An Overview on the Hallucinogenic Peyote and Its Alkaloid Mescaline: The Importance of Context, Ceremony and Culture
Abstract
:1. Introduction
2. Search Strategy
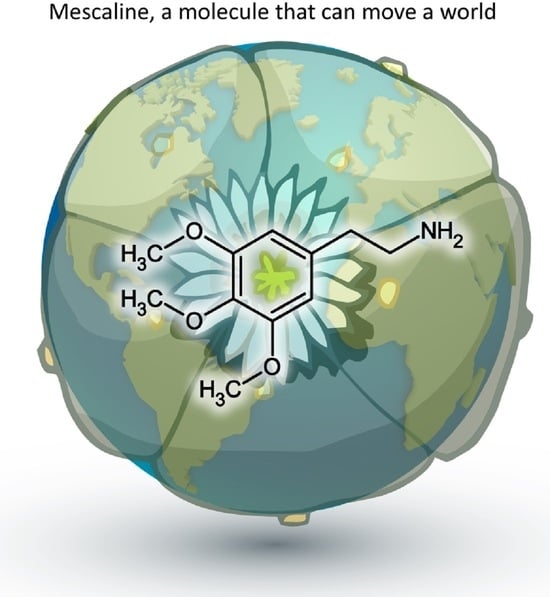
3. Mescaline—Metabolism, Clinical Reactions and Signalling
4. Mescaline—Chemistry and Synthesis
5. Peyote Alkaloids
| Alkaloid Content (Percent Total Alkaloid) | |
|---|---|
| Mescaline | 30.0 |
| Pellotine | 17.0 |
| Anhalonidine | 14.0 |
| Hordenine | 8.0 |
6. Clinical Studies and Therapeutic Potential of Mescaline
7. Ethnopharmacology
8. Different Ideas about Disease—Chances and Challenges
9. Future Research Aspects
10. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sahagún, B.; Bustamante, C.M. Historia General de las Cosas de Nueva España; Imprenta del Ciudadano Alejandro Valdés: Mexico City, Mexico, 1829. [Google Scholar]
- Lewin, L. Ueber Anhalonium lewinii und andere Cacteen. Naunyn-Schmiedeberg’s Arch. Pharmacol. 1894, 34, 374–391. [Google Scholar] [CrossRef]
- Lumholtz, C. Unknown Mexico: A Record of Five Years’ Exploration among the Tribes of the Western Sierra Madre; Cambridge University Press: Cambridge, UK, 2011; Volume 2. [Google Scholar]
- Stork, C.M. Peyote. In Reference Module in Biomedical Sciences; Elsevier: Amsterdam, The Netherlands, 2023. [Google Scholar]
- The ‘Diabolic Root’. New York Times, 1 November 1964; 96.
- US Drug Enforcement Administration Drug Scheduling. Available online: https://web.archive.org/web/20081020210309/http://www.usdoj.gov/dea/pubs/scheduling.html (accessed on 17 October 2023).
- International Narcotics Control Board List of Psychotropic Substances under International Control. Available online: https://web.archive.org/web/20051205125434/http://www.incb.org/pdf/e/list/green.pdf (accessed on 17 October 2023).
- Nutt, D. Illegal drugs laws: Clearing a 50-year-old obstacle to research. PLoS Biol. 2015, 13, e1002047. [Google Scholar] [CrossRef] [PubMed]
- 103d United States Congress American Indian Religious Freedom Act Amendments. Available online: https://www.congress.gov/103/statute/STATUTE-108/STATUTE-108-Pg3125.pdf (accessed on 17 October 2023).
- Decriminalize Nature—Organizer Info & Resources. Available online: https://www.decriminalizenature.org/policy/organizer-info-and-resources (accessed on 17 October 2023).
