Journal Description
Surgical Techniques Development
Surgical Techniques Development
is an international, peer-reviewed, open access journal on the latest progressive techniques and advanced technologies in the field of surgeries, published quarterly online by MDPI (from Volume 11, Issue 1 - 2022).
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Embase, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 32.8 days after submission; acceptance to publication is undertaken in 3.8 days (median values for papers published in this journal in the second half of 2023).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
<0.1 (2022)
Latest Articles
Report on the 11th National Congress AICPE (Associazione Italiana di Chirurgia Plastica Estetica) Held in Rimini, Italy, 12–14 April 2024
Surg. Tech. Dev. 2024, 13(2), 122-161; https://doi.org/10.3390/std13020009 - 22 Apr 2024
Abstract
The annual congress of the Italian Association of Plastic Aesthetic Surgery (AICPE) is one of the most relevant conference meetings in Europe concerning aesthetic plastic surgery as there are a number of participants and a parterre of invited speakers chosen for their renowned
[...] Read more.
The annual congress of the Italian Association of Plastic Aesthetic Surgery (AICPE) is one of the most relevant conference meetings in Europe concerning aesthetic plastic surgery as there are a number of participants and a parterre of invited speakers chosen for their renowned scientific value. [...]
Full article
Open AccessArticle
Anterior Cervical and Upper Thoracic Column Reconstruction Using an Expandable Poly-Ether-Ether-Ketone Vertebral Body Replacement: A Retrospective Single Center Cohort Analysis
by
Martin Štefanides, Katharina A. C. Oswald, Anaïs K. Luyet, Christoph E. Albers, Lorin M. Benneker and Moritz C. Deml
Surg. Tech. Dev. 2024, 13(2), 107-121; https://doi.org/10.3390/std13020008 - 12 Apr 2024
Abstract
►▼
Show Figures
This study aimed to evaluate the safety and efficacy of a novel Poly-Ether-Ether-Ketone (PEEK) expandable vertebral body replacement (VBR) for anterior cervico-thoracic vertebral column reconstruction in patients with metastatic, traumatic, or degenerative diseases. Radiographic and clinical outcomes, as well as complication rates, were
[...] Read more.
This study aimed to evaluate the safety and efficacy of a novel Poly-Ether-Ether-Ketone (PEEK) expandable vertebral body replacement (VBR) for anterior cervico-thoracic vertebral column reconstruction in patients with metastatic, traumatic, or degenerative diseases. Radiographic and clinical outcomes, as well as complication rates, were analyzed in a retrospective analysis of 28 patients (61 ± 13 years; 64% female) who underwent an anterior cervical corpectomy and fusion (ACCF) with the Expandable Corpectomy Device (ECD) from DePuy/Synthes (2011–2020). Correction of the bisegmental kyphotic angle (BKA) was chosen as the primary outcome. Bony fusion, loss of device height, and implant subsidence were evaluated additionally. Clinical outcome was assessed using Odom’s criteria, the numerical pain rating scale (NRS), the American Spinal Injury Association Impairment Scale (AIS), and the Karnofsky Performance Status Scale (KPSS). Our study found a significant improvement in the BKA (12.3° ± 9.6°; p = 0.0002) at the last follow-up with no statistically relevant loss of device height (p = 0.96) or implant subsidence (p = 0.99). Successful bony fusion was observed in all patients. The KPSS significantly improved in patients with a tumorous disease at the time of discharge (p = 0.0009), and the sensation of pain showed significant improvement at six months post-operatively and at the final follow-up (p = 0.004; p = 0.021). However, four patients needed further secondary posterior stabilization, and one ECD was explanted due to a severe surgical site infection after an accidental esophageal lesion. In conclusion, the ECD proofed the radiographic stability for the anterior column reconstruction of the cervico-thoracic spine with significantly improved clinical outcome.
Full article
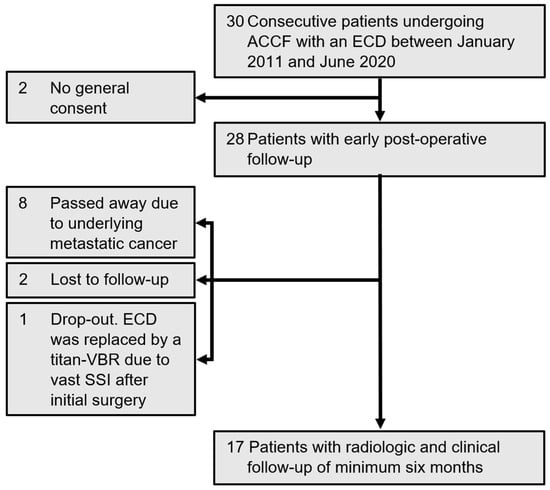
Figure 1
Open AccessTechnical Note
Novel Concept for the Expansion of the Fibula Bone as an Autologous Bone Graft: Experimental Tests on an Animal Implant Prototype—In Memoriam Volker Buehren
by
Matthias Militz, Volker Buehren, Christoph Miethke, Carolin Gabler, Josephine Mauck, Wolfram Mittelmeier, Robert Bialas and Rainer Bader
Surg. Tech. Dev. 2024, 13(2), 97-106; https://doi.org/10.3390/std13020007 - 22 Mar 2024
Abstract
►▼
Show Figures
The current reconstructive surgical procedures implemented after the resection of extended bone segments are associated with high complication rates and long-term treatments. By transplanting an autologous, vascularized and stabilized bone segment, these challenges can be managed. Thus, we propose a novel procedure to
[...] Read more.
The current reconstructive surgical procedures implemented after the resection of extended bone segments are associated with high complication rates and long-term treatments. By transplanting an autologous, vascularized and stabilized bone segment, these challenges can be managed. Thus, we propose a novel procedure to expand the currently available autologous bone grafts to the dimensions of the recipient bone using an implantable device. The objective of the present study was to characterize the feasibility of developing an implant prototype for fibula expansion in an in vitro model using a porcine fibula. A balloon catheter, as the part of the implant responsible for expansion, was proven to expand while being periodically filled with sodium chloride. Therefore, the expansion of the balloon catheter was analyzed in an experimental test setup with a 3D-printed porcine fibula with a closure film simulating callus formation to simulate the in vivo situation. Our experimental testing proved the successful expansion of the porcine fibula by the balloon catheter. Hence, the feasibility of the concept for subsequent animal testing was confirmed.
