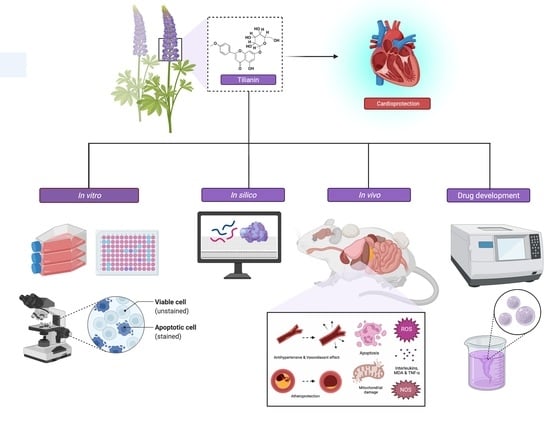
Tilianin: A Potential Natural Lead Molecule for New Drug Design and Development for the Treatment of Cardiovascular Disorders
Abstract
:1. Introduction
2. Cardioprotective Effect of Tilianin
3. Atheroprotective Effect of Tilianin
4. Antihypertensive and Vasorelaxant Effects of Tilianin
5. Overview of the Mechanisms of Action for Tilianin against CVDs
6. In-Silico Molecular Docking Study of Tilianin
7. Toxicity Profile of Tilianin
8. Pharmacokinetics and Bioavailability of Tilianin
9. Challenges and Opportunities of Tilianin to Be Developed as a Drug Molecule for the Treatment CVDs
10. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Cardiovascular Diseases. Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 24 September 2021).
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R. Heart disease and stroke statistics—2018 update: A report from the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef]
- Hausenloy, D.J.; Yellon, D.M. Cardioprotection (Oxford Cardiology Library); Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Sajid, M.; Cameotra, S.S.; Khan, M.S.A.; Ahmad, I. Nanoparticle-based delivery of phytomedicines: Challenges and opportunities. In New Look to Phytomedicine; Elsevier: Amsterdam, The Netherlands, 2019; pp. 597–623. [Google Scholar]
- Casertano, M.; Menna, M.; Imperatore, C. The ascidian-derived metabolites with antimicrobial properties. Antibiotics 2020, 9, 510. [Google Scholar] [CrossRef] [PubMed]
- Rosén, J.; Gottfries, J.; Muresan, S.; Backlund, A.; Oprea, T.I. Novel chemical space exploration via natural products. J. Med. Chem. 2009, 52, 1953–1962. [Google Scholar] [CrossRef] [Green Version]
- Ooi, B.K.; Chan, K.-G.; Goh, B.H.; Yap, W.H. The role of natural products in targeting cardiovascular diseases via Nrf2 pathway: Novel molecular mechanisms and therapeutic approaches. Front. Pharmacol. 2018, 9, 1308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cragg, G.M.; Newman, D.J. Natural products: A continuing source of novel drug leads. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2013, 1830, 3670–3695. [Google Scholar] [CrossRef] [Green Version]
- Ntie-Kang, F.; Svozil, D. An enumeration of natural products from microbial, marine and terrestrial sources. Phys. Sci. Rev. 2020, 5, 20180121. [Google Scholar] [CrossRef]
- Hernández-Abreu, O.; Torres-Piedra, M.; García-Jiménez, S.; Ibarra-Barajas, M.; Villalobos-Molina, R.; Montes, S.; Rembao, D.; Estrada-Soto, S. Dose-dependent antihypertensive determination and toxicological studies of tilianin isolated from Agastache mexicana. J. Ethnopharmacol. 2013, 146, 187–191. [Google Scholar] [CrossRef]
- Wei, J.; Cao, P.; Wang, J.; Kang, W. Analysis of tilianin and acacetin in Agastache rugosa by high-performance liquid chromatography with ionic liquids-ultrasound based extraction. Chem. Cent. J. 2016, 10, 76. [Google Scholar] [CrossRef] [Green Version]
- García-Díaz, J.A.; Navarrete-Vázquez, G.; García-Jiménez, S.; Hidalgo-Figueroa, S.; Almanza-Pérez, J.C.; Alarcón-Aguilar, F.J.; Gómez-Zamudio, J.; Cruz, M.; Ibarra-Barajas, M.; Estrada-Soto, S. Antidiabetic, antihyperlipidemic and anti-inflammatory effects of tilianin in streptozotocin-nicotinamide diabetic rats. Biomed. Pharmacother. 2016, 83, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Nam, K.-H.; Choi, J.-H.; Seo, Y.-J.; Lee, Y.-M.; Won, Y.-S.; Lee, M.-R.; Lee, M.-N.; Park, J.-G.; Kim, Y.-M.; Kim, H.-C. Inhibitory effects of tilianin on the expression of inducible nitric oxide synthase in low density lipoprotein receptor deficiency mice. Exp. Mol. Med. 2006, 38, 445–452. [Google Scholar] [CrossRef] [Green Version]
