Fatty-Acid-Rich Agave angustifolia Fraction Shows Antiarthritic and Immunomodulatory Effect
Abstract
:1. Introduction
2. Results
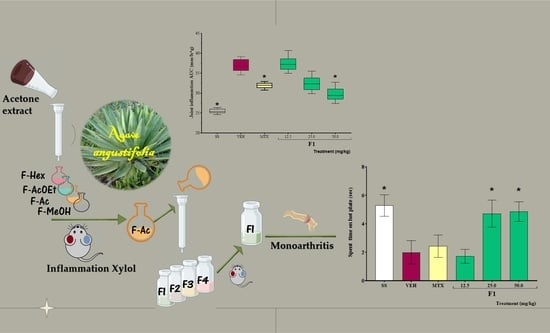
2.1. Chemical Analysis
2.2. Anti-Inflammatory Activity of A. angustifolia Extracts
2.3. Effect of A. angustifolia Extract on Mono-Arthritis Induced by K/C
2.3.1. Effect of A. angustifolia Extract on Cytokine Concentration in Organs from K/C-Treated Mice
2.3.2. Composition of F1
3. Discussion
4. Material and Methods
4.1. Plant Material, Extract, and Fraction Preparation
4.2. Chemical Analysis
4.2.1. Fractioning the Acetone Extract (AaAc)
4.2.2. Separation of Acetone Fraction (F-Ac)
4.2.3. Gas Chromatography–Mass Spectrometry Analysis
4.3. Biological Tests
4.3.1. Animals
4.3.2. Xylene-Induced Mouse Ear Edema
- Δveh = ear weight of VEH group
- Δtr = ear weight of treatments
4.3.3. TPA-Induced Mouse Ear Edema
- Δveh = ear weight VEH group
- Δtr = ear weight of treatment groups
4.3.4. Kaolin/Carrageenan (K/C)-Induced Mono-Arthritis
4.3.5. Thermal Hyperalgesia Assay
4.3.6. Spleen Index
4.3.7. Homogenization of Spleen and Joint Tissues
4.3.8. Quantification of Anti-Inflammatory and Pro-Inflammatory Cytokines
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Jaques-Hernández, C.; Salazar-Bravo, A. Caracterización y usos de las especies de agave en el Estado de Tamaulipas. Cienc. Conoc. Tecnol. 2009, 89, 91–100. [Google Scholar]
- García-Mendoza, A. Los Agaves de México. Ciencias 2007, 8, 14–23. [Google Scholar]
- García-Mendoza, A.; Galván, V. Riqueza de las familias Agavaceae y Nolinaceae en México. Biol. Soc. Bot. Mex. 1995, 56, 7–24. [Google Scholar] [CrossRef] [Green Version]
- Domínguez, M.; González, M.; Rosales, C.; Quiñones, C.; Delgadillo, S.; Mireles, J.; Pérez, E. El cultivo in vitro como herramienta para el aprovechamiento, mejoramiento y conservación de especies del género Agave. Universidad Autónoma de Aguascalientes, Aguascalientes, Mexico. Investig. Cienc. 2008, 16, 53–62. [Google Scholar]
- Herrera-Ruiz, M.; Jiménez-Ferrer, E.; González-Cortazar, M.; Zamilpa, A.; Cardoso-Taketa, A.; Arenas-Ocampo, M.L.; Jiménez-Aparicio, A.R.; Monterrosas-Brisson, N. Potential Use of Agave Genus in Neuroinflammation Management. Plants 2022, 11, 2208. [Google Scholar] [CrossRef]
- Cano, L. Flora Medicinal de Veracruz. In Inventario Etnobotánico; Universidad Veracruzana: Xalapa, Mexico, 1998; Volume 1, pp. 48–49. [Google Scholar]
- Monroy-Ortiz, C.; Castillo-España, P. Agave Angustifolia. In Plantas Medicinales Utilizadas en el estado de Morelos, 1st ed.; Universidad Autónoma del Estado de Morelos: Cuernavaca, Mexico, 2007; Volume 1, pp. 265–266. [Google Scholar]
- López-Romero, J.C.; Ayala-Zavala, J.F.; Peña-Ramos, E.A.; Hernández, J.; González-Ríos, H. Antioxidant and antimicrobial activity of Agave angustifolia extract on overall quality and shelf life of pork patties stored under refrigeration. J. Food Sci. Technol. 2018, 55, 4413–4423. [Google Scholar] [CrossRef] [PubMed]