- Shulgin, A.T.; Shulgin, A. PIHKAL: Phenethylamines I have known and loved. In A Chemical Love Story; Transform Press Berkeley: Berkeley, CA, USA, 1991. [Google Scholar]
- Pollan, M. How Should We Do Drugs Now? New York Times, 11 July 2021. [Google Scholar]
- Ona, G.; Berrada, A.; Bouso, J.C. Communalistic use of psychoactive plants as a bridge between traditional healing practices and Western medicine: A new path for the Global Mental Health movement. Transcult. Psychiatry 2021, 59, 638–651. [Google Scholar] [CrossRef] [PubMed]
- Bruhn, J.G.; Holmstedt, B.R. Early peyote research an interdisciplinary study. Econ. Bot. 1973, 28, 353–390. [Google Scholar] [CrossRef]
- Monte, A.P.; Waldman, S.R.; Marona-Lewicka, D.; Wainscott, D.B.; Nelson, D.L.; Sanders-Bush, E.; Nichols, D.E. Dihydrobenzofuran analogues of hallucinogens. 4. Mescaline derivatives. J. Med. Chem. 1997, 40, 2997–3008. [Google Scholar] [CrossRef] [PubMed]
- Graziano, S.; Orsolini, L.; Rotolo, M.C.; Tittarelli, R.; Schifano, F.; Pichini, S. Herbal Highs: Review on Psychoactive Effects and Neuropharmacology. Curr. Neuropharmacol. 2017, 15, 750–761. [Google Scholar] [CrossRef]
- Aghajanian, G.K.; Marek, G.J. Serotonin and hallucinogens. Neuropsychopharmacology 1999, 21 (Suppl. 2), 16S–23S. [Google Scholar] [CrossRef]
- Shulgin, A.T. Mescaline: The chemistry and pharmacology of its analogs. Lloydia 1973, 36, 46–58. [Google Scholar]
- López-Giménez, J.F.; González-Maeso, J. Hallucinogens and Serotonin 5-HT(2A) Receptor-Mediated Signaling Pathways. Curr. Top. Behav. Neurosci. 2018, 36, 45–73. [Google Scholar]
- Hannon, J.; Hoyer, D. Molecular biology of 5-HT receptors. Behav. Brain Res. 2008, 195, 198–213. [Google Scholar] [CrossRef]
- Raymond, J.R.; Mukhin, Y.V.; Gelasco, A.; Turner, J.; Collinsworth, G.; Gettys, T.W.; Grewal, J.S.; Garnovskaya, M.N. Multiplicity of mechanisms of serotonin receptor signal transduction. Pharmacol. Ther. 2001, 92, 179–212. [Google Scholar] [CrossRef] [PubMed]
- Leung, J.; Chan, G.; Stjepanović, D.; Chung, J.Y.C.; Hall, W.; Hammond, D. Prevalence and self-reported reasons of cannabis use for medical purposes in USA and Canada. Psychopharmacology 2022, 239, 1509–1519. [Google Scholar] [CrossRef] [PubMed]
- Kilcher, G.; Zwahlen, M.; Ritter, C.; Fenner, L.; Egger, M. Medical use of cannabis in Switzerland: Analysis of approved exceptional licences. Swiss Med. Wkly. 2017, 147, w14463. [Google Scholar] [PubMed]
- Coughenour, P.; Sadicario, J.S.; Karjane, N.; Parlier-Ahmad, A.B.; Phipps, L.; Svikis, D.S. Prevalence and Social Acceptability of Cannabis, Tobacco, and Alcohol Use in Adult Women. Womens Health Rep. 2021, 2, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Ansah, J.P.; Chiu, C.T. Projecting the chronic disease burden among the adult population in the United States using a multi-state population model. Front. Public Health 2022, 10, 1082183. [Google Scholar] [CrossRef]
- World Health Organization Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 17 October 2023).
- Statista Global Drug Use—Statistics & Facts. Available online: https://www.statista.com/topics/7786/global-drug-use/#topicOverview (accessed on 17 October 2023).