- Oh, H.M.; Kang, Y.J.; Lee, Y.S.; Park, M.K.; Kim, S.H.; Kim, H.J.; Seo, H.G.; Lee, J.H.; Chang, K.C. Protein kinase G-dependent heme oxygenase-1 induction by Agastache rugosa leaf extract protects RAW264. 7 cells from hydrogen peroxide-induced injury. J. Ethnopharmacol. 2006, 103, 229–235. [Google Scholar] [CrossRef]
- Gonzalez-Trujano, M.E.; Ponce-Muñoz, H.; Hidalgo-Figueroa, S.; Navarrete-Vázquez, G.; Estrada-Soto, S. Depressant effects of Agastache mexicana methanol extract and one of major metabolites tilianin. Asian Pac. J. Trop. Med. 2015, 8, 185–190. [Google Scholar] [CrossRef] [Green Version]
- Jiang, H.; Fang, J.; Xing, J.; Wang, L.; Wang, Q.; Wang, Y.; Li, Z.; Liu, R. Tilianin mediates neuroprotection against ischemic injury by attenuating CaMKII-dependent mitochondrion-mediated apoptosis and MAPK/NF-κB signaling. Life Sci. 2019, 216, 233–245. [Google Scholar] [CrossRef]
- Zeng, C.; Jiang, W.; Zheng, R.; He, C.; Li, J.; Xing, J. Cardioprotection of tilianin ameliorates myocardial ischemia-reperfusion injury: Role of the apoptotic signaling pathway. PLoS ONE 2018, 13, e0193845. [Google Scholar] [CrossRef] [PubMed]
- Gálvez, J.; Estrada-Reyes, R.; Benítez-King, G.; Araujo, G.; Orozco, S.; Fernández-Mas, R.; Almazán, S.; Calixto, E. Involvement of the GABAergic system in the neuroprotective and sedative effects of acacetin 7-O-glucoside in rodents. Restor. Neurol. Neurosci. 2015, 33, 683–700. [Google Scholar] [CrossRef] [Green Version]
- Greiser, K.H.; Kluttig, A.; Schumann, B.; Kors, J.A.; Swenne, C.A.; Kuss, O.; Werdan, K.; Haerting, J. Cardiovascular disease, risk factors and heart rate variability in the elderly general population: Design and objectives of the CARdiovascular disease, Living and Ageing in Halle (CARLA) Study. BMC Cardiovasc. Disord. 2005, 5, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pashkow, F.J. Oxidative stress and inflammation in heart disease: Do antioxidants have a role in treatment and/or prevention? Int. J. Inflamm. 2011, 2011, 514623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, H.; Zeng, L.; Dong, X.; Guo, S.; Xing, J.; Li, Z.; Liu, R. Tilianin extracted from Dracocephalum moldavica L. induces intrinsic apoptosis and drives inflammatory microenvironment response on pharyngeal squamous carcinoma cells via regulating TLR4 signaling pathways. Front. Pharmacol. 2020, 11, 205. [Google Scholar] [CrossRef]
- Tian, L.; Cao, W.; Yue, R.; Yuan, Y.; Guo, X.; Qin, D.; Xing, J.; Wang, X. Pretreatment with Tilianin improves mitochondrial energy metabolism and oxidative stress in rats with myocardial ischemia/reperfusion injury via AMPK/SIRT1/PGC-1 alpha signaling pathway. J. Pharmacol. Sci. 2019, 139, 352–360. [Google Scholar] [CrossRef]
