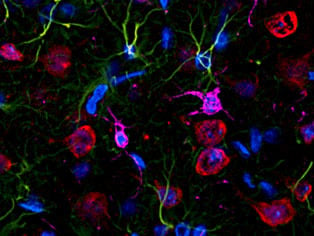
2.2. Cellular Responses
2.3. Oxidative Stress
2.4. Node of Ranvier Integrity
3. Discussion
4. Materials and Methods
4.1. Experimental Model
4.2. Combinatorial Treatment
4.3. Behavioural Assessments
4.4. Immunohistochemistry
4.5. Microscopy and Image Analysis
4.6. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 8OHdG | 8-hydroxy-2′-deoxyguanosine |
| AMPA | α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid |
| BBB | Blood–brain barrier |
| BBG | Brilliant Blue G |
| Caspr | Neurexin IV |
| CNS | Central nervous system |
| GFAP | Glial fibrillary acidic protein |
| Iba1 | Ionised calcium binding molecule 1 |
| ICI | Ion channel inhibitors |
| MnSOD | Manganese superoxide dismutase |
| MWM | Morris water maze |
| mTBI | Mild traumatic brain injury |
| Na+/K+-ATPase | Sodium- and potassium-activated adenosine 5′-triphosphatase |
| NeuN | Neuronal nuclear antigen |
| NMDA | N-methyl-d-aspartate |
| NSS | Neurological severity score |
| oxATP | 5′-triphosphate periodate oxidized sodium salt |
| TBI | Traumatic brain injury |
| rmTBI | Repeated mild traumatic brain injury |
| VGCC | Voltage-gated calcium channels |
References
- Kraus, M.F.; Susmaras, T.; Caughlin, B.P.; Walker, C.J.; Sweeney, J.A.; Little, D.M. White matter integrity and cognition in chronic traumatic brain injury: A diffusion tensor imaging study. Brain 2007, 130, 2508–2519. [Google Scholar] [CrossRef] [PubMed]
- Guskiewicz, K.M.; Marshall, S.W.; Bailes, J.; McCrea, M.; Cantu, R.C.; Randolph, C.; Jordan, B.D. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery 2005, 57, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Rabadi, M.H.; Jordan, B.D. The cumulative effect of repetitive concussion in sports. Clin. J. Sport Med. 2001, 11, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Barkhoudarian, G.; Hovda, D.A.; Giza, C.C. The molecular pathophysiology of concussive brain injury. Clin. Sports Med. 2011, 30, 33–48. [Google Scholar] [CrossRef] [PubMed]
- De Lores Arnaiz, G.R.; Ordieres, M.G.L. Brain Na+, K+-atpase activity in aging and disease. Int. J. Biomed. Sci. 2014, 10, 85–102. [Google Scholar] [PubMed]
- Tang, L.; El-Din, T.M.G.; Payandeh, J.; Martinez, G.Q.; Heard, T.M.; Scheuer, T.; Zheng, N.; Catterall, W.A. Structural basis for Ca2+ selectivity of a voltage-gated calcium channel. Nature 2014, 505, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Stanika, R.I.; Villanueva, I.; Kazanina, G.; Andrews, S.B.; Pivovarova, N.B. Comparative impact of voltage-gated calcium channels and nmda receptors on mitochondria-mediated neuronal injury. J. Neurosci. 2012, 32, 6642–6650. [Google Scholar] [CrossRef] [PubMed]
- Beattie, M.S.; Ferguson, A.R.; Bresnahan, J.C. Ampa-receptor trafficking and injury-induced cell death. Eur. J. Neurosci. 2010, 32, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Gerace, E.; E Pellegrini-Giampietro, D.; Moroni, F.; Mannaioni, G. Poly (ADP-ribose) polymerase 1 (PARP-1) activation and Ca2+ permeable α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) channels in post-ischemic brain damage: New therapeutic opportunities? CNS Neurol. Disord. Drug Targets 2015, 14, 636–646. [Google Scholar] [CrossRef] [PubMed]