- Collins, E.; Tranter, S.; Irvine, F. The physical health of the seriously mentally ill: An overview of the literature. J. Psychiatr. Ment. Health Nurs. 2012, 19, 638–646. [Google Scholar] [CrossRef]
- Farnam, C.R.; Zipple, A.M.; Tyrrell, W.; Chittinanda, P. Health status risk factors of people with severe and persistent mental illness. J. Psychosoc. Nurs. Ment. Health Serv. 1999, 37, 16–21. [Google Scholar] [CrossRef]
- Belouin, S.J.; Henningfield, J.E. Psychedelics: Where we are now, why we got here, what we must do. Neuropharmacology 2018, 142, 7–19. [Google Scholar] [CrossRef]
- Chapman, D.P.; Perry, G.S.; Strine, T.W. The vital link between chronic disease and depressive disorders. Prev. Chronic Dis. 2005, 2, A14. [Google Scholar]
- Bauml, J.A.; Schaefer, S.B.; Labate, B.C.; Cavnar, C. Peyote: History, Tradition, Politics, and Conservation; Bloomsbury Publishing: London, UK, 2016. [Google Scholar]
- Laing, R.R. Hallucinogens: A Forensic Drug Handbook; Academic Press: Cambridge, MA, USA, 2003. [Google Scholar]
- Wolbach, A.; Isbell, H.; Miner, E. Cross tolerance between mescaline and LSD-25 with a comparison of the mescaline and LSD reactions. Psychopharmacologia 1962, 3, 1–14. [Google Scholar] [CrossRef]
- Hartman, A.M.; Hollister, L.E. Effect of mescaline, lysergic acid diethylamide and psilocybin on color perception. Psychopharmacologia 1963, 4, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Lysergic acid diethylamide: Side effects and complications. J. Nerv. Ment. Dis. 1960, 130, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Denber, H.C.; Merlis, S. Studies on mescaline I. Action in schizophrenic patients: Clinical observations and brain wave patterns, showing effects before and after electric convulsive treatments. Psychiatr. Q. 1955, 29, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Oepen, G.; Fuenfgeld, M.; Harrington, A.; Hermle, L.; Botsch, H. Right hemisphere involvement in mescaline-induced psychosis. Psychiatry Res. 1989, 29, 335–336. [Google Scholar] [CrossRef] [PubMed]
- Hermle, L.; Fünfgeld, M.; Oepen, G.; Botsch, H.; Borchardt, D.; Gouzoulis, E.; Fehrenbach, R.A.; Spitzer, M. Mescaline-induced psychopathological, neuropsychological, and neurometabolic effects in normal subjects: Experimental psychosis as a tool for psychiatric research. Biol. Psychiatry 1992, 32, 976–991. [Google Scholar] [CrossRef] [PubMed]
- Hermle, L.; Gouzoulis-Mayfrank, E.; Spitzer, M. Blood flow and cerebral laterality in the mescaline model of psychosis. Pharmacopsychiatry 1998, 31, 85–91. [Google Scholar] [CrossRef]
- Dasgupta, A. Chapter Five—Challenges in Laboratory Detection of Unusual Substance Abuse: Issues with Magic Mushroom, Peyote Cactus, Khat, and Solvent Abuse. Adv. Clin. Chem. 2017, 78, 163–186. [Google Scholar]
- Kapadia, G.J.; Fayez, M.B.E. Peyote constituents: Chemistry, biogenesis, and biological effects. J. Pharm. Sci. 1970, 59, 1699–1727. [Google Scholar] [CrossRef]
- Cumming, P.; Scheidegger, M.; Dornbierer, D.; Palner, M.; Quednow, B.B.; Martin-Soelch, C. Molecular and Functional Imaging Studies of Psychedelic Drug Action in Animals and Humans. Molecules 2021, 26, 2451. [Google Scholar] [CrossRef]
- Korr, H. Autoradiographic studies on the distribution of 3H-mescaline in the brain of the marmoset, Callithrix jacchus. Psychopharmacologia 1976, 46, 115–117. [Google Scholar] [CrossRef]
- Dinis-Oliveira, R.J.; Pereira, C.L.; da Silva, D.D. Pharmacokinetic and Pharmacodynamic Aspects of Peyote and Mescaline: Clinical and Forensic Repercussions. Curr. Mol. Pharmacol. 2019, 12, 184–194. [Google Scholar] [CrossRef] [PubMed]
- Hilliker, K.S.; Roth, R.A. Prediction of mescaline clearance by rabbit lung and liver from enzyme kinetic data. Biochem. Pharmacol. 1980, 29, 253–255. [Google Scholar] [CrossRef] [PubMed]
- Seiler, N.; Demisch, L. Oxidative metabolism of mescaline in the central nervous system. 3. Side chain degradation of mescaline and formation of 3,4,5-trimethoxy-benzoic acid in vivo. Biochem. Pharmacol. 1974, 23, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Musacchio, J.M.; Goldstein, M. The metabolism of mescaline-14-C in rats. Biochem. Pharmacol. 1967, 16, 963–970. [Google Scholar] [CrossRef] [PubMed]
