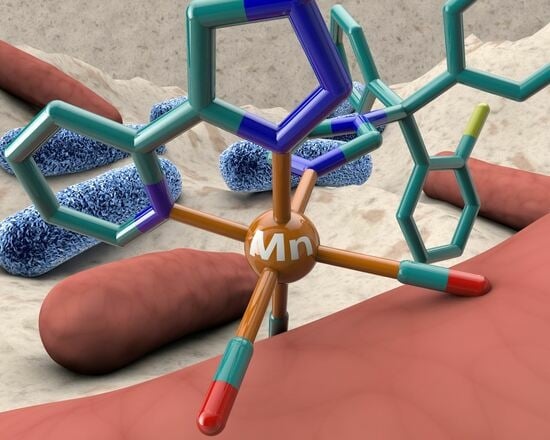
Antimicrobial Activity of Manganese(I) Tricarbonyl Complexes Bearing 1,2,3-Triazole Ligands
Abstract
:1. Introduction
2. Results and Discussion
2.1. Synthesis
2.2. Antimicrobial Activity of the Complexes against Gram-Positive and -Negative Bacteria
2.3. Effects of the Compound 4 on the Bacterial Growth of Gram-Positive and Gram-Negative Bacteria
2.4. Effects of Complexes 4–6 on the Cellular Viability of Human Monocytes
3. Materials and Methods
3.1. Synthesis
Synthetic Procedures
3.2. Crystallography
3.3. Biological Studies
3.3.1. Antimicrobial Activity
3.3.2. Effects of the Compounds on the Viability of Human Monocytes—MTS Assay
3.3.3. Data Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nicolaou, K.C.; Chen, J.S.; Edmonds, D.J.; Estrada, A.A. Recent advances in the chemistry and biology of naturally occurring antibiotics. Angew. Chem. Int. Ed. 2009, 48, 660–719. [Google Scholar] [CrossRef] [PubMed]
- Saxena, S.; Gomber, C. Surmounting Antimicrobial Resistance in the Millennium Superbug: Staphylococcus aureus. Cent. Eur. J. Med. 2010, 5, 12–29. [Google Scholar] [CrossRef]
- Martin, J.K., II; Sheehan, J.P.; Bratton, B.P.; Moore, G.M.; Mateus, A.; Li, S.H.-J.; Kim, H.; Rabinowitz, J.D.; Typas, A.; Savitski, M.M.; et al. A Dual-Mechanism Antibiotic Kills Gram-Negative Bacteria and Avoids Drug Resistance. Cell 2020, 181, 1518–1532.e14. [Google Scholar] [CrossRef] [PubMed]
- Biot, C.; Castro, W.; Botté, C.Y.; Navarro, M. The therapeutic potential of metal-based antimalarial agents: Implications for the mechanism of action. Dalton Trans. 2012, 41, 6335–6349. [Google Scholar] [CrossRef] [PubMed]
- Hudej, R.; Kljun, J.; Kandioller, W.; Repnik, U.; Turk, B.; Hartinger, C.G.; Keppler, B.K.; Miklavčič, D.; Turel, I. Synthesis and biological evaluation of the thionated antibacterial agent nalidixic acid and its organoruthenium(II) complex. Organometallics 2012, 31, 5867–5874. [Google Scholar] [CrossRef]
- Coogan, M.P.; Dyson, P.J.; Bochmann, M. Introduction to the organometallics in biology and medicine issue. Organometallics 2012, 31, 5671–5672. [Google Scholar] [CrossRef]
- Frei, A.; Zuegg, J.; Elliott, A.G.; Baker, M.; Braese, S.; Brown, C.; Chen, F.; Dowson, C.G.; Dujardin, G.; Jung, N.; et al. Metal complexes as a promising source for new antibiotics. Chem. Sci. 2020, 11, 2627–2639. [Google Scholar] [CrossRef]
- Biot, C.; Dive, D. Bioorganometallic chemistry and malaria. Top. Organomet. Chem. 2010, 32, 155–193. [Google Scholar] [CrossRef]
- Casini, A.; Hartinger, C.G.; Nazarov, A.A.; Dyson, P.J. Organometallic antitumour agents with alternative modes of action. Top. Organomet. Chem. 2010, 32, 57–80. [Google Scholar] [CrossRef]
- Mora, M.; Gimeno, M.C.; Visbal, R. Recent advances in gold-NHC complexes with biological properties. Chem. Soc. Rev. 2019, 48, 447–462. [Google Scholar] [CrossRef]
- Martins, P.; Marques, M.; Coito, L.; Pombeiro, A.; Baptista, P.; Fernandes, A. Organometallic Compounds in Cancer Therapy: Past Lessons and Future Directions. Anticancer. Agents Med. Chem. 2014, 14, 1199–1212. [Google Scholar] [CrossRef] [PubMed]
