Progress and Recent Advances in Solid Organ Transplantation
A topical collection in Transplantology (ISSN 2673-3943). This collection belongs to the section "Solid Organ Transplantation".
Viewed by 37239Editors
Interests: artificial intelligence; machine Learning; nephrology; acute kidney injury; clinical nephrology; kidney transplantation
Special Issues, Collections and Topics in MDPI journals
Interests: artificial Intelligence; machine learning; meta-analysis; acute kidney injury; clinical nephrology; kidney transplantation
Special Issues, Collections and Topics in MDPI journals
Interests: machine learning; kidney transplantation; observational studies; statistical analysis; epidemiology
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
There have been significant improvements in the short-term survival following solid organ transplantation due to advances in immunosuppression and transplant techniques. However, long-term graft survival has lagged relatively behind and has now become one of the main problems in solid organ transplantation.
In this Topical Collection, we are making a call to action to stimulate researchers and clinicians to submit their invaluable studies of solid organ transplantation, including issues related to donors, allograft, and patient survival following transplantation that will provide additional knowledge and skills in the field of transplantation research, ultimately to improve outcomes after solid organ transplantation. Original investigations, review articles, as well as short communications are especially welcome.
Potential topics include, but are not limited to, the following:
Advances in kidney transplant immunosuppression;
Advances in pancreas transplant immunosuppression;
Advances in liver transplantation;
Advances in heart transplantation;
Advances in lung transplantation;
Advances in kidney procurement and transplantation;
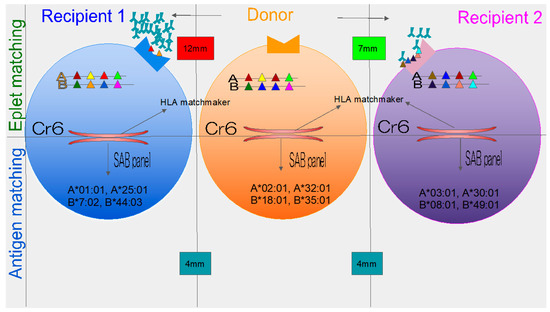
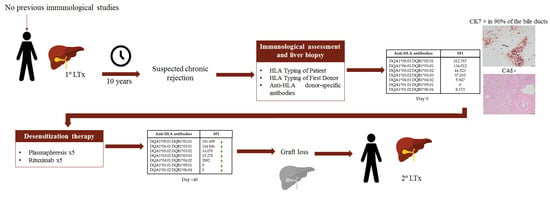
Antibody-mediated rejection: new approaches to prevention and management;
APOL1 genotype and kidney transplantation outcomes;
BK virus nephropathy and kidney transplantation;
Bone disease after kidney transplantation;
Cardiovascular complications after renal transplantation;
Cell-free DNA and active rejection in solid organ allografts;
Clinical outcomes of kidney transplantation in older end-stage renal disease patients;
Donor-specific antibody and graft outcomes in kidney transplant recipients;
Evaluation of the living kidney donor candidate;
Infectious complications after solid organ transplantation;
Combined liver-kidney transplantation;
Management of acute rejection of solid organ transplant;
Pancreas and kidney transplants: new lease on life;
Pediatric kidney transplantation in the new era;
Post-transplantation diabetes in solid organ transplant recipients;
Post-transplant lymphoproliferative disorder in solid organ transplant recipients;
Recent advances in perioperative management for kidney transplantation;
Recurrent glomerulonephritis after kidney transplantation;
Risks and complications in living kidney donors;
Treatment of chronic antibody-mediated rejection after solid organ transplantation.
Best regards,
Dr. Charat Thongprayoon
Dr. Wisit Cheungpasitporn
Dr. Wisit Kaewput
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Transplantology is an international peer-reviewed open access quarterly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1000 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- transplantation
- kidney transplantation
- liver transplantation
- heart transplantation
- pancreas transplantation
- lung transplantation
- immunosuppression
- kidney donor
- organ procurement
- renal transplantation
- post-transplant lymphoproliferative disorder