- Arbeloa, J.; Pérez-Samartín, A.; Gottlieb, M.; Matute, C. P2X7 receptor blockade prevents ATP excitotoxicity in neurons and reduces brain damage after ischemia. Neurobiol. Dis. 2012, 45, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Domercq, M.; Perez-Samartin, A.; Aparicio, D.; Alberdi, E.; Pampliega, O.; Matute, C. P2X7 receptors mediate ischemic damage to oligodendrocytes. Glia 2010, 58, 730–740. [Google Scholar] [CrossRef] [PubMed]
- Arundine, M.; Tymianski, M. Molecular mechanisms of glutamate-dependent neurodegeneration in ischemia and traumatic brain injury. Cell. Mol. Life Sci. 2004, 61, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, A.; Hovda, D.A.; Kawamata, T.; Katayama, Y.; Becker, D.P. Dynamic changes in local cerebral glucose utilization following cerebral concussion in rats: Evidence of a hyper-and subsequent hypometabolic state. Brain Res. 1991, 561, 106–119. [Google Scholar] [CrossRef]
- Gurkoff, G.; Shahlaie, K.; Lyeth, B.; Berman, R. Voltage-gated calcium channel blockers for the treatment of traumatic brain injury. In New Therapeutics for Traumatic Brain Injury; Elsevier: Amsterdam, The Netherlands, 2017; pp. 179–197. [Google Scholar]
- Kulbe, J.R.; Hill, R.L.; Singh, I.N.; Wang, J.A.; Hall, E.D. Synaptic mitochondria sustain more damage than non-synaptic mitochondria after traumatic brain injury and are protected by cyclosporine A. J. Neurotrauma 2017, 34, 1291–1301. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.; Brustovetsky, T.; Rysted, J.E.; Lin, Z.; Usachev, Y.M.; Brustovetsky, N. Deletion of mitochondrial calcium uniporter incompletely inhibits calcium uptake and induction of the permeability transition pore in brain mitochondria. J. Biol. Chem. 2018, 293, 15652–15663. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Chan, Y.L.; Nguyen, L.T.; Mao, Y.; de Rosa, A.; Beh, I.T.; Chee, C.; Oliver, B.; Herok, G.; Saad, S. Moderate traumatic brain injury is linked to acute behaviour deficits and long term mitochondrial alterations. Clin. Exp. Pharmacol. Physiol. 2016, 43, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Greer, J.E.; Hånell, A.; McGinn, M.J.; Povlishock, J.T. Mild traumatic brain injury in the mouse induces axotomy primarily within the axon initial segment. Acta Neuropathol. 2013, 126, 59–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kane, M.J.; Angoa-Pérez, M.; Briggs, D.I.; Viano, D.C.; Kreipke, C.W.; Kuhn, D.M. A mouse model of human repetitive mild traumatic brain injury. J. Neurosci. Methods 2012, 203, 41–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouzon, B.; Chaytow, H.; Crynen, G.; Bachmeier, C.; Stewart, J.; Mullan, M.; Stewart, W.; Crawford, F. Repetitive mild traumatic brain injury in a mouse model produces learning and memory deficits accompanied by histological changes. J. Neurotrauma 2012, 29, 2761–2773. [Google Scholar] [CrossRef] [PubMed]
- Mouzon, B.C.; Bachmeier, C.; Ferro, A.; Ojo, J.O.; Crynen, G.; Acker, C.M.; Davies, P.; Mullan, M.; Stewart, W.; Crawford, F. Chronic neuropathological and neurobehavioral changes in a repetitive mild traumatic brain injury model. Ann. Neurol. 2014, 75, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Ying, Z.; Gomez-Pinilla, F. Vitamin E protects against oxidative damage and learning disability after mild traumatic brain injury in rats. Neurorehabilit. Neural Repair 2010, 24, 290–298. [Google Scholar]
- Yates, N.J.; Lydiard, S.; Fehily, B.; Weir, G.; Chin, A.; Bartlett, C.A.; Alderson, J.; Fitzgerald, M. Repeated mild traumatic brain injury in female rats increases lipid peroxidation in neurons. Exp. Brain Res. 2017, 235, 2133–2149. [Google Scholar] [CrossRef] [PubMed]