- Charalampous, K.D.; Walker, K.E.; Kinross-Wright, J. Metabolic fate of mescaline in man. Psychopharmacologia 1966, 9, 48–63. [Google Scholar] [CrossRef]
- Dasgupta, A. Chapter 33—Abuse of Magic Mushroom, Peyote Cactus, LSD, Khat, and Volatiles. In Critical Issues in Alcohol and Drugs of Abuse Testing, 2nd ed.; Dasgupta, A., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 477–494. [Google Scholar]
- Charalampous, K.D.; Orengo, A.; Walker, K.E.; Kinross-Wright, J. Metabolic fate of ν-(3,4,5-trimethoxyphenyl)-ethylamine (mescaline) in humans: Isolation and identification of 3,4,5-trimethoxyphenylacetic acid. J. Pharmacol. Exp. Ther. 1964, 145, 242–246. [Google Scholar] [PubMed]
- Pálenícek, T.; Balíková, M.; Bubeníková-Valesová, V.; Horácek, J. Mescaline effects on rat behavior and its time profile in serum and brain tissue after a single subcutaneous dose. Psychopharmacology 2008, 196, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Halberstadt, A.L.; Powell, S.B.; Geyer, M.A. Role of the 5-HT2A receptor in the locomotor hyperactivity produced by phenylalkylamine hallucinogens in mice. Neuropharmacology 2013, 70, 218–227. [Google Scholar] [CrossRef]
- Rickli, A.; Moning, O.D.; Hoener, M.C.; Liechti, M.E. Receptor interaction profiles of novel psychoactive tryptamines compared with classic hallucinogens. Eur. Neuropsychopharmacol. 2016, 26, 1327–1337. [Google Scholar] [CrossRef]
- Patel, V.; Urban, L.; Vaz, R.J. Antitargets and Drug Safety; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Vamvakopoulou, I.A.; Narine, K.A.D.; Campbell, I.; Dyck, J.R.B.; Nutt, D.J. Mescaline: The forgotten psychedelic. Neuropharmacology 2023, 222, 109294. [Google Scholar] [CrossRef]
- Urban, J.D.; Clarke, W.P.; von Zastrow, M.; Nichols, D.E.; Kobilka, B.; Weinstein, H.; Javitch, J.A.; Roth, B.L.; Christopoulos, A.; Sexton, P.M.; et al. Functional selectivity and classical concepts of quantitative pharmacology. J. Pharmacol. Exp. Ther. 2007, 320, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Kurrasch-Orbaugh, D.M.; Parrish, J.C.; Watts, V.J.; Nichols, D.E. A complex signaling cascade links the serotonin2A receptor to phospholipase A2 activation: The involvement of MAP kinases. J. Neurochem. 2003, 86, 980–991. [Google Scholar] [CrossRef]
- Berg, K.A.; Maayani, S.; Goldfarb, J.; Scaramellini, C.; Leff, P.; Clarke, W.P. Effector pathway-dependent relative efficacy at serotonin type 2A and 2C receptors: Evidence for agonist-directed trafficking of receptor stimulus. Mol. Pharmacol. 1998, 54, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Xia, Z.; Gray, J.A.; Compton-Toth, B.A.; Roth, B.L. A direct interaction of PSD-95 with 5-HT2A serotonin receptors regulates receptor trafficking and signal transduction. J. Biol. Chem. 2003, 278, 21901–21908. [Google Scholar] [CrossRef]
- Abbas, A.I.; Yadav, P.N.; Yao, W.D.; Arbuckle, M.I.; Grant, S.G.; Caron, M.G.; Roth, B.L. PSD-95 is essential for hallucinogen and atypical antipsychotic drug actions at serotonin receptors. J. Neurosci. 2009, 29, 7124–7136. [Google Scholar] [CrossRef]
- González-Maeso, J.; Weisstaub, N.V.; Zhou, M.; Chan, P.; Ivic, L.; Ang, R.; Lira, A.; Bradley-Moore, M.; Ge, Y.; Zhou, Q.; et al. Hallucinogens recruit specific cortical 5-HT(2A) receptor-mediated signaling pathways to affect behavior. Neuron 2007, 53, 439–452. [Google Scholar] [CrossRef] [PubMed]
- González-Maeso, J.; Yuen, T.; Ebersole, B.J.; Wurmbach, E.; Lira, A.; Zhou, M.; Weisstaub, N.; Hen, R.; Gingrich, J.A.; Sealfon, S.C. Transcriptome fingerprints distinguish hallucinogenic and nonhallucinogenic 5-hydroxytryptamine 2A receptor agonist effects in mouse somatosensory cortex. J. Neurosci. 2003, 23, 8836–8843. [Google Scholar] [CrossRef] [PubMed]
- Trulson, M.E.; Crisp, T.; Henderson, L.J. Mescaline elicits behavioral effects in cats by an action at both serotonin and dopamine receptors. Eur. J. Pharmacol. 1983, 96, 151–154. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information PubChem Compound Summary for CID 4076, Mescaline. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Mescaline (accessed on 13 November 2023).