- Kwofie, S.K.; Broni, E.; Dankwa, B.; Enninful, K.S.; Teye, J.; Davidson, C.R.; Nimely, J.B.; Chioma Orizu, J.; Kempaiah, P.; Rathi, B.; et al. Review of Atypical Organometallic Compounds as Antimalarial Drugs. J. Chem. 2020, 2020, 1–9. [Google Scholar] [CrossRef]
- Navarro, M.; Castro, W.; Biot, C. Bioorganometallic Compounds with Antimalarial Targets: Inhibiting Hemozoin Formation. Organometallics 2012, 31, 5715–5727. [Google Scholar] [CrossRef]
- Glišić, B.; Djuran, M.I. Gold complexes as antimicrobial agents: An overview of different biological activities in relation to the oxidation state of the gold ion and the ligand structure. J. Chem. Soc. Dalton Trans. 2014, 43, 5950–5969. [Google Scholar] [CrossRef] [PubMed]
- Simpson, P.V.; Nagel, C.; Bruhn, H.; Schatzschneider, U. Antibacterial and Antiparasitic Activity of Manganese(I) Tricarbonyl Complexes with Ketoconazole, Miconazole, and Clotrimazole Ligands. Organometallics 2015, 34, 3809–3815. [Google Scholar] [CrossRef]
- Mendes, S.S.; Marques, J.; Mesterházy, E.; Straetener, J.; Arts, M.; Pissarro, T.; Reginold, J.; Berscheid, A.; Bornikoel, J.; Kluj, R.M.; et al. Synergetic Antimicrobial Activity and Mechanism of Clotrimazole-Linked CO-Releasing Molecules. ACS Bio. Med.Chem. Au. 2022, 2, 419–436. [Google Scholar] [CrossRef]
- Li, F.; Collins, J.G.; Keene, F.R. Ruthenium complexes as antimicrobial agents. Chem. Soc. Rev. 2015, 44, 2529–2542. [Google Scholar] [CrossRef]
- Duchane, C.M.; Brown, L.C.; Dozier, V.S.; Merola, J.S. Synthesis, Characterization, and Antimicrobial Activity of RhIII and IrIII β-Diketonato Piano-Stool Compounds. Organometallics 2018, 37, 530–538. [Google Scholar] [CrossRef]
- Simpson, P.V.; Schmidt, C.; Ott, I.; Bruhn, H.; Schatzschneider, U. Synthesis, Cellular Uptake and Biological Activity Against Pathogenic Microorganisms and Cancer Cells of Rhodium and Iridium N-Heterocyclic Carbene Complexes Bearing Charged Substituents. Eur. J. Inorg. Chem. 2013, 2013, 5547–5554. [Google Scholar] [CrossRef]
- Lu, L.; Liu, L.J.; Chao, W.C.; Zhong, H.J.; Wang, M.; Chen, X.P.; Lu, J.J.; Li, R.N.; Ma, D.L.; Leung, C.H. Identification of an iridium(III) complex with anti-bacterial and anti-cancer activity. Sci. Rep. 2015, 5, 14544. [Google Scholar] [CrossRef]
- Karpin, G.W.; Morris, D.M.; Ngo, M.T.; Merola, J.S.; Falkinham, J.O. Transition metal diamine complexes with antimicrobial activity against Staphylococcus aureus and methicillin-resistant S. aureus (MRSA). Medchemcomm 2015, 6, 1471–1478. [Google Scholar] [CrossRef]
- Ali, B.; Iqbal, M.A. Coordination Complexes of Manganese and Their Biomedical Applications. ChemistrySelect 2017, 2, 1586–1604. [Google Scholar] [CrossRef]
- Juttukonda, L.J.; Skaar, E.P. Manganese Homeostasis and Utilization in Pathogenic Bacteria: Manganese Utilization and Bacterial Virulence. Mol. Microbiol. 2015, 97, 216–228. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.; Kavanagh, K.A. Evaluation of Metal-Based Antimicrobial Compounds for the Treatment of Bacterial Pathogens. J. Med. Microbiol. 2021, 70, 5. [Google Scholar] [CrossRef]