Full article
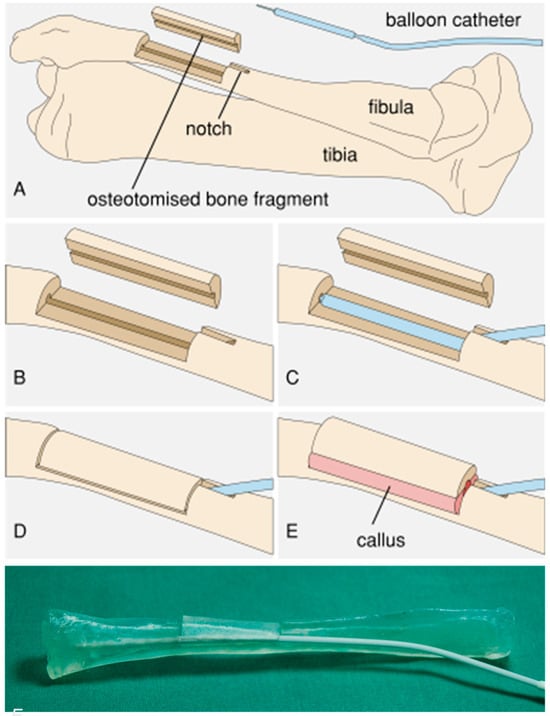
Figure 1
Open AccessArticle
What Are the Risk Factors for Mechanical Failure in Spinal Arthrodesis? An Observational Study
by
Vincenzo Peccerillo, Antonio Culcasi, Riccardo Ruisi, Francesca Amaducci, Maria Grazia Benedetti, Marco Girolami, Andrea Evangelista and Mattia Morri
Surg. Tech. Dev. 2024, 13(1), 87-96; https://doi.org/10.3390/std13010006 - 07 Mar 2024
Abstract
►▼
Show Figures
Background: The aim of this study was to identify the incidence of early mechanical failure in the first post-surgical year in patients who had undergone spinal surgery and to assess the related risk factors. Methods: A retrospective observational study was conducted examining all
[...] Read more.
Background: The aim of this study was to identify the incidence of early mechanical failure in the first post-surgical year in patients who had undergone spinal surgery and to assess the related risk factors. Methods: A retrospective observational study was conducted examining all patients who consecutively underwent arthrodesis surgery. The incidence of postoperative mechanical failure during the first year was calculated as the primary outcome. Results: A total of 237 patients were identified for statistical analysis. The median age of the group of patients was 47 years (IQR of 44), and 66.6% were female. The incidence of mechanical failure in the first postoperative year was 5.1% overall, with 12 events, and the median time between surgery and the need for revision surgery was 5 months (IQR = 7.75). ASA score (OR = 2.39; p = 0.134), duration of the surgical procedure (OR = 1.27; p = 0.118), and inability to walk at discharge (OR = 7.86; p = 0.007) were independent risk factors associated with the mechanical failure. Conclusions: A higher ASA score and longer duration of surgery were risk factors for mechanical failure in the first year in patients who had undergone spinal surgery and must be carefully considered when planning spinal surgery. Early recovery of ambulation must be encouraged to prevent mechanical failure.
Full article
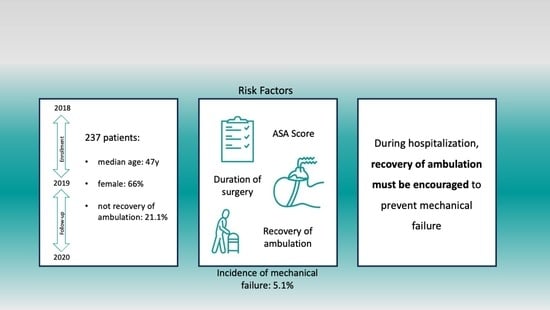
Graphical abstract
Open AccessTechnical Note
A Detailed Exploration of the Ex Utero Intrapartum Treatment Procedure with Center-Specific Advancements
by
Marta Domínguez-Moreno, Ángel Chimenea, María Remedios Viegas-González, Clara Morales-Muñoz, Lutgardo García-Díaz and Guillermo Antiñolo
Surg. Tech. Dev. 2024, 13(1), 76-86; https://doi.org/10.3390/std13010005 - 23 Feb 2024
Abstract
►▼
Show Figures
The Ex Utero Intrapartum Treatment (EXIT) procedure has long been an invaluable tool in managing complex fetal conditions requiring airway interventions during the transition from intrauterine to extrauterine life. This technical note offers an in-depth examination of the EXIT procedure, emphasizing the refinements
[...] Read more.
The Ex Utero Intrapartum Treatment (EXIT) procedure has long been an invaluable tool in managing complex fetal conditions requiring airway interventions during the transition from intrauterine to extrauterine life. This technical note offers an in-depth examination of the EXIT procedure, emphasizing the refinements and innovations introduced at our center. The technique focuses on meticulous preoperative assessment and uses distinctive techniques and anesthetic methodologies. A multidisciplinary team assembles to plan the EXIT procedure, emphasizing patient communication and risk discussion. Our technique involves atraumatic access to the uterine cavity, achieved through the application of a uterine progressive distractor developed for this purpose. Following the use of this distractor, vascular clamps and a stapling device (Premium Poly Cs-57 Autosuture®, Medtronic) are employed. Our anesthetic approach employs general anesthesia with epidural catheter placement. Maternal operation involves low transverse laparotomy and intraoperative ultrasonography-guided hysterotomy. Fetal exposure includes gentle extraction or external version, ensuring airway access. After securing fetal airway access, umbilical cord clamping and maternal abdominal closure conclude the procedure. By revisiting the core principles of EXIT and incorporating center-specific advancements, we enhance our understanding and technical expertise. To our knowledge, this is the first time a detailed description of the technique has been published.
Full article
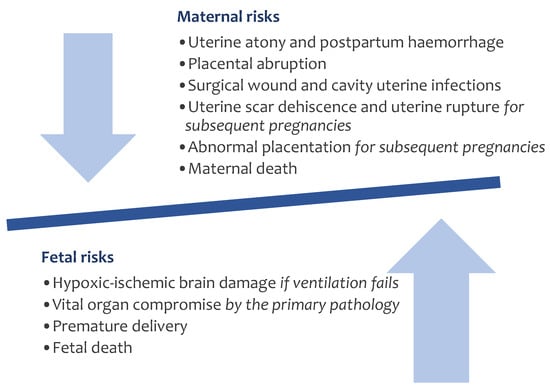
Figure 1
Open AccessArticle
Objective Gait Analysis Using a Single-Point Wearable Sensor to Assess Lumbar Spine Patients Pre- and Postoperatively
by
R Dineth Fonseka, Pragadesh Natarajan, Monish Movin Maharaj, Lianne Koinis, Luke Sy and Ralph Jasper Mobbs
Surg. Tech. Dev. 2024, 13(1), 58-75; https://doi.org/10.3390/std13010004 - 14 Feb 2024
Abstract
►▼
Show Figures
Background: Outcome measurement in lumbar surgery is traditionally performed using patient questionnaires that may be limited by subjectivity. Objective gait analysis may supplement patient assessment but must be clinically viable. We assessed gait metrics in lumbar spine patients pre- and postoperatively using a
[...] Read more.