- Reti, L. Fortschritte der Chemie organischer Naturstoffe; Zechmeister, L., Ed.; Springer: Wien, Austria, 1950; Volume VI. [Google Scholar]
- Cassels, B.K.; Sáez-Briones, P. Dark Classics in Chemical Neuroscience: Mescaline. ACS Chem. Neurosci. 2018, 9, 2448–2458. [Google Scholar] [CrossRef]
- McLean, T.H.; Parrish, J.C.; Braden, M.R.; Marona-Lewicka, D.; Gallardo-Godoy, A.; Nichols, D.E. 1-Aminomethylbenzocycloalkanes: Conformationally restricted hallucinogenic phenethylamine analogues as functionally selective 5-HT2A receptor agonists. J. Med. Chem. 2006, 49, 5794–5803. [Google Scholar] [CrossRef]
- Ibarra-Laclette, E.; Zamudio-Hernández, F.; Pérez-Torres, C.A.; Albert, V.A.; Ramírez-Chávez, E.; Molina-Torres, J.; Fernández-Cortes, A.; Calderón-Vázquez, C.; Olivares-Romero, J.L.; Herrera-Estrella, A. De novo sequencing and analysis of Lophophora williamsii transcriptome, and searching for putative genes involved in mescaline biosynthesis. BMC Genom. 2015, 16, 657. [Google Scholar] [CrossRef] [PubMed]
- Späth, E. Über die Anhalonium-Alkaloide: I. Anhalin und Mezcalin. Monatshefte Für Chem. Und Verwandte Teile Anderer Wiss. 1919, 40, 129–154. [Google Scholar] [CrossRef]
- Slotta, K.; Heller, H. Über β-Phenyl-äthylamine, I. Mitteil.: Mezcalin und mezcalin-ähnliche Substanzen. Berichte Der Dtsch. Chem. Ges. (A B Ser.) 1930, 63, 3029–3044. [Google Scholar] [CrossRef]
- Kindler, K.; Peschke, W. Über neue und über verbesserte Wege zum Aufbau von pharmakologisch wichtigen Aminen III. Über die Synthese von Adrenalin und von adrenalinähnlichen Verbindungen. Arch. Der Pharm. 1931, 269, 581–606. [Google Scholar] [CrossRef]
- Kindler, K.; Peschke, W. Über neue und über verbesserte Wege zum Aufbau von pharmakologisch wichtigen Aminen VI. Über Synthesen des Meskalins. Arch. Der Pharm. 1932, 270, 410–413. [Google Scholar] [CrossRef]
- Hahn, G.; Wassmuth, H. Über β-[Oxyphenyl]-äthylamine und ihre Umwandlungen, I. Mitteil.: Synthese des Mezcalins. Berichte Der Dtsch. Chem. Ges. (A B Ser.) 1934, 67, 696–708. [Google Scholar] [CrossRef]
- Erne, M.; Ramirez, F. Über die Reduktion von β-Nitrostyrolen mit Lithiumaluminiumhydrid. Helv. Chim. Acta 1950, 33, 912–916. [Google Scholar] [CrossRef]
- Banholzer, K.; Campbell, T.W.; Schmid, H. Notiz über eine neue Synthese von Mezcalin, N-Methyl-und N-Dimethylmezcalin. Helv. Chim. Acta 1952, 35, 1577–1581. [Google Scholar] [CrossRef]
- Rose-Munch, F.; Chavignon, R.; Tranchier, J.-P.; Gagliardini, V.; Rose, E. Mescaline synthesis via tricarbonyl (η6-1, 2, 3-trimethoxybenzene) chromium complex. Inorganica Chim. Acta 2000, 300, 693–697. [Google Scholar] [CrossRef]
- Soderquist, J.A.; Kock, I.; Estrella, M.E. Reductive cleavage of acetals and ketals with 9-borabicyclo[3.3. 1]nonane. Org. Process Res. Dev. 2006, 10, 1076–1079. [Google Scholar] [CrossRef]
- Bäumle, S. Heilpflanzenpraxis Heute: Porträts—Rezepturen—Anwendung; Urban & Fischer by Elsevier: Munich, Germany, 2006. [Google Scholar]
