Journal Description
Sinusitis
Sinusitis
(Volume 3, Issue 3 - 2018 was published with Sinusitis and Asthma) is a peer-reviewed, open access journal which focuses on medical research about sinusitis, and is published semiannually online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 34 days after submission; acceptance to publication is undertaken in 6.2 days (median values for papers published in this journal in the second half of 2023).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Sinusitis is a companion journal of JCM.
Latest Articles
Eosinophilic Cationic Protein and Immunoglobulin E: Unraveling Biomarkers in Chronic Pediatric Cough
Sinusitis 2024, 8(1), 1-10; https://doi.org/10.3390/sinusitis8010001 - 27 Feb 2024
Abstract
Although the cough reflex is one of the essential protective mechanisms in the respiratory tract, it is considered a considerable health problem in adults and children when it becomes chronic and hypersensitive. However, the need for biomarkers for chronic cough in children and
[...] Read more.
Although the cough reflex is one of the essential protective mechanisms in the respiratory tract, it is considered a considerable health problem in adults and children when it becomes chronic and hypersensitive. However, the need for biomarkers for chronic cough in children and adults is critical. The problem with cough is also a severe symptom in hypersensitivity children. Respiratory infections are a considerable challenge for pediatricians, especially in allergic children. The term cough hypersensitivity syndrome, although introduced in adults, was questioned for children. Eosinophil cationic protein (ECP) is a promising marker for chronic cough but still needs to be validated and proved in clinical settings. In this review article, we aimed to discuss the possible role of ECP in connection to IgE for chronic cough in children.
Full article
Open AccessReview
Chronic Rhinosinusitis with Nasal Polyposis in People with Cystic Fibrosis
by
Jessa E. Miller, Jennifer L. Taylor-Cousar and Daniel M. Beswick
Sinusitis 2023, 7(2), 27-37; https://doi.org/10.3390/sinusitis7020004 - 31 Oct 2023
Abstract
Cystic fibrosis (CF) is an autosomal recessive disorder that results in deranged ion transport and affects multiple organ systems, including the upper and lower respiratory tracts. People with CF (PwCF) often develop chronic rhinosinusitis (CRS) with or without nasal polyposis. CRS can significantly
[...] Read more.
Cystic fibrosis (CF) is an autosomal recessive disorder that results in deranged ion transport and affects multiple organ systems, including the upper and lower respiratory tracts. People with CF (PwCF) often develop chronic rhinosinusitis (CRS) with or without nasal polyposis. CRS can significantly decrease quality of life for PwCF and can lead to more frequent pulmonary exacerbations. The management of CRS in PwCF is different from that in individuals without CF. Novel therapies have emerged in the last several years that have drastically altered the progression of both pulmonary and sinonasal disease in people with CF. It is critical for providers who manage CF-related CRS to understand the unique characteristics and challenges that coincide with this disease process. This review article aims to provide readers with an overview of the pathophysiology of CF and to summarize best practice strategies for the management of CF-related CRS.
Full article
(This article belongs to the Special Issue Frontiers in Chronic Rhinosinusitis with Nasal Polyposis)
►▼
Show Figures
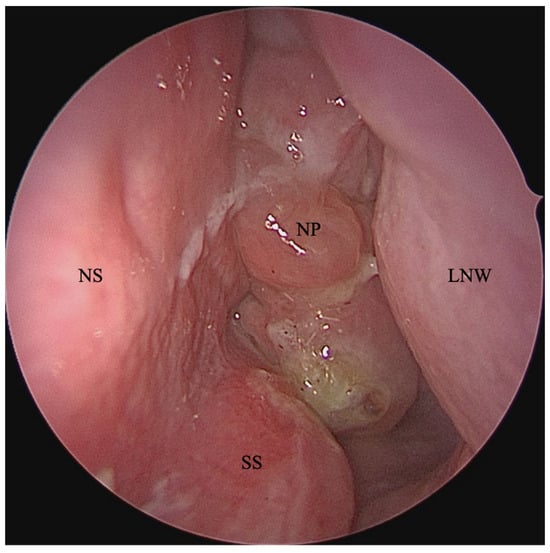
Figure 1
Open AccessReview
Central Compartment Atopic Disease as a Pathophysiologically Distinct Subtype of Chronic Rhinosinusitis: A Scoping Review
by
Camron Davies, Franklin Wu, Emily Y. Huang, Masayoshi Takashima, Nicholas R. Rowan and Omar G. Ahmed
Sinusitis 2023, 7(2), 12-26; https://doi.org/10.3390/sinusitis7020003 - 21 Sep 2023
Abstract
Central compartment atopic disease (CCAD) is a distinct phenotype within chronic rhinosinusitis with nasal polyps (CRSwNP) with a pathophysiology that bridges the gap between allergy and CRSwNP, an association that was previously ambiguous. Understanding this endotype and its link to allergic disease is
[...] Read more.