Background: Outcome measurement in lumbar surgery is traditionally performed using patient questionnaires that may be limited by subjectivity. Objective gait analysis may supplement patient assessment but must be clinically viable. We assessed gait metrics in lumbar spine patients pre- and postoperatively using a small and lightweight wearable sensor. Methods: This was a prospective observational study with intervention including 12 patients undergoing lumbar spine surgery and 24 healthy controls matched based on age and sex. All the subjects underwent gait analysis using the single-point wearable MetaMotionC sensor. The lumbar spine patients also completed traditional patient questionnaires including the Oswestry Disability Index (ODI). Results: The ODI score significantly improved in the patients from the baseline to six weeks postoperatively (42.4 to 22.8; p = 0.01). Simultaneously, the patients demonstrated significant improvements in gait asymmetry (asymmetry in step length, swing time, single support time, and double support time, by 17.4–60.3%; p ≤ 0.039) and variability (variability in gait velocity, step time, step length, stance time, swing time, single support time, and double support time, by 21.0–65.8%; p ≤ 0.023). After surgery, changes in most spatiotemporal (gait velocity, step length, stance time, swing time, and single limb support time) and asymmetry (asymmetry in step time, stance time, swing time, and single limb support time) metrics correlated strongly (magnitude of r = 0.581–0.914) and significantly (p ≤ 0.037) with changes in the ODI. Conclusions: Gait analysis using a single-point wearable sensor can demonstrate objective evidence of recovery in lumbar spine patients after surgery. This may be used as a routine pre- and postoperative assessment during scheduled visits to the clinic.
Full article
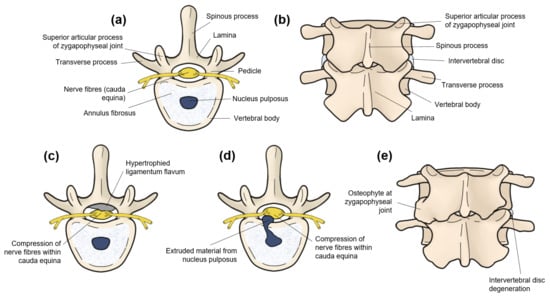
Figure 1
Open AccessSystematic Review
A Comparison of Clinical Outcomes of Robot-Assisted and Conventional Laparoscopic Surgery
by
Storm Chabot, Jean Calleja-Agius and Tim Horeman
Surg. Tech. Dev. 2024, 13(1), 22-57; https://doi.org/10.3390/std13010003 - 31 Jan 2024
Abstract
►▼
Show Figures
Background: Although robot-assisted laparoscopic surgery has become more in popular, it remains unclear what clinical advantages it offers over conventional laparoscopic surgery. Objective: This (systematic) umbrella review aims to synthesize and compare the clinical outcomes of robot-assisted laparoscopic surgery versus conventional laparoscopic surgery.
[...] Read more.
Background: Although robot-assisted laparoscopic surgery has become more in popular, it remains unclear what clinical advantages it offers over conventional laparoscopic surgery. Objective: This (systematic) umbrella review aims to synthesize and compare the clinical outcomes of robot-assisted laparoscopic surgery versus conventional laparoscopic surgery. Methods: A systematic literature search was conducted in PubMed and Scopus. All systematic reviews and meta-analyses published in the past five years that compared the clinical outcomes for cholecystectomy, colectomy, hysterectomy, nephrectomy, and/or prostatectomy were included. The quality of all included reviews was assessed with the AMSTAR 2 quality assessment tool. Each review’s study characteristics and primary sources were extracted, along with the quantitative and qualitative data for blood loss, rate of conversion to open surgery, hospitalization costs, incisional hernia rate, intraoperative complication rate, postoperative complication rate, length of hospital stay, operative time, readmission rate, and wound infection. Results: Fifty-two systematic reviews and (network) meta-analyses were included in this umbrella review, covering more than 1,288,425 patients from 1046 primary sources published between 1996 and 2022. The overall quality of the included reviews was assessed to be low or critically low. Robot-assisted laparoscopic surgery yielded comparable results to conventional laparoscopic surgery in terms of blood loss, conversion to open surgery rate, intraoperative complication rate, postoperative complication rate, readmission rate, and wound infection rate for most surgical procedures. While the hospitalization costs of robot-assisted laparoscopic surgery were higher and the operative times of robot-assisted laparoscopic surgery were longer than conventional laparoscopic surgery, robot-assisted laparoscopic surgery reduced the length of hospital stay of patients in nearly all cases. Conclusion: Robot-assisted laparoscopic surgery achieved comparable results with conventional laparoscopic surgery for cholecystectomy, colectomy, hysterectomy, nephrectomy, and prostatectomy based on ten clinical outcomes.
Full article
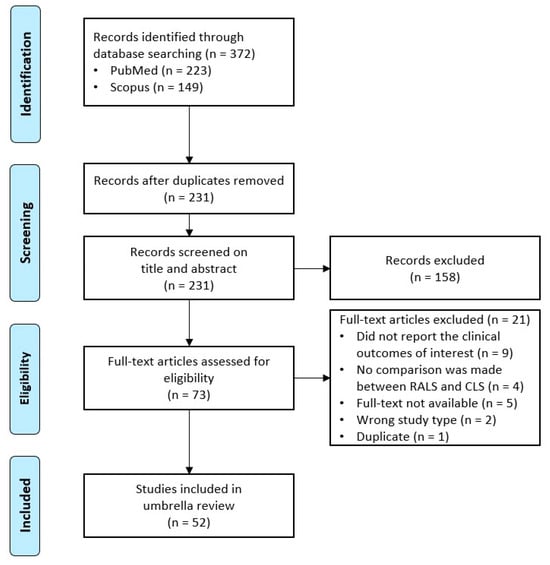
Figure 1
Open AccessSystematic Review
Postoperative Cast Immobilization Might Be Unnecessary after Pelvic Osteotomy for Children with Developmental Hip Dysplasia: A Systematic Review
by
Mohamed Mai, Renée A. van Stralen, Sophie Moerman and Christiaan J. A. van Bergen
Surg. Tech. Dev. 2024, 13(1), 9-21; https://doi.org/10.3390/std13010002 - 15 Jan 2024
Abstract
►▼
Show Figures
Background: Developmental dysplasia of the hip (DDH) is a common disorder of atypical hip development. Pelvic osteotomy (e.g., according to Salter, Pemberton or Dega) may be indicated for children with DDH at walking age. The most popular postoperative treatment is a hip spica
[...] Read more.