- Frank, M.; Weckman, T.J.; Wood, T.; Woods, W.E.; Tai, C.L.; Chang, S.L.; Ewing, A.; Blake, J.W.; Tobin, T. Hordenine: Pharmacology, pharmacokinetics and behavioural effects in the horse. Equine Vet. J. 1990, 22, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Steiner, I.; Brauers, G.; Temme, O.; Daldrup, T. A sensitive method for the determination of hordenine in human serum by ESI⁺ UPLC-MS/MS for forensic toxicological applications. Anal. Bioanal. Chem. 2016, 408, 2285–2292. [Google Scholar] [CrossRef]
- Zhou, J.-W.; Luo, H.-Z.; Jiang, H.; Jian, T.-K.; Chen, Z.-Q.; Jia, A.-Q. Hordenine: A Novel Quorum Sensing Inhibitor and Antibiofilm Agent against Pseudomonas aeruginosa. J. Agric. Food Chem. 2018, 66, 1620–1628. [Google Scholar] [CrossRef] [PubMed]
- Pilcz, A. Ueber Pellotin. Klin. Wochenschr. 1896, 9, 1121–1122. [Google Scholar]
- Chan, C.B.; Poulie, C.B.M.; Wismann, S.S.; Soelberg, J.; Kristensen, J.L. The Alkaloids from Lophophora diffusa and Other “False Peyotes”. J. Nat. Prod. 2021, 84, 2398–2407. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, R. Report on the use of pellotine as a sedative and hypnotic. State Hosp. Bull. 1897, 2, 45–48. [Google Scholar]
- Krüger, E. Die Wirkung des Pellotin im Kindesalter. Klin. Wochenschr. 1934, 13, 376–378. [Google Scholar] [CrossRef]
- Perrine, D.M. Visions of the Night-Western Medicine Meets Peyote 1887–1899. Heffter Rev. Psychedelic Res 2001, 2, 6–52. [Google Scholar]
- Poulie, C.B.M.; Chan, C.B.; Parka, A.; Lettorp, M.; Vos, J.; Raaschou, A.; Pottie, E.; Bundgaard, M.S.; Sørensen, L.M.E.; Cecchi, C.R.; et al. In Vitro and In Vivo Evaluation of Pellotine: A Hypnotic Lophophora Alkaloid. ACS Pharmacol. Transl. Sci. 2023, 6, 1492–1507. [Google Scholar] [CrossRef]
- Ghansah, E.; Kopsombut, P.; Maleque, M.A.; Brossi, A. Effects of mescaline and some of its analogs on cholinergic neuromuscular transmission. Neuropharmacology 1993, 32, 169–174. [Google Scholar] [CrossRef]
- Merlis, S. The effects of mescaline sulfate in chronic schizophrenia. J. Nerv. Ment. Dis. 1957, 125, 432–433. [Google Scholar] [CrossRef] [PubMed]
- Albaugh, B.J.; Anderson, P.O. Peyote in the treatment of alcoholism among American Indians. Am. J. Psychiatry 1974, 131, 1247–1250. [Google Scholar] [CrossRef] [PubMed]
- Halpern, J.H.; Sherwood, A.R.; Hudson, J.I.; Yurgelun-Todd, D.; Pope, H.G., Jr. Psychological and cognitive effects of long-term peyote use among Native Americans. Biol. Psychiatry 2005, 58, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Agin-Liebes, G.; Haas, T.F.; Lancelotta, R.; Uthaug, M.V.; Ramaekers, J.G.; Davis, A.K. Naturalistic use of mescaline is associated with self-reported psychiatric improvements and enduring positive life changes. ACS Pharmacol. Transl. Sci. 2021, 4, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Uthaug, M.V.; Davis, A.K.; Haas, T.F.; Davis, D.; Dolan, S.B.; Lancelotta, R.; Timmermann, C.; Ramaekers, J.G. The epidemiology of mescaline use: Pattern of use, motivations for consumption, and perceived consequences, benefits, and acute and enduring subjective effects. J. Psychopharmacol. 2022, 36, 309–320. [Google Scholar] [CrossRef] [PubMed]
- United States National Library of Medicine ClinicalTrials.gov—Search Results: Mescaline. Available online: https://clinicaltrials.gov/study/NCT05180149?intr=Mescaline&rank=6 (accessed on 13 October 2023).