- El-Hawary, S.; El-Kammar, H.A.; Farag, M.A.; Saleh, D.O.; El Dine, R.H. Metabolomic profiling of five Agave leaf taxa via UHPLC/PDA/ESI-MS inrelation to their anti-inflammatory, immunomodulatory and ulcero-protective activities. Steroids 2020, 160, 108648. [Google Scholar] [CrossRef]
- Rendón-Huerta, J.A.; Juárez-Flores, B.; Pinos-Rodríguez, J.M.; Aguirre-Rivera, J.R.; Delgado-Portales, R.E. Effects of different sources of fructans on body weight, blood metabolites and fecal bacteria in normal and obese non-diabetic and diabetic rats. Plant Foods Hum. Nutr. 2012, 67, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Santiago-García, P.A.; López, M.G. Agavins from Agave angustifolia and Agave potatorum affect food intake, body weight gain and satiety-related hormones (GLP-1 and ghrelin) in mice. Food Funct. 2014, 5, 3311–3319. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y. Rheumatoid Arthritis. Inflamm. Regen. 2020, 40, 20. [Google Scholar] [CrossRef]
- WHO. Musculoskeletal Conditions. Key Facts. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 3 June 2022).
- Cardiel, M.H.; Rojas-Serrano, J. Community based study to estimate prevalence, burden of illness and help seeking behaviour in rheumatic diseases in Mexico City. A COPCORD study. Clin. Exp. Rheumatol. 2002, 20, 617–624. [Google Scholar]
- Peláez-Ballestas, I.; Sanin, L.H.; Moreno-Montoya, J.; Alvarez-Nemegyei, J.; Burgos-Vargas, R.; Garza-Elizondo, M. Epidemiology of the rheumatic diseases in Mexico. A study of 5 regions based on the COPCORD methodology. J. Rheumatol. 2011, 86, 3–8. [Google Scholar] [CrossRef] [Green Version]
- INEGI. Comunicado de Prensa Núm. 450/20, del 1 Oct 2020, Pages 1/3. Available online: https://www.inegi.org.mx/contenidos/saladeprensa/boletines/2020/ENASEM/Enasem_Nal20.pdf (accessed on 4 April 2022).
- Tu, J.; Hong, W.; Guo, Y.; Zhang, P.; Fang, Y.; Wang, X.; Chen, X.; Lu, S.; Wei, W. Ontogeny of synovial macrophages and the roles of synovial macrophages from different origins in arthritis. Front. Immunol. 2019, 10, 1146. [Google Scholar] [CrossRef]
- Kalliolias, G.D.; Ivashkiv, L.B. TNF biology, pathogenic mechanisms and emerging therapeutic strategies. Nat. Rev. Rheumatol. 2016, 12, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, K.; Takayanagi, H. Osteoimmunology. Cold Spring Harb. Perspect. Med. 2019, 9, a031245. [Google Scholar] [CrossRef]
- Lubberts, E. The IL-23-IL-17 axis in inflammatory arthritis. Nat. Rev. Rheumatol. 2015, 11, 415–429. [Google Scholar] [CrossRef]
- Burska, A.N.; Neilan, J.; Chisman, R.E.; Pitaksalee, R.; Hodgett, R.; Marzo-Ortega, H.; Conaghan, P.G.; West, R.; Emery, P.; Ponchel, F. Serum IL-7 as diagnostic biomarker for rheumatoid arthritis, validation with EULAR 2010 classification criteria. Clin. Exp. Rheumatol. 2018, 36, 115–120. [Google Scholar] [PubMed]
- Lopez-Castejon, G.; Brough, D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011, 22, 189–195. [Google Scholar] [CrossRef]