- Facchinetti, F.; Dawson, V.L.; Dawson, T.M. Free radicals as mediators of neuronal injury. Cell. Mol. Neurobiol. 1998, 18, 667–682. [Google Scholar] [CrossRef] [PubMed]
- Tweedie, D.; Fukui, K.; Li, Y.; Yu, Q.-S.; Barak, S.; Tamargo, I.A.; Rubovitch, V.; Holloway, H.W.; Lehrmann, E.; Wood, W.H., III. Cognitive impairments induced by concussive mild traumatic brain injury in mouse are ameliorated by treatment with phenserine via multiple non-cholinergic and cholinergic mechanisms. PLoS ONE 2016, 11, e0156493. [Google Scholar] [CrossRef] [PubMed]
- Huber, B.R.; Meabon, J.S.; Martin, T.J.; Mourad, P.D.; Bennett, R.; Kraemer, B.C.; Cernak, I.; Petrie, E.C.; Emery, M.J.; Swenson, E.R. Blast exposure causes early and persistent aberrant phospho-and cleaved-tau expression in a murine model of mild blast-induced traumatic brain injury. J. Alzheimer’s Dis. 2013, 37, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, T.; Wei, E.P.; Povlishock, J.T. Evidence for the therapeutic efficacy of either mild hypothermia or oxygen radical scavengers after repetitive mild traumatic brain injury. J. Neurotrauma 2014, 31, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, R.; Conti, A.; Graham, D.; Krajewski, S.; Reed, J.; Grady, M.; Trojanowski, J.; McIntosh, T. Mild traumatic brain injury induces apoptotic cell death in the cortex that is preceded by decreases in cellular Bcl-2 immunoreactivity. Neuroscience 2002, 110, 605–616. [Google Scholar] [CrossRef]
- Niogi, S.; Mukherjee, P.; Ghajar, J.; Johnson, C.; Kolster, R.; Sarkar, R.; Lee, H.; Meeker, M.; Zimmerman, R.; Manley, G. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: A 3T diffusion tensor imaging study of mild traumatic brain injury. Am. J. Neuroradiol. 2008, 29, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Mierzwa, A.J.; Marion, C.M.; Sullivan, G.M.; McDaniel, D.P.; Armstrong, R.C. Components of myelin damage and repair in the progression of white matter pathology after mild traumatic brain injury. J. Neuropathol. Exp. Neurol. 2015, 74, 218–232. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Muneer, P.; Schuetz, H.; Wang, F.; Skotak, M.; Jones, J.; Gorantla, S.; Zimmerman, M.C.; Chandra, N.; Haorah, J. Induction of oxidative and nitrosative damage leads to cerebrovascular inflammation in an animal model of mild traumatic brain injury induced by primary blast. Free Radic. Biol. Med. 2013, 60, 282–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.; Chan, Y.L.; Linnane, C.; Mao, Y.; Anwer, A.G.; Sapkota, A.; Annissa, T.F.; Herok, G.; Vissel, B.; Oliver, B.G.; et al. L-carnitine and extendin-4 improve outcomes following moderate brain contusion injury. Sci. Rep. 2018, 8, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Loane, D.J.; Byrnes, K.R. Role of microglia in neurotrauma. Neurotherapeutics 2010, 7, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Mannix, R.; Meehan, W.P.; Mandeville, J.; Grant, P.E.; Gray, T.; Berglass, J.; Zhang, J.; Bryant, J.; Rezaie, S.; Chung, J.Y. Clinical correlates in an experimental model of repetitive mild brain injury. Ann. Neurol. 2013, 74, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Cotrina, M.L.; Lin, J.H.-C.; López-García, J.C.; Naus, C.C.; Nedergaard, M. ATP-mediated glia signaling. J. Neurosci. 2000, 20, 2835–2844. [Google Scholar] [CrossRef] [PubMed]