Background: Developmental dysplasia of the hip (DDH) is a common disorder of atypical hip development. Pelvic osteotomy (e.g., according to Salter, Pemberton or Dega) may be indicated for children with DDH at walking age. The most popular postoperative treatment is a hip spica cast. Alternative postoperative options include abduction braces and non-weightbearing protocols combined with physical therapy. The aim of this systematic review was to determine the most effective form of postoperative treatment after unilateral pelvic osteotomy in children with DDH in terms of clinical and radiological outcomes and complications. Methods: A systematic review was conducted and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis 2020 guidelines and registered in the international prospective register of systematic reviews. Articles were selected from PubMed, Embase and Cochrane databases. The quality of all (non-)randomized included studies was assessed using the Methodological Index for Non-Randomized Studies (MINORS) criteria. Results: The search strategy yielded 3524 articles. Fourteen articles with 367 total hips were included in this review. A total of 312 hips were treated with spica casts, 49 with abduction braces and 6 with non-weightbearing protocols. The quality of evidence was moderate (MINORS, 3–12 points). All types of postoperative treatments had good clinical outcomes overall, without secondary displacement of the osteotomy. Clinical outcomes for spica casts were reported according to McKay’s criteria in 135 hips, with 123 excellent and 12 good results. Clinical outcomes for abduction braces showed satisfaction for all parents (49 of 49). The radiological outcome was overall well preserved with any postoperative treatment. There was a higher complication rate with the use of hip spica casts, including avascular necrosis, pain complaints and superficial infections. Conclusion: This systematic review showed no benefit of postoperative spica casts compared with abduction braces and avoidance of weightbearing after simple pelvic osteotomy for residual DDH.
Full article
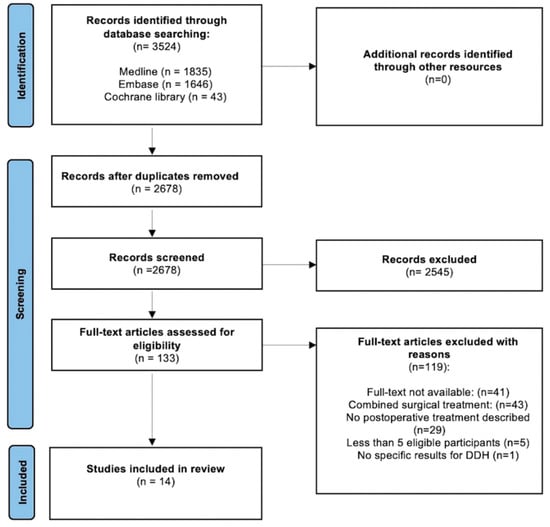
Figure 1
Open AccessCase Report
Ultrasound-Assisted Removal of a Wooden Foreign Body Embedded in the Neck
by
Daniele Vitali, Pietro Orlando, Giandomenico Maggiore, Oreste Gallo and Ilaria Bindi
Surg. Tech. Dev. 2024, 13(1), 1-8; https://doi.org/10.3390/std13010001 - 19 Dec 2023
Abstract
►▼
Show Figures
Objectives: The deep submucosal migration of ingested foreign bodies into the pharyngolaryngeal mucosa is a sporadic event, and its management can be very challenging. In the case of the failure of endoscopic retrieval, open surgical techniques are usually required, and intraoperative ultrasonography can
[...] Read more.
Objectives: The deep submucosal migration of ingested foreign bodies into the pharyngolaryngeal mucosa is a sporadic event, and its management can be very challenging. In the case of the failure of endoscopic retrieval, open surgical techniques are usually required, and intraoperative ultrasonography can become a useful adjunct for identifying their precise localization. Methods: An 84-year-old woman presented with new-onset dysphagia and odynophagia after the accidental ingestion of a fragment of a toothpick a few hours before in the absence of hoarseness or respiratory distress. Ultrasonography and an unenhanced CT scan of the neck revealed a 3 cm linear foreign body embedded into the neck between the left pyriform sinus and the esophageal wall. Results: We report the removal of a fragment of a wooden toothpick deeply lodged between the left pyriform sinus and the esophageal wall, which was managed via an open transcervical approach with the aid of intraoperative ultrasound guidance. Conclusions: We suggest that both preoperative and intraoperative ultrasonography should represent the first-line imaging technique for deeply embedded neck foreign bodies.
Full article
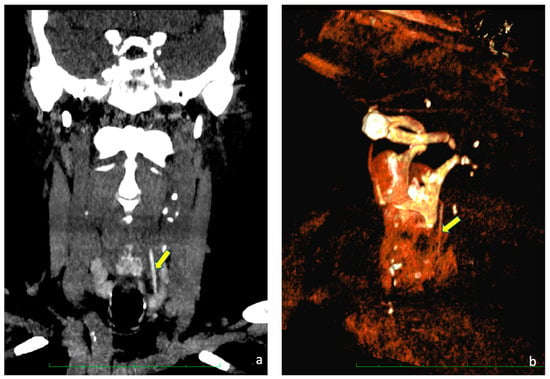
Figure 1
Open AccessReview
Complications Associated with Oblique Lumbar Interbody Fusion: A Systematic Review
by
Quan Rui Tan, Russell Andrew Wong, Arun-Kumar Kaliya-Perumal and Jacob Yoong-Leong Oh
Surg. Tech. Dev. 2023, 12(4), 211-223; https://doi.org/10.3390/std12040020 - 20 Nov 2023
Cited by 1
Abstract
►▼
Show Figures
The main advantage of Oblique Lumbar Interbody Fusion (OLIF) is its ability to provide safe access to the lumbar spine while being a robust interbody fusion technique through a minimally invasive approach. This study reviews the postoperative complications of OLIF, offering a comprehensive
[...] Read more.