- Bober, L.A.; Rojas-Riana, A.; Jackson, J.V.; Leach, M.W.; Manfra, D.; Narula, S.K.; Grace, M.J. Regulatory effects of interleukin-4 and interleukin-10 on human neutrophil function ex vivo and on neutrophil influx in a rat model of arthritis. Arthritis Rheum. 2000, 43, 2660–2667. [Google Scholar] [CrossRef]
- Smallie, T.; Ricchetti, G.; Horwood, N.J.; Feldmann, M.; Clark, A.R.; Williams, L.M. IL-10 inhibits transcription elongation of the human TNF gene in primary macrophages. J. Exp. Med. 2010, 207, 2081–2088. [Google Scholar] [CrossRef] [Green Version]
- Cardiel, M.H.; Díaz-Borjón, A.; Espinosa, M.V.D.M. Update of the Mexican College of Rheumatology guidelines for the pharmacologic treatment of rheumatoid arthritis. Reumatol. Clin. 2014, 10, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.W.; Liu, C.Z.; Cao, D.; Chen, P.Y.; Chen, M.-F.; Lin, S.Z.; Mozayan, M.; Chen, A.F.; Premkumar, L.S.; Torry, D.S.; et al. Endogenous methyl palmitate modulates nicotinic receptor-mediated transmission in the superior cervical ganglion. Proc. Natl. Acad. Sci. USA 2008, 105, 19526–19531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Demerdash, E. Anti-inflammatory and antifibrotic effects of methyl palmitate. Toxicol. Appl. Pharmacol. 2011, 254, 238–244. [Google Scholar] [CrossRef]
- Saeed, N.M.; El-Demerdash, E.; Abdel-Rahman, H.M.; Algandaby, M.M.; Al-Abbasi, F.A.; Abdel-Naim, A.B. Anti-inflammatory activity of methyl palmitate and ethyl palmitate in different experimental rat models. Toxicol. Appl. Pharmacol. 2012, 264, 84–93. [Google Scholar] [CrossRef]
- Ethyl Palmitate. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Ethyl-palmitate (accessed on 30 March 2022).
- Ye, S.; Zhong, J.; Huang, J.; Chen, L.; Yi, L.; Li, X.; Lv, J.; Miao, J.; Li, H.; Chen, D.; et al. Protective effect of plastrum testudinis extract on dopaminergic neurons in a Parkinson’s disease model through DNMT1 nuclear translocation and SNCA’s methylation. Biomed. Pharmacother. 2021, 141, 111832. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Seetharaman, R.; JungKo, M.; Kim, D.Y.; Kim, T.H.; Yoon, M.K.; Kwak, J.H.; Lee, S.J.; Bae, Y.S.; Choi, Y.W. Ethyl linoleate from garlic attenuates lipopolysaccharide-induced pro-inflammatory cytokine production by inducing heme oxygenase-1 in RAW264.7 cells. Int. Immunopharmacol. 2014, 19, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Monterrosas-Brisson, N.; Ocampo, M.L.; Jiménez-Ferrer, E.; Jiménez-Aparicio, A.R.; Zamilpa, A.; Gonzalez-Cortazar, M.; Tortoriello, J.; Herrera-Ruiz, M. Anti-inflammatory activity of different agave plants and the compound cantalasaponin-1. Molecules 2013, 18, 8136–8146. [Google Scholar] [CrossRef]
- Hernández-Valle, E.; Herrera-Ruiz, M.; Salgado, G.R.; Zamilpa, A.; Ocampo, M.L.; Aparicio, A.J.; Tortoriello, J.; Jiménez-Ferrer, E. Anti-inflammatory effect of 3-O-[(6′-O-palmitoyl)-beta-D-glucopyranosyl sitosterol] from Agave angustifolia on ear e in mice. Molecules 2014, 19, 15624–15637. [Google Scholar] [CrossRef] [Green Version]