Central compartment atopic disease (CCAD) is a distinct phenotype within chronic rhinosinusitis with nasal polyps (CRSwNP) with a pathophysiology that bridges the gap between allergy and CRSwNP, an association that was previously ambiguous. Understanding this endotype and its link to allergic disease is crucial for improved CCAD management. Using a systematic search and an independent dual-reviewer evaluation and data extraction process, this scoping review examines the clinical features, management options, and treatment outcomes of CCAD. Central compartment (CC) polypoid changes of the MT predominantly correlate with allergic rhinitis, increased septal inflammation, oblique MT orientation, and decreased nasal cavity opacification and Lund–Mackay scores compared to other CRSwNP subtypes. CCAD patients also exhibit higher rates of asthma, allergen sensitization, and hyposmia or anosmia. Surgical outcomes, including revision rate and SNOT-22 improvement, are favorable in CCAD as well. In conclusion, CCAD primarily affects atopic individuals and is managed using endoscopic sinus surgery combined with treating the underlying allergy. Continued research is needed to further refine understanding and develop optimal treatment strategies of this emerging CRS subtype.
Full article
(This article belongs to the Special Issue Frontiers in Chronic Rhinosinusitis with Nasal Polyposis)
►▼
Show Figures
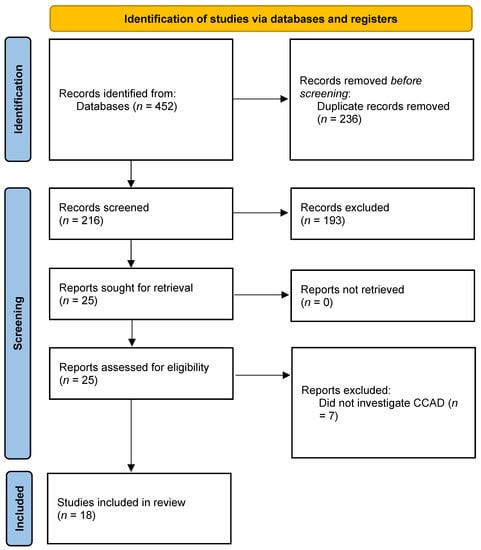
Figure 1
Open AccessCase Report
Bleach-Induced Chemical Sinusitis and Orbital Cellulitis Following Root Canal Treatment
by
Terese Huiying Low, Jun Jie Seah, Somasundaram Subramaniam, Vijayaraj Thirunavukarasu and Chew Lip Ng
Sinusitis 2023, 7(1), 6-11; https://doi.org/10.3390/sinusitis7010002 - 31 May 2023
Abstract
►▼
Show Figures
The authors describe an unusual case of chemical sinusitis and orbital cellulitis secondary to a sodium hypochlorite accident in a patient who had just undergone root canal treatment. The patient presented with acute, progressive symptoms of unilateral maxillary sinusitis, facial cellulitis and orbital
[...] Read more.
The authors describe an unusual case of chemical sinusitis and orbital cellulitis secondary to a sodium hypochlorite accident in a patient who had just undergone root canal treatment. The patient presented with acute, progressive symptoms of unilateral maxillary sinusitis, facial cellulitis and orbital cellulitis which began hours after root canal treatment on the ipsilateral side. He was admitted to hospital under the care of the Otorhinolaryngology team and reviewed regularly by the Ophthalmologists. He underwent Endoscopic Sinus Surgery during his hospital stay. The intraoperative findings revealed necrotic sinus mucosa and slough within the involved maxillary sinus, which were suggestive of chemical burn injury induced by the highly alkaline sodium hypochlorite solution used during root canal treatment. He was treated postoperatively with regular nasal toilet, culture-directed antibiotics and topical ocular pressure-lowering eyedrops. He displayed a slow recovery with eventually no orbital sequelae, but experienced persistent cheek numbness three months post-injury. Severe chemical sinusitis with orbital cellulitis secondary to sodium hypochlorite accident is a rare complication of root canal treatment, with potentially severe consequences. It can present with symptoms similar to complicated acute bacterial sinusitis. Otorhinolaryngologists and dental surgeons should maintain a high index of suspicion when managing a patient post-root canal treatment with symptoms of unilateral sinusitis, facial cellulitis, orbital cellulitis and even airway compromise. This would allow prompt intervention before sight or life-threatening complications set in.