- Betts, J.; Nagel, C.; Schatzschneider, U.; Poole, R.; Ragione, R.M. La Antimicrobial activity of carbon monoxide-releasing molecule [Mn(CO)3 tpa-κ3N)]Br versus multidrug-resistant isolates of Avian Pathogenic Escherichia coli and its synergy with colistin. PLoS ONE 2017, 12, e0186359. [Google Scholar] [CrossRef]
- Rana, N.; Jesse, H.E.; Tinajero-Trejo, M.; Butler, J.A.; Tarlit, J.D.; Von Und Zur Muhlen, M.L.; Nagel, C.; Schatzschneider, U.; Poole, R.K. A manganese photosensitive tricarbonyl molecule [Mn(CO)3(tpa-k3N)]Br enhances antibiotic efficacy in a multi-drug-resistant Escherichia coli. Microbiology 2017, 163, 1477–1489. [Google Scholar] [CrossRef] [PubMed]
- Ashok Kumar, C.; Divya, D.; Nagarajaprakash, R.; Veena, V.; Vidhyapriya, P.; Sakthivel, N.; Manimaran, B. Self-assembly of manganese(I) and rhenium(I) based semi-rigid ester functionalized M2L2-type metallacyclophanes: Synthesis, characterization and cytotoxicity evaluation. J. Organomet. Chem. 2017, 846, 152–160. [Google Scholar] [CrossRef]
- Musib, D.; Raza, M.K.; Martina, K.; Roy, M. Mn(I)-based photoCORMs for trackable, visible light-induced CO release and photocytotoxicity to cancer cells. Polyhedron 2019, 172, 125–131. [Google Scholar] [CrossRef]
- Tinajero-Trejo, M.; Rana, N.; Nagel, C.; Jesse, H.E.; Smith, T.W.; Wareham, L.K.; Hippler, M.; Schatzschneider, U.; Poole, R.K. Antimicrobial Activity of the Manganese Photoactivated Carbon Monoxide-Releasing Molecule [Mn(CO) 3 (tpa-j 3 N)] + Against a Pathogenic Escherichia coli that Causes Urinary Infections. Antioxid. Redox Signal 2016, 24, 765–780. [Google Scholar] [CrossRef]
- Bozorov, K.; Zhao, J.; Aisa, H.A. 1,2,3-Triazole-containing hybrids as leads in medicinal chemistry: A recent overview. Bioorganic Med. Chem. 2019, 27, 3511–3531. [Google Scholar] [CrossRef]
- Kommidi, H.; Guo, H.; Nurili, F.; Vedvyas, Y.; Jin, M.M.; McClure, T.D.; Ehdaie, B.; Sayman, H.B.; Akin, O.; Aras, O.; et al. 18F-Positron Emitting/Trimethine Cyanine-Fluorescent Contrast for Image-Guided Prostate Cancer Management. J. Med. Chem. 2018, 61, 4256–4262. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Zhao, S.J.; Liu, Y. 1,2,3-Triazole-containing hybrids as potential anticancer agents: Current developments, action mechanisms and structure-activity relationships. Eur. J. Med. Chem. 2019, 183, 111700. [Google Scholar] [CrossRef] [PubMed]
- El Malah, T.; Nour, H.F.; Satti, A.A.E.; Hemdan, B.A.; El-Sayed, W.A. Design, synthesis, and antimicrobial activities of 1,2,3-triazole glycoside clickamers. Molecules 2020, 25, 790. [Google Scholar] [CrossRef]
- Zhou, L.; Amer, A.; Korn, M.; Burda, R.; Balzarini, J.; De Clercq, E.; Kern, E.R.; Torrence, P.F. Synthesis and antiviral activities of 1,2,3-triazole functionalized thymidines: 1,3-dipolar cycloaddition for efficient regioselective diversity generation. Antivir. Chem. Chemother. 2005, 16, 375–383. [Google Scholar] [CrossRef]