- Bautista, D.M.; Jordt, S.E.; Nikai, T.; Tsuruda, P.R.; Read, A.J.; Poblete, J.; Yamoah, E.N.; Basbaum, A.I.; Julius, D. TRPA1 Mediates the Inflammatory Actions of Environmental Irritants and Proalgesic Agents. Cell 2006, 124, 1269–1282. [Google Scholar] [CrossRef] [Green Version]
- Norões, M.M.; Santos, L.G.; Gavioli, E.C.; Rachetti, V.D.P.S.; Otuki, M.F.; de Almeida Cabrini, D.; da Silveira Prudente, A.; Oliveira, J.R.J.M.; de Carvalho Gonçalves, M.; Ferreira, J.; et al. Role of TRPA1 receptors in skin inflammation induced by volatile chemical irritants in mice. Eur. J. Pharmacol. 2019, 858, 172460. [Google Scholar] [CrossRef]
- Bellono, N.W.; Kammel, L.G.; Zimmerman, A.L.; Oancea, E. UV light phototransduction activates transient receptor potential A1 ion channels in human melanocytes. Proc. Natl. Acad. Sci. USA 2013, 110, 2383–2388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bíró, T.; Kovács, L. An ice-Cold TR(i)P to skin biology: The role of TRPA1 in human epidermal keratinocytes. J. Investig. Dermatol. 2009, 129, 2096–2209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyeong-Dong, K.; Hyung-Rae, C.; Seung-Bae, M.; Hyun-Dong, S.; Kun-Ju, Y.; Bok-Ryeon, P.; Hee-Jeong, J.; Lin-Su, K.; Hyeung-Sik, L.; Sae-Kwang, K. Effects of beta-glucan from Aureobasidium pullulans on acute inflammation in mice. Arch. Pharm. Res. 2007, 30, 323–328. [Google Scholar]
- Eidi, A.; Oryan, S.; Zaringhalam, J.; Rad, M. Antinociceptive and anti-inflammatory effects of the aerial parts of Artemisia dracunculus in mice. Pharm. Biol. 2016, 54, 549–554. [Google Scholar] [CrossRef] [Green Version]
- Othman, A.R.; Abdullah, N.; Ahmad, S.; Ismail, I.S.; Zakaria, M.P. Elucidation of in-vitro anti-inflammatory bioactive compounds isolated from Jatropha curcas L. plant root. BMC Complement. Altern. Med. 2015, 15, 11–21. [Google Scholar] [CrossRef]
- Huebner, S.M.; Campbell, J.P.; Butz, D.E.; Fulmer, T.G.; Gendron-Fitzpatrick, A.; Cook, M.E. Individual isomers of conjugated linoleic acid reduce inflammation associated with established collagen-induced arthritis in DBA/1 mice. J. Nutr. 2010, 140, 1454–1461. [Google Scholar] [CrossRef] [Green Version]
- Muhlenbeck, J.A.; Olson, J.M.; Hughes, A.B.; Cook, M.E. Conjugated Linoleic Acid Isomers Trans-10, Cis-12 and Cis-9, Trans-11 Prevent Collagen-Induced Arthritis in a Direct Comparison. Lipids 2018, 53, 689–698. [Google Scholar] [CrossRef]
- Schaible, H.G. Nociceptive neurons detect cytokines in arthritis. Arthritis Res. Ther. 2014, 16, 470. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, M.D.; Bobinski, F.; Sato, K.L.; Kolker, S.J.; Sluka, K.A.; Santos, A.R. IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol. Neurobiol. 2015, 51, 19–31. [Google Scholar] [CrossRef] [Green Version]
- Gárbor, M. 12-O-tetradecanoylphorbol-13-acetate ear oedema (TPA). In Mouse Ear Inflammation Models and Their Pharmacological Applications; Gárbor, M., Ed.; Hungarian Academy of Sciences: Budapest, Hungary, 2000; pp. 28–33. [Google Scholar]