- Wang, Y.; Yuan, Y.; Wang, X.; Wang, Y.; Cheng, J.; Tian, L.; Guo, X.; Qin, D.; Cao, W. Tilianin post-conditioning attenuates myocardial ischemia/reperfusion injury via mitochondrial protection and inhibition of apoptosis. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 4490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, X.; Cao, W.; Yao, J.; Yuan, Y.; Hong, Y.; Wang, X.; Xing, J. Cardioprotective effects of tilianin in rat myocardial ischemia-reperfusion injury. Mol. Med. Rep. 2015, 11, 2227–2233. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Y.; Cao, W.; Hong, Y.; Guo, X.; Wang, Y.; Wang, Y.; Wang, X.; Hu, P. Tilianin pretreatment prevents myocardial ischemia-reperfusion injury via preservation of mitochondrial function in rat heart. Phytomedicine 2017, 34, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; Li, Y.; Jin, Y.; Chen, Y.; Tian, L.; He, W. Synergistic cardioptotection by tilianin and syringin in diabetic cardiomyopathy involves interaction of TLR4/NF-κB/NLRP3 and PGC1a/SIRT3 pathways. Int. Immunopharmacol. 2021, 96, 107728. [Google Scholar] [CrossRef]
- Castellon, X.; Bogdanova, V. Chronic inflammatory diseases and endothelial dysfunction. Aging Dis. 2016, 7, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nam, K.-w.; Kim, J.; Hong, J.-J.; Choi, J.-H.; Mar, W.; Cho, M.-H.; Kim, Y.-M.; Oh, S.-R.; Lee, H.-k.; Nam, K.-H. Inhibition of cytokine-induced IκB kinase activation as a mechanism contributing to the anti-atherogenic activity of tilianin in hyperlipidemic mice. Atherosclerosis 2005, 180, 27–35. [Google Scholar] [CrossRef]
- Shen, W.; Anwaier, G.; Cao, Y.; Lian, G.; Chen, C.; Liu, S.; Tuerdi, N.; Qi, R. Atheroprotective mechanisms of tilianin by inhibiting inflammation through down-regulating NF-κB pathway and foam cells formation. Front. Physiol. 2019, 10, 825. [Google Scholar] [CrossRef]
- Cao, W.; Hu, N.; Yuan, Y.; Cheng, J.; Guo, X.; Wang, Y.; Wang, X.; Hu, P. Effects of tilianin on proliferation, migration and TGF-β/smad signaling in rat vascular smooth muscle cells induced with angiotensin II. Phytother. Res. 2017, 31, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- Israili, Z.H.; Hernández-Hernández, R.; Valasco, M. The future of antihypertensive treatment. Am. J. Ther. 2007, 14, 121–134. [Google Scholar] [CrossRef]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [Green Version]
- Finlay, B.B.; Falkow, S. Free-form 3-D surface description in multiple scales. Microbiol. Mol. Biol. Rev. 1997, 61, 136–169. [Google Scholar]
- Hernández-Abreu, O.; Castillo-España, P.; León-Rivera, I.; Ibarra-Barajas, M.; Villalobos-Molina, R.; González-Christen, J.; Vergara-Galicia, J.; Estrada-Soto, S. Antihypertensive and vasorelaxant effects of tilianin isolated from Agastache mexicana are mediated by NO/cGMP pathway and potassium channel opening. Biochem. Pharmacol. 2009, 78, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Carmona-Castro, G.; Estrada-Soto, S.; Arellano-García, J.; Arias-Duran, L.; Valencia-Díaz, S.; Perea-Arango, I. High accumulation of tilianin in in-vitro cultures of Agastache mexicana and its potential vasorelaxant action. Mol. Biol. Rep. 2019, 46, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Abreu, O.; Durán-Gómez, L.; Best-Brown, R.; Villalobos-Molina, R.; Rivera-Leyva, J.; Estrada-Soto, S. Validated liquid chromatographic method and analysis of content of tilianin on several extracts obtained from Agastache mexicana and its correlation with vasorelaxant effect. J. Ethnopharmacol. 2011, 138, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; El-Din, T.M.G.; Swanson, T.M.; Pryde, D.C.; Scheuer, T.; Zheng, N.; Catterall, W.A. Structural basis for inhibition of a voltage-gated Ca2+ channel by Ca2+ antagonist drugs. Nature 2016, 537, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Deedwania, P. The Role of Angiotensin Receptor Blockers in Cardiovascular Protection Beyond Blood Pressure Control. US Cardiol. 2006, 3, 37–39. [Google Scholar] [CrossRef]