- Chu, X.M.; Wang, C.; Wang, W.L.; Liang, L.L.; Liu, W.; Gong, K.K.; Sun, K.L. Triazole derivatives and their antiplasmodial and antimalarial activities. Eur. J. Med. Chem. 2019, 166, 206–223. [Google Scholar] [CrossRef]
- Shaikh, M.H.; Subhedar, D.D.; Nawale, L.; Sarkar, D.; Kalam Khan, F.A.; Sangshetti, J.N.; Shingate, B.B. 1,2,3-Triazole derivatives as antitubercular agents: Synthesis, biological evaluation and molecular docking study. MedChemComm 2015, 6, 1104–1116. [Google Scholar] [CrossRef]
- Bolje, A.; Urankar, D.; Košmrlj, J. Synthesis and NMR analysis of 1,4-disubstituted 1,2,3-triazoles tethered to pyridine, pyrimidine, and pyrazine rings. Eur. J. Org. Chem. 2014, 2014, 8167–8181. [Google Scholar] [CrossRef]
- Vivancos, Á.; Albrecht, M. Influence of the Linker Length and Coordination Mode of (Di)Triazolylidene Ligands on the Structure and Catalytic Transfer Hydrogenation Activity of Iridium(III) Centers. Organometallics 2017, 36, 1580–1590. [Google Scholar] [CrossRef]
- Bernet, L.; Lalrempuia, R.; Ghattas, W.; Mueller-Bunz, H.; Vigara, L.; Llobet, A.; Albrecht, M. Tunable single-site ruthenium catalysts for efficient water oxidation. Chem. Commun. 2011, 47, 8058–8060. [Google Scholar] [CrossRef]
- Raydan, D.; Friães, S.; Royo, B.; Marques, M.M.B.; Viduedo, N.; Santos, A.S.; Gomes, C.S.B. Manganese-Catalyzed Synthesis of Imines from Primary Alcohols and (Hetero)Aromatic Amines. Synlett 2022, 33, 1290–1294. [Google Scholar] [CrossRef]
- Friães, S.; Realista, S.; Gomes, C.S.B.; Martinho, P.N.; Royo, B. Click-Derived Triazoles and Triazolylidenes of Manganese for Electrocatalytic Reduction of CO2. Molecules 2021, 26, 6325. [Google Scholar] [CrossRef] [PubMed]
- Groom, C.R.; Bruno, I.J.; Lightfoot, M.P.; Ward, S.C. The Cambridge Structural Database. Acta Crystallogr. B Struct. Sci. Cryst. Eng. Mater. 2016, 72, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Wesseling, C.M.J.; Martin, N.I. Synergy by Perturbing the Gram-Negative Outer Membrane: Opening the Door for Gram-Positive Specific Antibiotics. ACS Infect. Dis. 2022, 8, 1731–1757. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Krause, L.; Herbst-Irmer, R.; Sheldrick, G.M.; Stalke, D. Comparison of Silver and Molybdenum Microfocus X-Ray Sources for Single-Crystal Structure Determination. J. Appl. Crystallogr. 2015, 48, 3–10. [Google Scholar] [CrossRef]
- Sheldrick, G.M. Crystal Structure Refinement withSHELXL. Acta Crystallogr. C Struct. Chem. 2015, 71, 3–8. [Google Scholar] [CrossRef]
- Hübschle, C.B.; Sheldrick, G.M.; Dittrich, B. ShelXle: A Qt Graphical User Interface for SHELXL. J. Appl. Crystallogr. 2011, 44, 1281–1284. [Google Scholar] [CrossRef]
- Farrugia, L.J. WinGXandORTEP for Windows: An Update. J. Appl. Crystallogr. 2012, 45, 849–854. [Google Scholar] [CrossRef]
- Alves Ferreira, D.; Martins, L.M.D.R.S.; Fernandes, A.R.; Martins, M. A Tale of Two Ends: Repurposing Metallic Compounds from Anti-Tumour Agents to Effective Antibacterial Activity. Antibiotics 2020, 9, 321. [Google Scholar] [CrossRef]