- Gómez-Rivera, A.; González-Cortazar, M.; Gallegos-García, A.J.; Escobar-Ramos, A.; Flores-Franco, G.; Lobato-García, C. Spasmolytic, anti-inflammatory, and antioxidant activities of Salvia gesneriflora Lindley. Afr. J. Tradit. Complement. Altern. Med. 2018, 15, 78–82. [Google Scholar] [CrossRef] [Green Version]
- Gutiérrez-Román, A.S.; Trejo-Tapia, G.; González-Cortazar, M.; Jiménez-Ferrer, E.; Trejo-Espino, J.L.; Zamilpa, A.; Ble-González, E.; Camacho-Díaz, B.H.; Herrera-Ruiz, M. Anti-arthritic and anti-inflammatory effects of Baccharis conferta Kunth in a kaolin/carrageenan-induced monoarthritis model. J. Ethnopharmacol. 2022, 288, 114996. [Google Scholar] [CrossRef] [PubMed]
- Neugebauer, V.; Han, J.S.; Adwanikar, H.; Fu, Y.; Ji, G. Techniques for assessing knee joint pain in arthritis. Mol. Pain 2007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sluka, K.A.; Bailey, K.; Bogush, J.; Olson, R.; Ricketts, A. Treatment with either high or low frequency TENS reduces the secondary hyperalgesia observed after injection of kaolin and carrageenan into the knee joint. Pain 1998, 77, 97–102. [Google Scholar] [CrossRef]
- Langford, D.J.; Mogil, J.S. Pain testing in the laboratory mouse. In Anesthesia and Analgesia in Laboratory Animals; Fish, R.E., Brown, M.J., Danneman, P.J., Karas, A.Z., Eds.; Academic Press: Cambridge, MA, USA, 2008; pp. 549–560. [Google Scholar]
- Martínez-Hernández, G.B.; Vargas-Villa, G.; Jiménez-Ferrer, E.; García-Aguilar, M.P.; Zamilpa, A.; González-Cortazar, M.; Avilés-Flores, M.; Herrera-Ruiz, M. Anti-arthritic and anti- inflammatory effects of extract and fractions of Malva parviflora in a mono- arthritis model induced with kaolin. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2020, 393, 1281–1291. [Google Scholar] [CrossRef] [PubMed]


| Treatment (mg/kg) | Edema (mg) | Inflammation Inhibition (%) |
|---|---|---|
| VEH | 8.87 ± 2.8 | - |
| IND (5.0) | 2.40 ± 1.8 * | 72.9 |
| AaAc (200.0) | 1.52 ± 0.8 * | 82.9 |
| Fractions | ||
| F-Hex (50.0) | 5.36 ± 0.6 * | 39.6 |
| F-AcOEt (50.0) | 5.10 ± 2.2 * | 42.6 |
| F-Ac (50.0) | 4.75 ± 1.6 * | 46.4 |
| F-MeOH (50.0) | 4.50 ± 2.1 * | 49.3 |
| Treatment (mg/ear) | Edema (mg) | Inflammation Inhibition (%) |
|---|---|---|
| VEH | 10.24 ± 2.10 | - |
| IND (1.0) | 1.65 ± 0.21 * | 83.8 |
| F1 (1.0) | 3.06 ± 2.00 * | 70.1 |
| F2 (1.0) | 7.87 ± 0.23 * | 23.1 |
| F3 (1.0) | 6.58 ± 0.51 * | 35.7 |
| F4 (1.0) | 7.08 ± 1.20 * | 30.8 |
| Treatment (mg/kg) | Relative Weight of Spleen (%) |
|---|---|
| SS | 0.552 ± 0.045 * |
| VEH | 0.638 ± 0.035 |
| MTX (1.0) | 0.582 ± 0.050 * |
| F1 (12.5) | 0.573 ± 0.043 * |
| F1 (25.0) | 0.632 ± 0.030 |
| F1 (50.0) | 0.587 ± 0.044 * |
| Treatment (mg/kg) | Cytokine Levels (pg/mg Protein) | |||
|---|---|---|---|---|
| IL-1β | TNF-α | IL-17 | IL-10 | |
| Spleen | ||||
| SS | 15,589.6 ± 3110.3 * | 10,339.97 ± 2379.4 * | 4588.2 ± 253.6 * | 17,474.8 ± 1768.0 * |
| VEH | 20,661.5 ± 1302.9 | 23,015.1 ± 4134.2 | 5917.7 ± 997.5 | 7742.0 ± 3688.6 |
| MTX (1.0) | 18,360.4 ± 1396.1 | 11,751.53 ± 3765.9 * | 5090.7 ± 767.7 | 19,709.9 ± 3429.0 * |
| F1 (12.5) | 18,070.5 ± 596.1 * | 11,547.29 ± 1792.1 * | 5576.8 ± 916.1 | 17,271.0 ± 625.0 * |