The main advantage of Oblique Lumbar Interbody Fusion (OLIF) is its ability to provide safe access to the lumbar spine while being a robust interbody fusion technique through a minimally invasive approach. This study reviews the postoperative complications of OLIF, offering a comprehensive understanding of its advantages and disadvantages. A total of 27 studies with 1275 patients were shortlisted based on our selection criteria. Complications were categorized into intra-operative, immediate post-operative, and delayed post-operative and were interpreted based on surgical procedure into stand-alone OLIF, OLIF with posterior stabilisation, and unspecified. Major complications exhibited a pooled prevalence of just 1.7%, whereas the overall pooled prevalence of complications was 24.7%. Among the subgroups, the stand-alone subgroup had the lowest prevalence of complications (14.6%) compared to the unspecified subgroup (29.6%) and the OLIF L2-5 with posterior stabilisation subgroup (25.8%). Similarly, for major complications, the stand-alone subgroup had the lowest prevalence (1.4%), while the OLIF L2-5 with posterior stabilisation subgroup (1.8%) and the unspecified OLIF L2-5 subgroup (1.6%) had higher rates. However, the differences were not statistically significant. In conclusion, the rate of major complications after OLIF is minimal, making it a safe procedure with significant benefits outweighing the risks. The advantages of OLIF L2-5 with posterior stabilisation over stand-alone OLIF L2-5 is a subject of discussion.
Full article
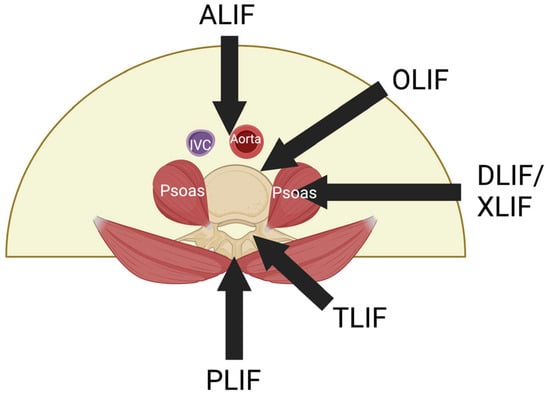
Figure 1
Open AccessCase Report
Anterior Lumbar Interbody Fusion (ALIF) for Lumbar Hemivertebra in an Adult Using Three-Dimensional-Printed Patient-Specific Implants and Virtual Surgery Planning: A Technical Report
by
Tajrian Amin, William C. H. Parr, Pragadesh Natarajan, Andrew Lennox, Lianne Koinis and Ralph J. Mobbs
Surg. Tech. Dev. 2023, 12(4), 199-210; https://doi.org/10.3390/std12040019 - 08 Nov 2023
Abstract
►▼
Show Figures
Introduction: Hemivertebrae are a common defect of vertebral formation, potentially resulting in debilitating congenital scoliosis and necessitating highly traumatic surgery. Virtual surgical planning (VSP) and 3D-printed patient-specific implants (PSIs) have increasingly been applied to complex spinal surgery, and offer a range of potential
[...] Read more.
Introduction: Hemivertebrae are a common defect of vertebral formation, potentially resulting in debilitating congenital scoliosis and necessitating highly traumatic surgery. Virtual surgical planning (VSP) and 3D-printed patient-specific implants (PSIs) have increasingly been applied to complex spinal surgery, and offer a range of potential benefits. Research Question: We report the use of 3D-printed PSIs and VSP as part of a two-level anterior lumbar interbody fusion (ALIF) for the management of lateral hemivertebra and congenital scoliosis. Material and Methods: A 53-year-old male with chronic low-back pain, due to L4 hemivertebra and mild congenital scoliosis, presented with new-onset leg pain. CT revealed L4/5 and L5/S1 degeneration and foraminal stenosis. Given the complex anatomy and extensive multi-level osteophytosis, 3D-printed PSIs were designed, manufactured, and implanted as part of a two-level ALIF. Results: Excellent implant fit was achieved intraoperatively, confirmed via postoperative imaging. VSP assisted with navigating challenging bony and vascular anatomy. Three-month postoperative imaging demonstrated construct stability, early signs of bony fusion, with implant placement, spinal curvature, and disc height corrections closely matching the VSP. Clinically, the patient’s pain and functional impairment had effectively resolved by nine-month follow up, as demonstrated through subjective and objective measures. Discussion and Conclusions: Virtual surgical planning and 3D-printed PSIs can be useful surgical aids in the management of the often-complex cases involving hemivertebrae and congenital scoliosis. This case of congenital pathology adds to the growing reports of PSI application to a variety of complex spinal pathologies, with analyses showing a close match of the postoperative construct to the preoperative VSP.
Full article

Figure 1
Open AccessArticle
Intraoperative Complications of the Anterior Retroperitoneal Approach to the Lumbosacral Spine in the Supine Position: A Proposal for an Algorithm to Predict the Degree of Difficulty of the Surgical Procedure
by
Francesco Caiazzo, Lucas Capo and Juan Bago
Surg. Tech. Dev. 2023, 12(4), 188-198; https://doi.org/10.3390/std12040018 - 19 Oct 2023
Abstract
►▼
Show Figures
The main concern in anterior exposure of the lumbosacral spine is the risk of vascular injury during mobilization and retraction of the blood vessels. Preoperative planning is considered essential to reducing the incidence of vascular injury, although no consensus has been reached on
[...] Read more.
The main concern in anterior exposure of the lumbosacral spine is the risk of vascular injury during mobilization and retraction of the blood vessels. Preoperative planning is considered essential to reducing the incidence of vascular injury, although no consensus has been reached on the preferred methodology for such planning. This is a retrospective study, including all patients operated on by a single surgeon, who received anterior lumbar-spine surgery in the supine position as a primary procedure before undergoing an anterior lumbar interbody fusion (ALIF) or an artificial disc replacement (ADR). The aim of this study was to list the intraoperative complications observed. We included 156 patients (87 women; mean age, 48 years) who met the inclusion criteria. The overall complication rate was 6.4% (10/156). The most frequent complications were an incidental peritoneal opening (seven patients, 4.4%); two left–iliac-vein injuries (1.28%) that were sutured; and one dural tear during a decompression maneuver of the canal. No neurological, arterial, or ureteral injury or retrograde ejaculation was reported. The use of a sound protocol that includes planning, assessment of approach difficulty, and step-by-step surgical technique can reduce the rate of vascular injury in anterior lumbosacral-spine surgery.