| Compounds | Bacterial Strains/MIC and (MBC) (µM) | |||||
|---|---|---|---|---|---|---|
| Gram-Positive Bacteria | Gram-Negative Bacteria | |||||
| S. aureus ATCC25923 | E. coli ATCC25922 | S. typhimurium 14028S | K. pneumoniae ATCC700603 | P. aeruginosa PAO1 | A. baumannii ATCC19606 | |
| 1 | 1411.33 (2822.66) | 2822.11 | 2822.11 | 2822.11 | 2822.11 | 2822.11 |
| 4 | 1.89 | 15.15 (30.29) | 30.29 | 60.59 | 15.15 | 1.89 (3.79) |
| 5 | 1.93 | 15.48 (30.98) | 30.97 | 61.95 (247.80) | 15.48 | 1.93 (3.88) |
| 6 | 1.79 | 7.19 (14.38) | 14.38 (28.76) | 57.52 | 7.19 (14.38) | 1.79 |
| Tetracycline | 0.81 | 3.51 | 13.78 | 56.25 (112.50) | 28.12 | 0.81 (1.75) |
| Thioridazine | 33.73 | 67.46 (134.93) | 539.70 | 1079.42 | 269.85 | 33.73 |
| Compounds | Bacterial Strains/MIC (µM) | |||||
|---|---|---|---|---|---|---|
| Gram-Positive Bacteria | Gram-Negative Bacteria | |||||
| S. aureus | E. coli | S. typhimurium | K. pneumoniae | P. aeruginosa | A. baumannii | |
| 4 | 1.89 | 15.15 | 30.29 | 60.59 | 15.15 | 1.89 |
| 5 | 1.93 | 15.48 | 30.97 | 61.95 | 15.48 | 1.93 |
| 6 | 1.79 | 7.19 | 14.38 | 57.52 | 7.19 | 1.79 |
| Mn1 | >43.15 | 10.78 | - | >43.15 | >43.15 | >43.15 |
| Mn2 | 0.625 | 40 | - | - | > 40 | - |
| Mn3 | 2.5 | >40 | - | - | > 40 | - |
| Mn4 | 40 | >40 | - | - | > 40 | - |
| Mn5 | 1.25 | 20 | - | - | > 40 | - |
| Mn6 | 2.5 | >40 | - | - | > 40 | - |
| Mn7 | 2.53 | 40.55 | - | - | - | - |
| Mn8 | 8.99 | 35.98 | - | - | - | - |
| Pt1 | 19.30 | 38.62 | - | 38.62 | >38.62 | >38.62 |
| Ir1 | 1.37 | 5.50 | - | 44.03 | >44.03 | 5.50 |
| Ru1 | 0.65 | 20.83 | - | >20.83 | >20.83 | >20.83 |
| Ru2 | 1.43 | 22.97 | - | >22.97 | >22.97 | >22.97 |
| Ag1 | 85.07 | 42.54 | - | 85.07 | 42.54 | 42.54 |
| Ag2 | 20 | 10 | - | 20 | >20 | 5.0 |
| Ag3 | 20 | 20 | - | 20 | >20 | 5.0 |
| Ag4 | >20 | 20 | - | >20 | >20 | 20 |
| Ag5 | >20 | >20 | - | >20 | >20 | 10 |
| Ag6 | >20 | 20 | - | >20 | >20 | 10 |
| Ag7 | >20 | 20 | - | >20 | >20 | 10 |
| Ag8 | 20 | 20 | - | >20 | >20 | 10 |
| Ag9 | >20 | >20 | - | >20 | >20 | 20 |
| Colistin | - | 0.11 | - | 2.16 | 2.16 | 2.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Friães, S.; Trigueiros, C.; Gomes, C.S.B.; Fernandes, A.R.; Lenis-Rojas, O.A.; Martins, M.; Royo, B. Antimicrobial Activity of Manganese(I) Tricarbonyl Complexes Bearing 1,2,3-Triazole Ligands. Molecules 2023, 28, 7453. https://doi.org/10.3390/molecules28217453
Friães S, Trigueiros C, Gomes CSB, Fernandes AR, Lenis-Rojas OA, Martins M, Royo B. Antimicrobial Activity of Manganese(I) Tricarbonyl Complexes Bearing 1,2,3-Triazole Ligands. Molecules. 2023; 28(21):7453. https://doi.org/10.3390/molecules28217453
Chicago/Turabian StyleFriães, Sofia, Cândida Trigueiros, Clara S. B. Gomes, Alexandra R. Fernandes, Oscar A. Lenis-Rojas, Marta Martins, and Beatriz Royo. 2023. "Antimicrobial Activity of Manganese(I) Tricarbonyl Complexes Bearing 1,2,3-Triazole Ligands" Molecules 28, no. 21: 7453. https://doi.org/10.3390/molecules28217453