- O’Hare Doig, R.L.; Bartlett, C.A.; Smith, N.M.; Hodgetts, S.I.; Dunlop, S.A.; Hool, L.; Fitzgerald, M. Specific combinations of ion channel inhibitors reduce excessive Ca2+ influx as a consequence of oxidative stress and increase neuronal and glial cell viability in vitro. Neuroscience 2016, 339, 450–462. [Google Scholar] [CrossRef] [PubMed]
- Yates, N.J.; Giacci, M.K.; Doig, R.L.H.; Chiha, W.; Ashworth, B.E.; Kenna, J.; Bartlett, C.A.; Fitzgerald, M. Delayed treatment of secondary degeneration following acute optic nerve transection using a combination of ion channel inhibitors. Neural Regen. Res. 2017, 12, 307–316. [Google Scholar] [PubMed]
- O’Hare Doig, R.L.; Chiha, W.; Giacci, M.K.; Yates, N.J.; Bartlett, C.A.; Smith, N.M.; Hodgetts, S.I.; Harvey, A.R.; Fitzgerald, M. Specific ion channels contribute to key elements of pathology during secondary degeneration following neurotrauma. BMC Neurosci. 2017, 18, 62. [Google Scholar] [CrossRef] [PubMed]
- Savigni, D.L.; Doig, R.L.H.; Szymanski, C.R.; Bartlett, C.A.; Lozić, I.; Smith, N.M.; Fitzgerald, M. Three Ca2+ channel inhibitors in combination limit chronic secondary degeneration following neurotrauma. Neuropharmacology 2013, 75, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Erlinge, D.; Burnstock, G. P2 receptors in cardiovascular regulation and disease. Purinergic Signal. 2008, 4, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Donnelly-Roberts, D.; Jarvis, M. Discovery of P2X7 receptor-selective antagonists offers new insights into P2X7 receptor function and indicates a role in chronic pain states. Br. J. Pharmacol. 2007, 151, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.-H.; Mackenzie, A.B.; North, R.A.; Surprenant, A. Brilliant blue G selectively blocks ATP-gated rat P2X7 receptors. Mol. Pharmacol. 2000, 58, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Remy, M.; Thaler, S.; Schumann, R.G.; May, C.; Fiedorowicz, M.; Schuettauf, F.; Grüterich, M.; Priglinger, S.G.; Nentwich, M.M.; Kampik, A. An in vivo evaluation of brilliant blue g in animals and humans. Br. J. Ophthalmol. 2008, 92, 1142–1147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolton Hall, A.N.; Joseph, B.; Brelsfoard, J.M.; Saatman, K.E. Repeated closed head injury in mice results in sustained motor and memory deficits and chronic cellular changes. PLoS ONE 2016, 11, e0159442. [Google Scholar] [CrossRef] [PubMed]
- Mychasiuk, R.; Farran, A.; Esser, M.J. Assessment of an experimental rodent model of pediatric mild traumatic brain injury. J. Neurotrauma 2014, 31, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Selwyn, R.G.; Cooney, S.J.; Khayrullina, G.; Hockenbury, N.; Wilson, C.M.; Jaiswal, S.; Bermudez, S.; Armstrong, R.C.; Byrnes, K.R. Outcome after repetitive mild traumatic brain injury is temporally related to glucose uptake profile at time of second injury. J. Neurotrauma 2016, 33, 1479–1491. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.R.; MacFabe, D.F.; Foley, K.A.; Taylor, R.; Cain, D.P. Sub-concussive brain injury in the long-evans rat induces acute neuroinflammation in the absence of behavioral impairments. Behav. Brain Res. 2012, 229, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Valavanidis, A.; Vlachogianni, T.; Fiotakis, C. 8-hydroxy-2′-deoxyguanosine (8-ohdg): A critical biomarker of oxidative stress and carcinogenesis. J. Environ. Sci. Health 2009, 27, 120–139. [Google Scholar] [CrossRef] [PubMed]