Full article
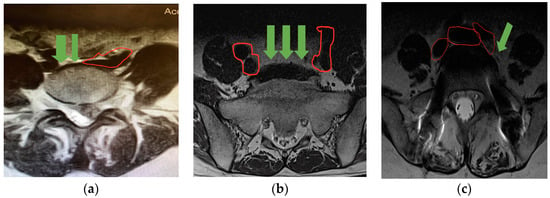
Figure 1
Open AccessArticle
Robotic Liver Resection: Report of Institutional First 100 Cases
by
Maria Conticchio, Antonella Delvecchio, Valentina Ferraro, Matteo Stasi, Annachiara Casella, Rosalinda Filippo, Michele Tedeschi, Alba Fiorentino and Riccardo Memeo
Surg. Tech. Dev. 2023, 12(4), 176-187; https://doi.org/10.3390/std12040017 - 12 Oct 2023
Abstract
►▼
Show Figures
Backgrounds: Liver surgery has developed progressively during the last 10 years, especially in minimally invasive approaches. Robotic surgery seemed to overcome laparoscopic limitations with 3D visualization, the increased degrees of freedom given with Endowrist instruments, tremor filtering, better dexterity, and improved ergonomics for
[...] Read more.
Backgrounds: Liver surgery has developed progressively during the last 10 years, especially in minimally invasive approaches. Robotic surgery seemed to overcome laparoscopic limitations with 3D visualization, the increased degrees of freedom given with Endowrist instruments, tremor filtering, better dexterity, and improved ergonomics for the surgeon. Methods: This work was a retrospective analysis of our first 100 robotic hepatectomies from March 2020 to July 2022. Patient demographics characteristics and intra- and postoperative outcomes were analyzed. Results: A total of 59 males and 41 females, with a median age of 68 years, underwent a robotic liver resection. The indications for robotic liver resections were malignant lesions in 86% of patients. Anatomical resection (AR) was undertaken in 27% of cases and non-anatomical resection (NAR) in 63% of cases. None of the patients were converted to the ‘open’ approach. Postoperative complications were as follows: 1% of biliary leakage, 5% of ascites, 6% of pulmonary infections, and 3% of other sites’ infections. CONCLUSIONS Our results showed the satisfactory experience of a tertiary HPB center with its first 100 robotic liver resections. The opportunity to make the robotic approach routinary provided global growth of a surgical team, improving the quality of patient outcomes.
Full article
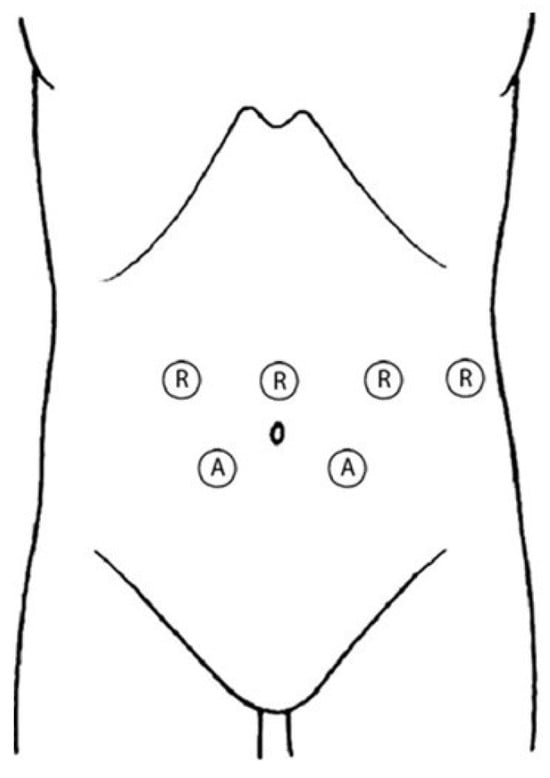
Figure 1
Open AccessArticle
Keystone Flap in Amniotic Band Syndrome—Innovative Approach of an Established Operative Technique for an Unusual Entity
by
Dominik Promny, Raymund E. Horch and Theresa Promny
Surg. Tech. Dev. 2023, 12(4), 164-175; https://doi.org/10.3390/std12040016 - 22 Sep 2023
Abstract
►▼
Show Figures
Amniotic Band Syndrome (ABS) is a complex condition characterized by constricting rings and tissue synechiae, resulting in tissue necrosis and congenital anomalies. In newborns and infants with ABS, tissue necrosis can be profound, requiring a tissue defect reconstruction, realized by a Keystone Perforator
[...] Read more.
Amniotic Band Syndrome (ABS) is a complex condition characterized by constricting rings and tissue synechiae, resulting in tissue necrosis and congenital anomalies. In newborns and infants with ABS, tissue necrosis can be profound, requiring a tissue defect reconstruction, realized by a Keystone Perforator Island Flap (KF). Primarily used for reconstruction after skin cancer excisions, KF’s applications expanded to defects of various etiologies and disorders throughout the body. Subsequently, additional KF types adapted to the particular tissue defects were developed. The KF’s preparation is relatively simple to perform leading to shorter operative times, and the postoperative monitoring is less laborious. Individualized surgical approaches and timing are essential for addressing the varied manifestations of ABS, with immediate treatment recommended for vascular compression, all-layered tissue necrosis, and nerve compression cases. To our knowledge, there is no published case in which a KF was used for the reconstruction of tissue defects and release of constriction rings in the context of an amniotic band syndrome. Therefore, the purpose of this article is to introduce the established surgical technique of KFs as an innovative surgical approach with satisfying reconstructive results for tissue defects and constriction ring release in ABS.
Full article
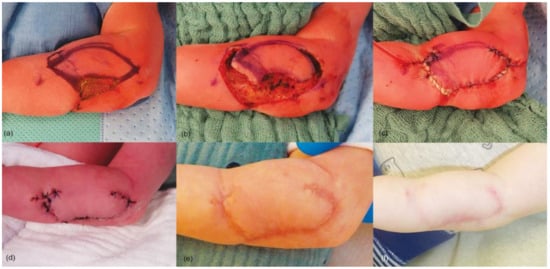
Figure 1
Open AccessCase Report
Anesthetic Management for a Pregnant Patient with Bilateral Vocal Cord Granuloma Using High-Flow Nasal Cannula Oxygenation with Oxygen Reserve Index Monitoring: A Case Report
by
Hyo Sung Kim, Seok Kyeong Oh, Jae Eun Lee, Hyun Ah Lee and Jae Gu Cho
Surg. Tech. Dev. 2023, 12(3), 156-163; https://doi.org/10.3390/std12030015 - 07 Sep 2023
Abstract
►▼
Show Figures
Anesthetic management for pregnant patients suffering from airway pathology poses unique challenges. The presence of a bilateral vocal cord granuloma adds further complexity to anesthetic management as it can potentially cause a compromised airway and respiratory distress. This case presents a pregnant patient
[...] Read more.