- Feest, C.F. Beseelte Welten: Die Religionen der Indianer Nordamerikas; Herder: Middelburg, The Netherlands, 1998. [Google Scholar]
- Shemluck, M. Medicinal and other uses of the Compositae by Indians in the United States and Canada. J. Ethnopharmacol. 1982, 5, 303–358. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.N. The Native American Church, peyote, and health: Expanding consciousness for healing purposes. Contemp. Justice Rev. 2007, 10, 411–425. [Google Scholar] [CrossRef]
- Ronald Reagan Presidential Library Digital Library Collections Folder Title: Native American Church of North America. Available online: https://www.reaganlibrary.gov/public/digitallibrary/smof/publicliaison/blackwell/box-038/40_047_7007844_038_007_2017.pdf (accessed on 10 October 2023).
- Carvalho, I.; Steil, C.; Gonzaga, F. Learning from a more-than-human perspective. Plants as teachers. J. Environ. Educ. 2020, 51, 144–155. [Google Scholar] [CrossRef]
- Mastinu, A.; Anyanwu, M.; Carone, M.; Abate, G.; Bonini, S.A.; Peron, G.; Tirelli, E.; Pucci, M.; Ribaudo, G.; Oselladore, E.; et al. The Bright Side of Psychedelics: Latest Advances and Challenges in Neuropharmacology. Int. J. Mol. Sci. 2023, 24, 1329. [Google Scholar] [CrossRef]
- Jones, P.N. The American Indian Church and its sacramental use of peyote: A review for professionals in the mental-health arena. Ment. Health Relig. Cult. 2005, 8, 277–290. [Google Scholar] [CrossRef]
- Schultes, R.E. The botanical and chemical distribution of hallucinogens. Annu. Rev. Plant Physiol. 1970, 21, 571–598. [Google Scholar] [CrossRef]
- Schultes, R.E. An overview of hallucinogens in the Western Hemisphere. In Flesh of the Gods; Furst, P.T., Ed.; Praeger Publishers: New York, NY, USA, 1972. [Google Scholar]
- Metzner, R. Hallucinogenic drugs and plants in psychotherapy and shamanism. J. Psychoact. Drugs 1998, 30, 333–341. [Google Scholar] [CrossRef]
- Garrity, J.F. Jesus, peyote, and the holy people: Alcohol abuse and the ethos of power in Navajo healing. Med. Anthr. Q. 2000, 14, 521–542. [Google Scholar] [CrossRef] [PubMed]
- McClusky, M.S.W. Native American Church Peyotism and the Treatment of Alcoholism. Newsl. Multidiscip. Assoc. Psychedelic Stud. MAPS 1997, 7, 3–4. [Google Scholar]
- Huttlinger, K.W.; Tanner, D. The Peyote way: Implications for Culture Care theory. J. Transcult. Nurs. 1994, 5, 5–11. [Google Scholar] [CrossRef]
- World Health Organization the Constitution. Available online: https://www.who.int/about/accountability/governance/constitution (accessed on 25 October 2023).