- Aucoin, J.-S.; Jiang, P.; Aznavour, N.; Tong, X.-K.; Buttini, M.; Descarries, L.; Hamel, E. Selective cholinergic denervation, independent from oxidative stress, in a mouse model of Alzheimer’s disease. Neuroscience 2005, 132, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, M.; Bartlett, C.A.; Harvey, A.R.; Dunlop, S.A. Early events of secondary degeneration after partial optic nerve transection: An immunohistochemical study. J. Neurotrauma 2010, 27, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Szymanski, C.R.; Chiha, W.; Morellini, N.; Cummins, N.; Bartlett, C.A.; O’Hare Doig, R.L.; Savigni, D.L.; Payne, S.C.; Harvey, A.R.; Dunlop, S.A.; et al. Paranode abnormalities and oxidative stress in optic nerve vulnerable to secondary degeneration: Modulation by 670 nm light treatment. PLoS ONE 2013, 8, e66448. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, T.H.; Reynolds, C.A.; Kumar, R.; Przyklenk, K.; Hüttemann, M. Molecular mechanisms of ischemia–reperfusion injury in brain: Pivotal role of the mitochondrial membrane potential in reactive oxygen species generation. Mol. Neurobiol. 2013, 47, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Zorov, D.B.; Filburn, C.R.; Klotz, L.-O.; Zweier, J.L.; Sollott, S.J. Reactive oxygen species (Ros-induced) ros release: A new phenomenon accompanying induction of the mitochondrial permeability transition in cardiac myocytes. J. Exp. Med. 2000, 192, 1001–1014. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.T.; Beal, M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 2006, 443, 787. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.N.; Kindy, M.S.; Holtsberg, F.W.; Clair, D.K.S.; Yen, H.-C.; Germeyer, A.; Steiner, S.M.; Bruce-Keller, A.J.; Hutchins, J.B.; Mattson, M.P. Mitochondrial manganese superoxide dismutase prevents neural apoptosis and reduces ischemic brain injury: Suppression of peroxynitrite production, lipid peroxidation, and mitochondrial dysfunction. J. Neurosci. 1998, 18, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.H. Reactive oxygen radicals in signaling and damage in the ischemic brain. J. Cereb. Blood Flow Metab. 2001, 21, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Turrens, J.F. Mitochondrial formation of reactive oxygen species. J. Physiol. 2003, 552, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Lyeth, B.; Jenkins, L.; Hamm, R.; Dixon, C.; Phillips, L.; Clifton, G.; Young, H.; Hayes, R. Prolonged memory impairment in the absence of hippocampal cell death following traumatic brain injury in the rat. Brain Res. 1990, 526, 249–258. [Google Scholar] [CrossRef]
- Chakraborti, A.; Allen, A.; Allen, B.; Rosi, S.; Fike, J.R. Cranial irradiation alters dendritic spine density and morphology in the hippocampus. PLoS ONE 2012, 7, e40844. [Google Scholar] [CrossRef] [PubMed]
- Corniola, R.; Zou, Y.; Leu, D.; Fike, J.R.; Huang, T.-T. Paradoxical relationship between Mn superoxide dismutase deficiency and radiation-induced cognitive defects. PLoS ONE 2012, 7, e49367. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Corniola, R.; Leu, D.; Khan, A.; Sahbaie, P.; Chakraborti, A.; Clark, D.J.; Fike, J.R.; Huang, T.