- Asada, H.; Inoue, A.; Kadji, F.M.N.; Hirata, K.; Shiimura, Y.; Im, D.; Shimamura, T.; Nomura, N.; Iwanari, H.; Hamakubo, T. The crystal structure of angiotensin II type 2 receptor with endogenous peptide hormone. Structure 2020, 28, 418–425.e4. [Google Scholar] [CrossRef]
- Hahn, V.S.; Zhang, K.W.; Sun, L.; Narayan, V.; Lenihan, D.J.; Ky, B. Heart failure with targeted cancer therapies: Mechanisms and cardioprotection. Circ. Res. 2021, 128, 1576–1593. [Google Scholar] [CrossRef]
- Wiseman, D.N.; Samra, N.; Román Lara, M.M.; Penrice, S.C.; Goddard, A.D. The Novel Application of Geometric Morphometrics with Principal Component Analysis to Existing G Protein-Coupled Receptor (GPCR) Structures. Pharmaceuticals 2021, 14, 953. [Google Scholar] [CrossRef]
- Bitencourt-Ferreira, G.; de Azevedo, W.F. Molegro virtual docker for docking. In Docking Screens for Drug Discovery; Springer: Berlin/Heidelberg, Germany, 2019; pp. 149–167. [Google Scholar]
- EPA. User’s Guide for T.E.S.T. (version 5.1) (Toxicity Estimation Software Tool): A Program to Estimate Toxicity from Molecular Structure; EPA: Cincinnati, OH, USA, 2020. [Google Scholar]
- Yuan, Y.; Wang, X.; Chen, W.; Hong, Y.; Chen, Q. Pharmacokinetics and bioavailability of tilianin microemulsion in rats. Chin. J. Hosp. Pharm. 2015, 35, 1815–1819. [Google Scholar]
- NIPER. Drug Likeness Tool (DruLiTo). Available online: http://www.niper.gov.in/pi_dev_tools/DruLiToWeb/DruLiTo_Reference.html (accessed on 24 September 2021).
- Wang, Y.; Wang, Y.; Wang, X.; Hu, P. Tilianin-loaded reactive oxygen species-scavenging nano-micelles protect H9c2 cardiomyocyte against hypoxia/reoxygenation-induced injury. J. Cardiovasc. Pharmacol. 2018, 72, 32–39. [Google Scholar] [CrossRef]
- Zielińska, S.; Matkowski, A. Phytochemistry and bioactivity of aromatic and medicinal plants from the genus Agastache (Lamiaceae). Phytochem. Rev. 2014, 13, 391–416. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.W.; Ryu, H.W.; Baek, S.C.; Kang, M.-G.; Park, D.; Han, H.-Y.; An, J.H.; Oh, S.-R.; Kim, H. Potent inhibitions of monoamine oxidase A and B by acacetin and its 7-O-(6-O-malonylglucoside) derivative from Agastache rugosa. Int. J. Biol. Macromol. 2017, 104, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Chaurasiya, N.D.; Zhao, J.; Pandey, P.; Doerksen, R.J.; Muhammad, I.; Tekwani, B.L. Selective inhibition of human monoamine oxidase B by acacetin 7-methyl ether isolated from turnera diffusa (Damiana). Molecules 2019, 24, 810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, N.; He, C.; Awuti, G.; Zeng, C.; Xing, J.; Huang, W. Simultaneous determination of six active compounds in Yixin Badiranjibuya granules, a traditional Chinese medicine, by RP-HPLC-UV method. J. Anal. Methods Chem. 2015, 2015, 974039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mas-Capdevila, A.; Teichenne, J.; Domenech-Coca, C.; Caimari, A.; Del Bas, J.M.; Escoté, X.; Crescenti, A. Effect of hesperidin on cardiovascular disease risk factors: The role of intestinal microbiota on hesperidin bioavailability. Nutrients 2020, 12, 1488. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.; Wu, Q.-Q.; Xiao, Y.; Jiang, X.-H.; Yuan, Y.; Zeng, X.-F.; Tang, Q.-Z. Acacetin protects against cardiac remodeling after myocardial infarction by mediating MAPK and PI3K/Akt signal pathway. J. Pharmacol. Sci. 2017, 135, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Bonferoni, M.C.; Rossi, S.; Sandri, G.; Ferrari, F. Nanoparticle formulations to enhance tumor targeting of poorly soluble polyphenols with potential anticancer properties. Semin. Cancer Biol. 2017, 46, 205–214. [Google Scholar] [CrossRef]