- Yuan, B. Holistic medicine: A new medical system based on body constitution and functional status. J. Tradit. Chin. Med. Sci. 2017, 4, 3–9. [Google Scholar] [CrossRef]
- Risch, N.; Merikangas, K. The future of genetic studies of complex human diseases. Science 1996, 273, 1516–1517. [Google Scholar] [CrossRef]
- Broadbent, A. Causation and models of disease in epidemiology. Stud. Hist. Philos. Biol. Biomed. Sci. 2009, 40, 302–311. [Google Scholar] [CrossRef]
- Longdon, E.; Read, J. ‘People with Problems, Not Patients with Illnesses’: Using Psychosocial Frameworks to Reduce the Stigma of Psychosis. Isr. J. Psychiatry Relat. Sci. 2017, 54, 24–28. [Google Scholar]
- World Health Organization Alcohol. Available online: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed on 17 October 2023).
- Skolnick, P. The Opioid Epidemic: Crisis and Solutions. Annu. Rev. Pharmacol. Toxicol. 2018, 58, 143–159. [Google Scholar] [CrossRef]
- Huxley, A. The Doors of Perception; Strelbytskyy Multimedia Publishing: Kyiv, Ukraine, 2021. [Google Scholar]
- Collins, P.Y.; Patel, V.; Joestl, S.S.; March, D.; Insel, T.R.; Daar, A.S.; Scientific Advisory, B.; The Executive Committee of the Grand Challenges on Global Mental Health; Anderson, W.; Dhansay, M.A.; et al. Grand challenges in global mental health. Nature 2011, 475, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Metzner, R. (Ed.) Ayahuasca: Hallucinogens, Consciousness, and the Spirit of Nature; Running Press: Philadelphia, PA, USA, 1999. [Google Scholar]
- Eisner, B. Set, setting, and matrix. J. Psychoact. Drugs 1997, 29, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.A.; Suissa-Rocheleau, L.; Lifshitz, M.; Raz, A.; Veissiere, S.P.L. Tripping on nothing: Placebo psychedelics and contextual factors. Psychopharmacology 2020, 237, 1371–1382. [Google Scholar] [CrossRef] [PubMed]
- Hartogsohn, I. Constructing drug effects: A history of set and setting. Drug Sci. Policy Law 2017, 3, 2050324516683325. [Google Scholar] [CrossRef]
- Hartogsohn, I. Set and setting, psychedelics and the placebo response: An extra-pharmacological perspective on psychopharmacology. J. Psychopharmacol. 2016, 30, 1259–1267. [Google Scholar] [CrossRef]
- Soloman, D. LSD—The Consciousness-Expanding Drug; Berkley Medallion Book: Berkley, CA, USA, 1966. [Google Scholar]
- O’Shaughnessy, D.M.; Berlowitz, I. Amazonian Medicine and the Psychedelic Revival: Considering the “Dieta”. Front. Pharmacol. 2021, 12, 639124. [Google Scholar] [CrossRef]
- Berlowitz, I.; O’Shaughnessy, D.M.; Heinrich, M.; Wolf, U.; Maake, C.; Martin-Soelch, C. Teacher plants—Indigenous Peruvian-Amazonian dietary practices as a method for using psychoactives. J. Ethnopharmacol. 2022, 286, 114910. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Doesburg-van Kleffens, M.; Zimmermann-Klemd, A.M.; Gründemann, C. An Overview on the Hallucinogenic Peyote and Its Alkaloid Mescaline: The Importance of Context, Ceremony and Culture. Molecules 2023, 28, 7942. https://doi.org/10.3390/molecules28247942
Doesburg-van Kleffens M, Zimmermann-Klemd AM, Gründemann C. An Overview on the Hallucinogenic Peyote and Its Alkaloid Mescaline: The Importance of Context, Ceremony and Culture. Molecules. 2023; 28(24):7942. https://doi.org/10.3390/molecules28247942
Chicago/Turabian StyleDoesburg-van Kleffens, Marjolein, Amy M. Zimmermann-Klemd, and Carsten Gründemann. 2023. "An Overview on the Hallucinogenic Peyote and Its Alkaloid Mescaline: The Importance of Context, Ceremony and Culture" Molecules 28, no. 24: 7942. https://doi.org/10.3390/molecules28247942