-T. Extracellular superoxide dismutase is important for hippocampal neurogenesis and preservation of cognitive functions after irradiation. Proc. Natl. Acad. Sci. USA 2012, 109, 21522–21527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Constantini, S.; Trembovler, V.; Weinstock, M.; Shohami, E. An experimental model of closed head injury in mice: Pathophysiology, histopathology, and cognitive deficits. J. Neurotrauma 1996, 13, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Stahel, P.F.; Shohami, E.; Younis, F.M.; Kariya, K.; Otto, V.I.; Lenzlinger, P.M.; Grosjean, M.B.; Eugster, H.-P.; Trentz, O.; Kossmann, T. Experimental closed head injury: Analysis of neurological outcome, blood–brain barrier dysfunction, intracranial neutrophil infiltration, and neuronal cell death in mice deficient in genes for pro-inflammatory cytokines. J. Cereb. Blood Flow Metab. 2000, 20, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Hinkley, L.B.; Marco, E.J.; Findlay, A.M.; Honma, S.; Jeremy, R.J.; Strominger, Z.; Bukshpun, P.; Wakahiro, M.; Brown, W.S.; Paul, L.K. The role of corpus callosum development in functional connectivity and cognitive processing. PLoS ONE 2012, 7, e39804. [Google Scholar] [CrossRef] [PubMed]
- Loane, D.J.; Kumar, A.; Stoica, B.A.; Cabatbat, R.; Faden, A.I. Progressive neurodegeneration after experimental brain trauma: Association with chronic microglial activation. J. Neuropathol. Exp. Neurol. 2014, 73, 14–29. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.H.; Shin, C.-M.; Kim, M.J.; Cha, C.I. Enhanced expression of L-type Ca2+ channels in reactive astrocytes after ischemic injury in rats. Neurosci. Lett. 2001, 302, 93–96. [Google Scholar] [CrossRef]
- Burgos, M.; Pastor, M.; González, J.; Martinez-Galan, J.; Vaquero, C.; Fradejas, N.; Benavides, A.; Hernández-Guijo, J.; Tranque, P.; Calvo, S. PKCε upregulates voltage-dependent calcium channels in cultured astrocytes. Glia 2007, 55, 1437–1448. [Google Scholar] [CrossRef] [PubMed]
- Le Feuvre, R.; Brough, D.; Rothwell, N. Extracellular atp and P2X7 receptors in neurodegeneration. Eur. J. Pharmacol. 2002, 447, 261–269. [Google Scholar] [CrossRef]
- Pelegrin, P.; Surprenant, A. Pannexin-1 mediates large pore formation and interleukin-1β release by the ATP-gated P2X7 receptor. EMBO J. 2006, 25, 5071–5082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davalos, D.; Grutzendler, J.; Yang, G.; Kim, J.V.; Zuo, Y.; Jung, S.; Littman, D.R.; Dustin, M.L.; Gan, W.-B. ATP mediates rapid microglial response to local brain injury in vivo. Nat. Neurosci. 2005, 8, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Kimbler, D.E.; Shields, J.; Yanasak, N.; Vender, J.R.; Dhandapani, K.M. Activation of P2X7 promotes cerebral edema and neurological injury after traumatic brain injury in mice. PLoS ONE 2012, 7, e41229. [Google Scholar] [CrossRef] [PubMed]
- Howell, O.; Palser, A.; Polito, A.; Melrose, S.; Zonta, B.; Scheiermann, C.; Vora, A.; Brophy, P.; Reynolds, R. Disruption of neurofascin localization reveals early changes preceding demyelination and remyelination in multiple sclerosis. Brain 2006, 129, 3173–3185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, W.; Fu, Y.; Shi, Y.; Cheng, J.-X.; Cao, P.; Shi, R. Paranodal myelin damage after acute stretch in guinea pig spinal cord. J. Neurotrauma 2012, 29, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Nave, K.-A. Myelination and support of axonal integrity by glia. Nature 2010, 468, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Reeves, T.M.; Greer, J.E.; Vanderveer, A.S.; Phillips, L.L. Proteolysis of submembrane cytoskeletal proteins ankyrin-g and αii-spectrin following diffuse brain injury: A role in white matter vulnerability at nodes of ranvier. Brain Pathol. 