Full article
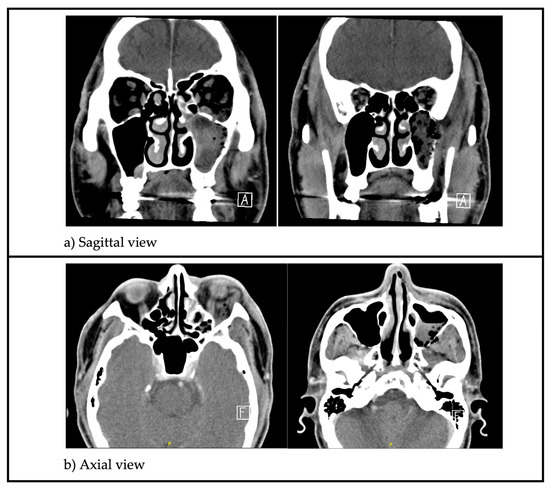
Figure 1
Open AccessBrief Report
Patient-Reported Outcomes with Benralizumab in Patients with Severe Eosinophilic Asthma and Severe Chronic Rhinosinusitis with Nasal Polyps
by
Rory Chan, Kirsten Stewart, Rasads Misirovs and Brian Lipworth
Sinusitis 2023, 7(1), 1-5; https://doi.org/10.3390/sinusitis7010001 - 29 Mar 2023
Abstract
►▼
Show Figures
Introduction: Chronic rhinosinusitis with nasal polyps (CRSwNP) and severe eosinophilic asthma (SEA) are common comorbidities characterised by type 2 inflammation associated with increased expression of interleukin 5. Methods: Eight patients with SEA and severe CRSwNP attended the Scottish Centre for Respiratory Research as
[...] Read more.
Introduction: Chronic rhinosinusitis with nasal polyps (CRSwNP) and severe eosinophilic asthma (SEA) are common comorbidities characterised by type 2 inflammation associated with increased expression of interleukin 5. Methods: Eight patients with SEA and severe CRSwNP attended the Scottish Centre for Respiratory Research as part of a clinical trial (EudraCT number 2019-003763-22). Following an initial 4-week run-in period (baseline) when patients took their usual inhaled and intranasal corticosteroid treatment for SEA and CRSwNP, they all received subcutaneous benralizumab 30 mg q4w for 12 weeks. Results: Following 12 weeks of benralizumab, no significant differences were detected in nasal global symptom visual analogue score (VAS), hyposmia VAS, total nasal symptom score, or peak nasal inspiratory flow. In contrast, Asthma Control Questionnaire significantly improved along with near-complete depletion of peripheral blood eosinophils by 99%, while eosinophil-derived neurotoxin fell by 72%. Conclusions: Greater improvements in patient-reported outcomes related to asthma were observed than with CRSwNP in response to benralizumab.
Full article

Figure 1
Open AccessArticle
Immunomodulators Containing Epicor, Colostrum, Vitamin D, Zinc, Lactobacilli and Bifidobacterium Reduce Respiratory Exacerbations in Children and Adults with Chronic Pulmonary Diseases
by
Snezhina Lazova, Nikolay Yanev, Nadia Kolarova-Yaneva and Tsvetelina Velikova
Sinusitis 2022, 6(2), 66-76; https://doi.org/10.3390/sinusitis6020009 - 02 Dec 2022
Abstract
(1) Background: A number of studies have demonstrated the connection between developing or exacerbating chronic respiratory diseases in adults and children. However, still, few studies focus on reducing exacerbations via immunomodulation. (2) Methods: In this pilot study, a total of 25 pediatric and
[...] Read more.