| F1 (25.0) | 17,639.1 ± 409.7 * | 12,296.05 ± 1541.5 * | 6291.1 ± 669.0 | 16,670.3 ± 370.5 * |
| F1 (50.0) | 18,481.0 ± 1381.8 | 11,844.34 ± 1669.6 * | 5212.9 ± 738.2 | 17,142.5 ± 1728.8 * |
| Left knee joint | ||||
| SS | 13,883.5 ± 2957.9 | 6808.08 ± 2761.4 * | 1258.7 ± 261.5 * | 15,938.4 ± 1855.6 * |
| VEH | 18,382.1 ± 3616.2 | 10,762.80 ± 564.4 | 2188.5 ± 249.1 | 9832.6 ± 1514.5 |
| MTX (1.0) | 12,242.5 ± 2605.4 | 8080.48 ± 1703.3 * | 1561.2 ± 324.1 * | 13,501.1 ± 1382.2 * |
| F1 (12.5) | 18,807.9 ± 1401.3 | 9569.87 ± 1038.7 | 2337.4 ± 168.6 | 15,803.1 ± 1362.1 * |
| F1 (25.0) | 17,465.7 ± 1398.0 | 9145.84 ± 588.6 * | 1556.8 ± 196.8 * | 15,506.8 ± 1075.4 * |
| F1 (50.0) | 15,112.1 ± 780.9 | 9064.67 ± 313.6 * | 1713.1 ± 232.5 | 14,851.6 ± 989.2 * |
| RT (min) | Fatty Acid Name | Composition (%) | General Data |
|---|---|---|---|
| 18.71 | Palmitic acid, methyl ester (methyl palmitate) | 20 | A C16 saturated fatty acid, a natural product with a vasodilator effect on rat/rabbit thoracic aorta [26]; anti-inflammatory activity in different assays [27,28] |
| 19.32 | Palmitic acid, ethyl ester (ethyl palmitate) | 10 | Ethyl hexadecanoate is a long-chain fatty acid ethyl ester resulting from the formal condensation of the carboxy group of palmitic acid with the hydroxy group of ethanol; it has a role as a plant metabolite; anti-inflammatory activity in different assays [27,28,29] |
| 20.43 | Octadecenoic acid, methyl ester (methyl octadecenoate or ethyl stearate) | 35 | This aliphatic-chain fatty acid had a neuroprotective effect on dopaminergic cells in a model of Parkinson’s disease [30] |
| 20.93 | Linoleic acid, ethyl ester (ethyl linoleate) | 13 | An essential fatty acid, which among other things reduces the levels of nitric oxide and PGE2 by downregulating the enzymes involved in their production (iNOS and COX-2) [31] |
| 20.98 | Oleic acid, ethyl ester (ethyl oleate) | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-Ferrer, E.; Vargas-Villa, G.; Martínez-Hernández, G.B.; González-Cortazar, M.; Zamilpa, A.; García-Aguilar, M.P.; Arenas-Ocampo, M.L.; Herrera-Ruiz, M. Fatty-Acid-Rich Agave angustifolia Fraction Shows Antiarthritic and Immunomodulatory Effect. Molecules 2022, 27, 7204. https://doi.org/10.3390/molecules27217204
Jiménez-Ferrer E, Vargas-Villa G, Martínez-Hernández GB, González-Cortazar M, Zamilpa A, García-Aguilar MP, Arenas-Ocampo ML, Herrera-Ruiz M. Fatty-Acid-Rich Agave angustifolia Fraction Shows Antiarthritic and Immunomodulatory Effect. Molecules. 2022; 27(21):7204. https://doi.org/10.3390/molecules27217204
Chicago/Turabian StyleJiménez-Ferrer, Enrique, Gabriela Vargas-Villa, Gabriela Belen Martínez-Hernández, Manases González-Cortazar, Alejandro Zamilpa, Maribel Patricia García-Aguilar, Martha Lucía Arenas-Ocampo, and Maribel Herrera-Ruiz. 2022. "Fatty-Acid-Rich Agave angustifolia Fraction Shows Antiarthritic and Immunomodulatory Effect" Molecules 27, no. 21: 7204. https://doi.org/10.3390/molecules27217204