Anesthetic management for pregnant patients suffering from airway pathology poses unique challenges. The presence of a bilateral vocal cord granuloma adds further complexity to anesthetic management as it can potentially cause a compromised airway and respiratory distress. This case presents a pregnant patient with a bilateral vocal cord granuloma who underwent anesthesia using high-flow nasal cannula (HFNC) oxygenation and oxygen reserve index (ORi) monitoring. A 33-year-old pregnant woman, who underwent intubation six months ago, experienced hoarseness and was ultimately diagnosed with a bilateral granuloma. Due to the significant airway obstruction, neither intubation nor ventilation was feasible, thereby requiring a surgical intervention. Before the surgical removal, the patient’s oxygenation was ensured using HFNC oxygenation. After confirming the sufficient oxygenation of the patient with an ORi of 0.38, the operation commenced, and as it lasted approximately 3 min, the patient was able to tolerate the brief period without additional oxygen supply. Post-surgical excision, mask bagging, and HFNC oxygenation was resumed, driving the ORi to 0.39; then, the operation was resumed. Throughout the procedure, the SpO2 remained above 98. The combination of HFNC and ORi ensured adequate oxygenation and allowed for the early detection of hypoxemia during the procedure. This approach may be a good option for managing granulomas.
Full article
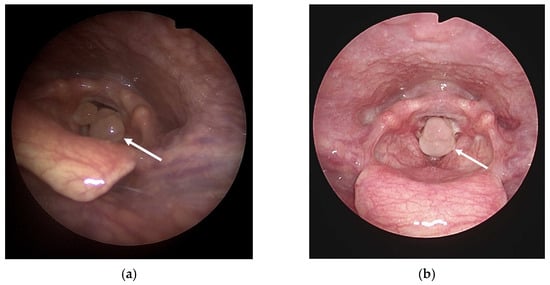
Figure 1
Open AccessArticle
An Evaluation of the Caudal End Deviation of the Nasal Septum Using the Quantitative Analysis of Computed Tomography
by
Tomohisa Hirai, Tsutomu Ueda, Takashi Ishino and Sachio Takeno
Surg. Tech. Dev. 2023, 12(3), 145-155; https://doi.org/10.3390/std12030014 - 24 Aug 2023
Abstract
►▼
Show Figures
Objectives: This study was designed to determine objective surgical indications of correcting caudal end deviation of the nasal septum. Methods: We employed quantitative computed tomographic (CT) analysis and assessed the validity by comparing this with anterior rhinoscopic findings (AR findings). The study population
[...] Read more.
Objectives: This study was designed to determine objective surgical indications of correcting caudal end deviation of the nasal septum. Methods: We employed quantitative computed tomographic (CT) analysis and assessed the validity by comparing this with anterior rhinoscopic findings (AR findings). The study population consisted of 300 patients. The archived CT data were transferred to a workstation, and 3D CT volume-rendered images were generated using computer graphics tools. In the plane of the nostril entrance, we calculated ratios of the cross-sectional area of the convex side (narrower side) and the concave side (wider side), which is abbreviated as the N/W ratio. We also examined the presence of laterality between the right and the left cross-sectional area of the nasal valve based on the AR findings. Surgical procedures for whether to expose the caudal end were planned based on the AR findings and the N/W ratio. Results: A significant correlation was found between the AR findings and the N/W ratio. After surgery, the average N/W ratio improved from 0.53 ± 0.15 to 0.81 ± 0.15, and the average values of VAS scaling for nasal obstruction improved from 8.1 ± 0.2 to 1.0 ± 0.1. Conclusions: The quantitative CT analysis proposed in the study is a useful modality to objectively determine the surgical indications of managing the caudal end of the nasal septum.
Full article
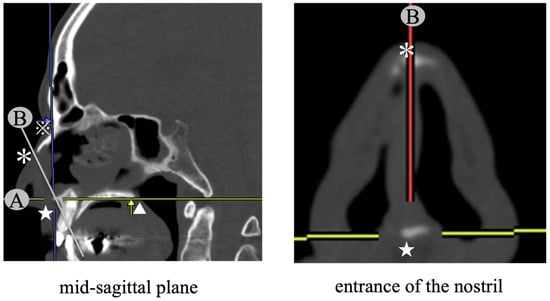
Figure 1
Open AccessArticle
Predictive Factors for Union Time in Adult Diaphyseal Forearm Fractures
by
Shai Factor, Ron Gurel, Gilad Eisenberg, Daniel Tordjman, Yishai Rosenblatt, Tamir Pritsch and Franck Atlan
Surg. Tech. Dev. 2023, 12(3), 135-144; https://doi.org/10.3390/std12030013 - 09 Aug 2023
Abstract
►▼
Show Figures
Purpose: Although open reduction and internal fixation (ORIF) by plating are the treatment of choice for diaphyseal fractures of the forearm, delayed union and non-union remain as existing complications. This study aimed to analyze predictive factors for the union time in diaphyseal fractures
[...] Read more.
Purpose: Although open reduction and internal fixation (ORIF) by plating are the treatment of choice for diaphyseal fractures of the forearm, delayed union and non-union remain as existing complications. This study aimed to analyze predictive factors for the union time in diaphyseal fractures of the forearm. Methods: A retrospective study was conducted on all adult patients with diaphyseal forearm fractures who underwent surgical treatment with plate fixation between 2007 and 2016 at a tertiary care referral center. The patients were divided into two groups based on their union times: ≤3 months or >3 months. They were then compared for demographics, fracture pattern and characteristics, associated injuries, type of fixation, and quality of postoperative reduction. Results: Eighty-six diaphyseal forearm bone fractures (radius, ulna, or both) were observed in 55 adults. Out of these fractures, 55 (65.1%) achieved union within ≤3 months, 26 (30.3%) took more than 3 months to achieve union, and 4 (4.6%) resulted in nonunion. The use of a locking plate in open reduction and internal fixation of diaphyseal forearm fractures significantly increased the likelihood of union within ≤3 months (p = 0.043). The parameter of gap width at the fracture site, as observed on postoperative X-rays, showed a qualitative and quantitative correlation with union time (p = 0.028). Conclusion: The use of a locking plate, combined with reducing the gap width at the fracture site after reduction during open reduction and internal fixation (ORIF) of diaphyseal forearm fractures, is significantly correlated with an increased likelihood of achieving bone union within 3 months.