- Lagoa, R.; Silva, J.; Rodrigues, J.R.; Bishayee, A. Advances in phytochemical delivery systems for improved anticancer activity. Biotechnol. Adv. 2020, 38, 107382. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, H.R.; Nedaeinia, R.; Shamloo, A.S.; Nikdoust, S.; Oskuee, R.K. Novel delivery system for natural products: Nano-curcumin formulations. Avicenna J. Phytomedicine 2016, 6, 383. [Google Scholar]
- Siddiqui, I.A.; Sanna, V. Impact of nanotechnology on the delivery of natural products for cancer prevention and therapy. Mol. Nutr. Food Res. 2016, 60, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Su, R.; Nie, S.; Sun, M.; Zhang, J.; Wu, D.; Moustaid-Moussa, N. Application of nanotechnology in improving bioavailability and bioactivity of diet-derived phytochemicals. J. Nutr. Biochem. 2014, 25, 363–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pistollato, F.; Bremer-Hoffmann, S.; Basso, G.; Cano, S.S.; Elio, I.; Vergara, M.M.; Giampieri, F.; Battino, M. Targeting glioblastoma with the use of phytocompounds and nanoparticles. Target. Oncol. 2016, 11, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Zuraini, N.Z.A.; Sekar, M.; Wu, Y.S.; Gan, S.H.; Bonam, S.R.; Rani, N.N.I.M.; Begum, M.Y.; Lum, P.T.; Subramaniyan, V.; Fuloria, N.K. Promising nutritional fruits against cardiovascular diseases: An overview of experimental evidence and understanding their mechanisms of action. Vasc. Health Risk Manag. 2021, 17, 739–769. [Google Scholar] [CrossRef] [PubMed]
- Yap, K.M.; Sekar, M.; Fuloria, S.; Wu, Y.S.; Gan, S.H.; Rani, N.N.I.M.; Subramaniyan, V.; Kokare, C.; Lum, P.T.; Begum, M.Y. Drug delivery of natural products through nanocarriers for effective breast cancer therapy: A comprehensive review of literature. Int. J. Nanomed. 2021, 16, 7891–7941. [Google Scholar] [CrossRef] [PubMed]
- Davatgaran-Taghipour, Y.; Masoomzadeh, S.; Farzaei, M.H.; Bahramsoltani, R.; Karimi-Soureh, Z.; Rahimi, R.; Abdollahi, M. Polyphenol nanoformulations for cancer therapy: Experimental evidence and clinical perspective. Int. J. Nanomed. 2017, 12, 2689. [Google Scholar] [CrossRef] [Green Version]










| Animal, Sex | Model | Dose of Tilianin Dose (mg/kg/Day) | Route of Administration | Duration of Treatment | Mechanism of Action | Therapeutic Effects | References |
|---|---|---|---|---|---|---|---|
| SD rats, male | Isolated heart ischemia/reperfusion | -- | -- | -- | - By inhibiting CaMKII-mediated mitochondrial apoptosis - By inhibiting JNK/NF-κB inflammation | Cardioprotection | Jiang et al. [21] |
| SD rats, male | Myocardial ischemia reperfusion injury | 5 | Intragastic | 7 Days | - By improving mitochondrial energy metabolism - By reducing oxidative stress via AMPK/SIRT1/PGC-1α signaling pathway | Cardioprotection | Tian et al. [22] |
| SD rats, male | Myocardial ischemia reperfusion injury | 2.5, 5, 10 | p.o. | 14 Days | - By activating the PI3K/Akt signalling pathway - By inhibiting myocardial apoptosis | Cardioprotection | Zeng et al. [17] |
| SD rats, male | Myocardial ischemia reperfusion injury | 1.25, 2.5, 5 | p.o. | 7 Days | - By alleviating apoptosis of cardiomyocytes - By protecting myocardium through protection of mitochondria and repression of mitochondrial apoptotic pathways | Cardioprotection | Wang et al. [23] |