2010, 20, 1055–1068. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.C.; Mierzwa, A.J.; Sullivan, G.M.; Sanchez, M.A. Myelin and oligodendrocyte lineage cells in white matter pathology and plasticity after traumatic brain injury. Neuropharmacology 2016, 110, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Wang, H.; Huff, T.B.; Shi, R.; Cheng, J.X. Coherent anti-stokes raman scattering imaging of myelin degradation reveals a calcium-dependent pathway in lyso-ptdcho-induced demyelination. J. Neurosci. Res. 2007, 85, 2870–2881. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, H.; Sun, W.; Fu, Y.; Li, J.; Cheng, J.-X.; Nauman, E.; Shi, R. Compression induces acute demyelination and potassium channel exposure in spinal cord. J. Neurotrauma 2010, 27, 1109–1120. [Google Scholar] [CrossRef] [PubMed]
- Khorchid, A.; Ikura, M. How calpain is activated by calcium. Nat. Struct. Mol. Biol. 2002, 9, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Dupree, J.L.; Coetzee, T.; Blight, A.; Suzuki, K.; Popko, B. Myelin galactolipids are essential for proper node of ranvier formation in the cns. J. Neurosci. 1998, 18, 1642–1649. [Google Scholar] [CrossRef] [PubMed]
- Ohno, N.; Kidd, G.J.; Mahad, D.; Kiryu-Seo, S.; Avishai, A.; Komuro, H.; Trapp, B.D. Myelination and axonal electrical activity modulate the distribution and motility of mitochondria at CNS nodes of ranvier. J. Neurosci. 2011, 31, 7249–7258. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.C.; Akle, V.; Zheng, W.; Kitlen, J.; O’steen, B.; Larner, S.F.; Dave, J.R.; Tortella, F.C.; Hayes, R.L.; Wang, K.K. Extensive degradation of myelin basic protein isoforms by calpain following traumatic brain injury. J. Neurochem. 2006, 98, 700–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saatman, K.E.; Murai, H.; Bartus, R.T.; Smith, D.H.; Hayward, N.J.; Perri, B.R.; McIntosh, T.K. Calpain inhibitor AK295 attenuates motor and cognitive deficits following experimental brain injury in the rat. Proc. Natl. Acad. Sci. USA 1996, 93, 3428–3433. [Google Scholar] [CrossRef] [PubMed]
- Karim, Z.; Sawada, A.; Kawakami, H.; Yamamoto, T.; Taniguchi, T. A new calcium channel antagonist, lomerizine, alleviates secondary retinal ganglion cell death after optic nerve injury in the rat. Curr. Eye Res. 2006, 31, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Milbourn, H.R.; Toomey, L.M.; Gavriel, N.; Gray, C.G.; Gough, A.H.; Fehily, B.; Giacci, M.K.; Fitzgerald, M. Limiting oxidative stress following neurotrauma with a combination of ion channel inhibitors. Discov. Med. 2017, 23, 361–369. [Google Scholar] [PubMed]
- Furukawa, T.; Hoshino, S.; Kobayashi, S.; Asakura, T.; Takahashi, M.; Atsumi, T.; Teramoto, A. The glutamate ampa receptor antagonist, YM872, attenuates cortical tissue loss, regional cerebral edema, and neurological motor deficits after experimental brain injury in rats. J. Neurotrauma 2003, 20, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Atsumi, T.; Hoshino, S.; Furukawa, T.; Kobayashi, S.; Asakura, T.; Takahashi, M.; Yamamoto, Y.; Teramoto, A. The glutamate ampa receptor antagonist, YM872, attenuates regional cerebral edema and IgG immunoreactivity following experimental brain injury in rats. In Brain Edema XII; Springer: Wien, Austria, 2003; pp. 305–307. [Google Scholar]