Full article
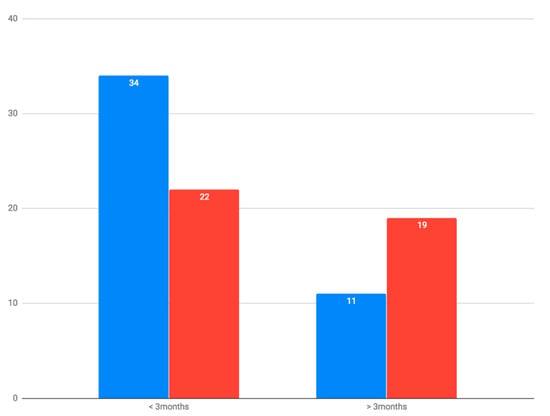
Figure 1
Open AccessCase Report
The Ileojejunal Bypass: The Forgotten Procedure
by
Caroline Mercedes Sobotta, Emre Tanay, Shadi Sued, Christopher Kieninger, Jörg Köninger and Tobias Meile
Surg. Tech. Dev. 2023, 12(3), 126-134; https://doi.org/10.3390/std12030012 - 26 Jul 2023
Abstract
►▼
Show Figures
Since its inception in the early 1970s, bariatric surgery has experienced remarkable advancements, leading to improved patient outcomes. However, amidst these developments, the once-popular ileojejunal bypass procedure has faded into obscurity, along with its associated risks and complications. In this particular case, we
[...] Read more.
Since its inception in the early 1970s, bariatric surgery has experienced remarkable advancements, leading to improved patient outcomes. However, amidst these developments, the once-popular ileojejunal bypass procedure has faded into obscurity, along with its associated risks and complications. In this particular case, we present the medical history of a 68-year-old male who endured prolonged hospitalization due to a myriad of health issues, including malnutrition, kidney stones, chronic kidney disease, and persistent diarrhea following an ileojejunal bypass performed back in 1973. Troublingly, his symptoms were erroneously attributed to other causes for an extended period, overlooking the potential long-term effects of his prior surgery. This case emphasizes the importance of recognizing and monitoring the lasting impacts of historical surgical interventions, as well as the need for heightened vigilance in postoperative care.
Full article

Figure 1
Open AccessCase Report
Achalasia Post-Bariatric Surgery, Placement Roux-En-Y Gastric Bypass: Case Report
by
Juan Pablo Landeros-Ruiz, Lourdes Marlene Zúñiga-Ramos, Daniela Cárdenas-Guerrero and Quitzia Libertad Torres-Salazar
Surg. Tech. Dev. 2023, 12(3), 119-125; https://doi.org/10.3390/std12030011 - 25 Jul 2023
Abstract
►▼
Show Figures
Introduction: Achalasia is a pathology with an incidence of 1 in 100,000 inhabitants per year. There are very limited data on achalasia in the obese population, especially in those undergoing bariatric surgery. The approach of choice for cases of achalasia is the procedure
[...] Read more.
Introduction: Achalasia is a pathology with an incidence of 1 in 100,000 inhabitants per year. There are very limited data on achalasia in the obese population, especially in those undergoing bariatric surgery. The approach of choice for cases of achalasia is the procedure partial fundoplication to correct the reflux; however, lacking a fundus due to a previous gastrectomy, an alternative that offers optimal results should be chosen. Here, we present the surgical approach in a case of esophageal achalasia and a history of vertical sleeve gastrectomy, where we performed a simultaneous Heller’s cardiomyotomy and laparoscopic Roux-en-Y gastric bypass, as well as the results obtained. Case Presentation: A 44-year-old woman with no chronic degenerative diseases, who had a vertical sleeve gastrectomy carried out 5 years ago. Her first symptoms manifested 17 months before, and they were dysphagia to liquids and then to solids, in addition to weight loss of 10 kg in 4 months. Her body mass index before the vertical sleeve gastrectomy was 32 kg/m2; her body mass index at the time of admission was 20 kg/m2; she also presented regurgitation and generalized weakness. After analyzing the surgical options, it was decided to perform a Heller cardiomyotomy and a Roux-en-Y gastric bypass. Discussion and Conclusions: The procedure turned out to be safe and successful in treating achalasia symptomatology, in addition to completely resolving the reflux symptoms.
Full article
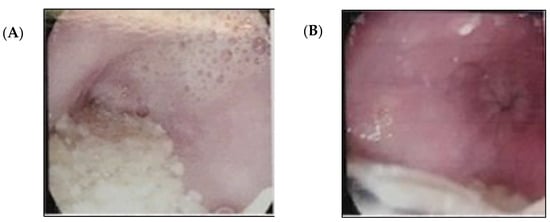
Figure 1
Open AccessArticle
Pediatric Supracondylar Fracture of the Humerus with Sideward Displacement
by
Michael Zaidman, Mark Eidelman, Khaled Abu-Dalu and Pavel Kotlarsky
Surg. Tech. Dev. 2023, 12(3), 107-118; https://doi.org/10.3390/std12030010 - 30 Jun 2023
Abstract
►▼
Show Figures
Background: Supracondylar humeral fracture is probably the most common elbow fracture in children requiring surgical intervention. We observed a subtype of pediatric supracondylar humeral fracture with a sideward translation, without substantial displacement in the sagittal plane on initial radiographs. The purpose of this
[...] Read more.
Background: Supracondylar humeral fracture is probably the most common elbow fracture in children requiring surgical intervention. We observed a subtype of pediatric supracondylar humeral fracture with a sideward translation, without substantial displacement in the sagittal plane on initial radiographs. The purpose of this study was to calculate the incidence of this fracture subtype and suggest a modification to the standard operative technique, to achieve the desired fracture alignment and fixation. Methods: We reviewed the clinical records and radiographs of all pediatric patients with supracondylar humeral fractures surgically treated in our institution between the years 2006 and 2014. The fracture types, fixation configuration and any complications were recorded. Results: Overall, 263 consecutive patients were included. The incidence of supracondylar fracture of the humerus with solely sideward displacement was 6%. The fracture was characterized clinically and radiographically. We proposed a modification to the standard operative technique for this fracture subtype for successful closed reduction and percutaneous pinning. Conclusions: Special attention to this fracture subtype, including appropriate operating room setup and the application of a suitable reduction and pinning technique, has the potential to achieve successful results and avoid the need for open reduction.
Full article
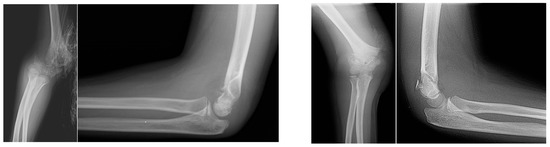
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Surgical Techniques Development
Feature Papers in Spinal Surgery 2024
Guest Editors: Monish Maharaj, Ralph MobbsDeadline: 15 December 2024