| SD rats, male | Myocardial ischemia reperfusion injury | 1.5, 2.5, 5 | p.o. | 7 Days | - By relieving calcium overload - By correcting energy metabolism - By improving endothelial function - By inhibiting cell apoptosis | Cardioprotection | Guo et al. [24] |
| SD rats, male | Myocardial ischemia reperfusion injury | 1.25, 2.5, 5 | p.o. | 7 days | -By raising the levels of ATP of the myocardium - By protecting micro-structures and functions of mitochondria | Cardioprotection | Yuan et al. [25] |
| Ldlr−/− mice, male | High-cholesteroldiet | high-cholesterol diet supplemented with 0.05% (w/w diet) of tilianin | p.o. | 7 weeks | - By inhibiting NF-κB-dependent pro-inflammatory cytokines (TNF-α and IL-1β) - By inhibiting IκB kinase activity | Atheroprotection | Nam et al. [28] |
| SHR rats, Male | Spontaneously hypertensive rats | 50 | p.o. | Single dose | - By endothelium-dependent manner, probably due to NO release - By endothelium-independent pathway by opening up K+ channels | Anti-hypertensive | Hernández-Abreu et al. [34] |
| S. No. | Protein Data Bank ID | Name of the Protein | Ligand | MolDock Score | Rerank Score | HBond |
|---|---|---|---|---|---|---|
| 1. | 5KLB | CavAb voltage-gated calcium channel | Tilianin | −106.31 | −96.8228 | −14.7418 |
| Amlodipine | −129.418 | −40.768 | −1.49788 | |||
| Verapamil | −86.916 | −42.9639 | 0 | |||
| 2. | 6JOD | Angiotensin II type 2 receptor | Tilianin | −97.5636 | −87.5858 | −8.44394 |
| Azilsartan | −124.389 | −77.9133 | −9.92896 | |||
| Losartan | −116.448 | −51.6799 | −8.43829 | |||
| 3. | 7BU6 | Human β1 adrenergic receptor | Tilianin | −115.036 | −95.7438 | −5.83387 |
| Nebivolol | −100.61 | −80.3808 | −5.56831 | |||
| Atenolol | −84.7246 | −65.7884 | −6.11871 |
| Property/Rule | Result |
|---|---|
| Molecular formula | C22H22O10 |
| Molecular weight | 446.12 |
| Hydrogen bond donors | 5 |
| Hydrogen bond acceptors | 10 |
| Rotatable bonds | 5 |
| Log P (Partition coefficient, Predicted value) | 0.153 |
| Molar refractivity | 117.89 cm3 |
| Topological polar surface area | 155.14 Å2 |
| Lipinski’s Rule of Five | Passed |
| Unweighted QED | Passed |
| Weighted QED | Passed |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khattulanuar, F.S.; Sekar, M.; Fuloria, S.; Gan, S.H.; Rani, N.N.I.M.; Ravi, S.; Chidambaram, K.; Begum, M.Y.; Azad, A.K.; Jeyabalan, S.; et al. Tilianin: A Potential Natural Lead Molecule for New Drug Design and Development for the Treatment of Cardiovascular Disorders. Molecules 2022, 27, 673. https://doi.org/10.3390/molecules27030673
Khattulanuar FS, Sekar M, Fuloria S, Gan SH, Rani NNIM, Ravi S, Chidambaram K, Begum MY, Azad AK, Jeyabalan S, et al. Tilianin: A Potential Natural Lead Molecule for New Drug Design and Development for the Treatment of Cardiovascular Disorders. Molecules. 2022; 27(3):673. https://doi.org/10.3390/molecules27030673
Chicago/Turabian StyleKhattulanuar, Farrah Syazana, Mahendran Sekar, Shivkanya Fuloria, Siew Hua Gan, Nur Najihah Izzati Mat Rani, Subban Ravi, Kumarappan Chidambaram, M. Yasmin Begum, Abul Kalam Azad, Srikanth Jeyabalan, and et al. 2022. "Tilianin: A Potential Natural Lead Molecule for New Drug Design and Development for the Treatment of Cardiovascular Disorders" Molecules 27, no. 3: 673. https://doi.org/10.3390/molecules27030673