- Takahashi, M.; Ni, J.W.; Kawasaki-Yatsugi, S.; Toya, T.; Ichiki, C.; Yatsugi, S.-I.; Koshiya, K.; Shimizu-Sasamata, M.; Yamaguchi, T. Neuroprotective efficacy of YM872, an α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid receptor antagonist, after permanent middle cerebral artery occlusion in rats. J. Pharmacol. Exp. Ther. 1998, 287, 559–566. [Google Scholar] [PubMed]
- Peng, W.; Cotrina, M.L.; Han, X.; Yu, H.; Bekar, L.; Blum, L.; Takano, T.; Tian, G.-F.; Goldman, S.A.; Nedergaard, M. Systemic administration of an antagonist of the ATP-sensitive receptor P2X7 improves recovery after spinal cord injury. Proc. Natl. Acad. Sci. USA 2009, 106, 12489–12493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.C.; Cui, Y.; Cui, J.Z.; Sun, L.Q.; Cui, C.M.; Zhang, H.A.; Zhu, H.X.; Li, R.; Tian, Y.X.; Gao, J.L. Neuroprotective effects of brilliant blue G on the brain following traumatic brain injury in rats. Mol. Med. Rep. 2015, 12, 2149–2154. [Google Scholar] [CrossRef] [PubMed]
- Ridderström, M.; Ohlsson, M. Brilliant blue G treatment facilitates regeneration after optic nerve injury in the adult rat. NeuroReport 2014, 25, 1405–1410. [Google Scholar] [CrossRef] [PubMed]
- Gurkoff, G.; Shahlaie, K.; Lyeth, B.; Berman, R. Voltage-gated calcium channel antagonists and traumatic brain injury. Pharmaceuticals 2013, 6, 788–812. [Google Scholar] [CrossRef] [PubMed]
- Bickler, P.E.; Hansen, B.M. Causes of calcium accumulation in rat cortical brain slices during hypoxia and ischemia: Role of ion channels and membrane damage. Brain Res. 1994, 665, 269–276. [Google Scholar] [CrossRef]
- Tamaki, Y.; Araie, M.; Fukaya, Y.; Nagahara, M.; Imamura, A.; Honda, M.; Obata, R.; Tomita, K. Effects of lomerizine, a calcium channel antagonist, on retinal and optic nerve head circulation in rabbits and humans. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4864–4871. [Google Scholar] [CrossRef]
- Fitzgerald, M.; Payne, S.C.; Bartlett, C.A.; Evill, L.; Harvey, A.R.; Dunlop, S.A. Secondary retinal ganglion cell death and the neuroprotective effects of the calcium channel blocker lomerizine. Investig. Ophthalmol. Vis. Sci. 2009, 50, 5456–5462. [Google Scholar] [CrossRef] [PubMed]
- Morris, R. Developments of a water-maze procedure for studying spatial learning in the rat. J. Neurosci. Methods 1984, 11, 47–60. [Google Scholar] [CrossRef]






© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mao, Y.; Black, A.M.B.; Milbourn, H.R.; Krakonja, S.; Nesbit, M.; Bartlett, C.A.; Fehily, B.; Takechi, R.; Yates, N.J.; Fitzgerald, M. The Effects of a Combination of Ion Channel Inhibitors in Female Rats Following Repeated Mild Traumatic Brain Injury. Int. J. Mol. Sci. 2018, 19, 3408. https://doi.org/10.3390/ijms19113408
Mao Y, Black AMB, Milbourn HR, Krakonja S, Nesbit M, Bartlett CA, Fehily B, Takechi R, Yates NJ, Fitzgerald M. The Effects of a Combination of Ion Channel Inhibitors in Female Rats Following Repeated Mild Traumatic Brain Injury. International Journal of Molecular Sciences. 2018; 19(11):3408. https://doi.org/10.3390/ijms19113408
Chicago/Turabian StyleMao, Yilin, Anna M. B. Black, Hannah R. Milbourn, Samra Krakonja, Michael Nesbit, Carole A. Bartlett, Brooke Fehily, Ryu Takechi, Nathanael J. Yates, and Melinda Fitzgerald. 2018. "The Effects of a Combination of Ion Channel Inhibitors in Female Rats Following Repeated Mild Traumatic Brain Injury" International Journal of Molecular Sciences 19, no. 11: 3408. https://doi.org/10.3390/ijms19113408