(1) Background: A number of studies have demonstrated the connection between developing or exacerbating chronic respiratory diseases in adults and children. However, still, few studies focus on reducing exacerbations via immunomodulation. (2) Methods: In this pilot study, a total of 25 pediatric and adult patients with bronchial asthma (BA) and chronic obstructive pulmonary disease (COPD)/persistent bacterial bronchitis (PBB) were included, administered over-the-counter (OTC) immunomodulators and followed up for 6 or 12 months. (3) Results: We observed a decrease in the frequency of exacerbations with slight improvements in functional respiratory indicators in adults on their second and third visits and a reduced number of exacerbations and improved spirometry indices in children with BA, although exacerbations requiring hospital admission remained at a similar rate. (4) Conclusions: We confirmed that the number of exacerbations of underlying chronic respiratory disease in adults and children could be reduced after the administration of OTC immunomodulators, probably by optimizing the immune resistance to common viral infections.
Full article
(This article belongs to the Special Issue Feature Papers in Sinusitis 2022)
►▼
Show Figures

Figure 1
Open AccessArticle
The Safety of Topical and Intravenous Tranexamic Acid in Endoscopic Sinus Surgery
by
Agrani Ratnayake Kumar and Andrew James Wood
Sinusitis 2022, 6(2), 56-65; https://doi.org/10.3390/sinusitis6020008 - 18 Oct 2022
Abstract
Tranexamic acid (TXA) is an inexpensive and widely used medication indicated for the reduction of bleeding. There are data showing the efficacy of intravenous (IV) and topical TXA in endoscopic sinus surgery (ESS) but the safety of this practice is not well studied.
[...] Read more.
Tranexamic acid (TXA) is an inexpensive and widely used medication indicated for the reduction of bleeding. There are data showing the efficacy of intravenous (IV) and topical TXA in endoscopic sinus surgery (ESS) but the safety of this practice is not well studied. The objective of this study was to assess the safety of using both IV and topical TXA in ESS. A scoping review was performed to investigate the effect of TXA on respiratory epithelia. A retrospective single-surgeon study was used to assess 177 comprehensive ESS cases from January 2017–December 2019 for the safety of combined IV and topical TXA. The scoping review demonstrated that respiratory epithelia could withstand a wide range of TXA concentrations without detrimental morphological effects. Topical TXA may have positive effects on wound healing and inflammation. The retrospective study showed no thromboembolic complications attributable to TXA in the 28 days after ESS. Only two patients (1.3%) who received TXA re-presented with post-operative bleeding. The use of IV and topical TXA is safe with regards to its effect on respiratory epithelium and thromboembolic disease. Topical TXA may have more positive effects than merely the reduction of bleeding following ESS.
Full article
(This article belongs to the Special Issue Innovations in the Management of Chronic Rhinosinusitis)
►▼
Show Figures
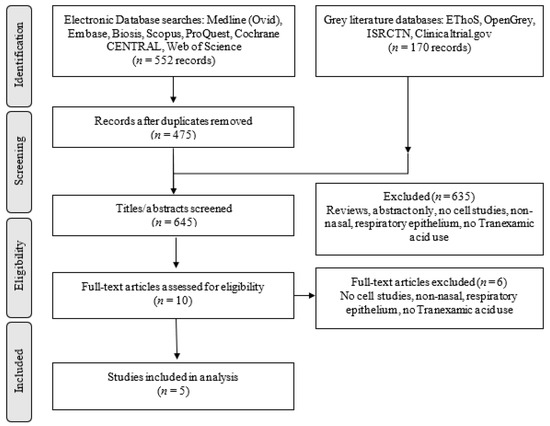
Figure 1
Open AccessReview
Home-Based Respiratory Care for COPD Patients
by
Ricardo G. Figueiredo, Caio Laudano, Jaqueline Muniz and José de Bessa, Jr.
Sinusitis 2022, 6(2), 49-55; https://doi.org/10.3390/sinusitis6020007 - 12 Sep 2022
Cited by 1
Abstract
Despite significant advances in pharmacological treatment over the last few decades, COPD remains a heavy burden on the health systems around the world, affecting approximately 210 million people, with elevated morbimortality and socioeconomic impact. Barriers to healthcare access were even more evident during
[...] Read more.
Despite significant advances in pharmacological treatment over the last few decades, COPD remains a heavy burden on the health systems around the world, affecting approximately 210 million people, with elevated morbimortality and socioeconomic impact. Barriers to healthcare access were even more evident during the coronavirus disease 19 (COVID-19) pandemic and increased patients’ vulnerability to physical deconditioning, depression, and social isolation. Home-based respiratory care in patients with COPD provides a valuable contribution to effective disease management, with potential advantages for monitoring, treatment adherence, and cost reduction. Technological innovation allows clinical markers of interest, such as respiratory frequency, pulmonary function, and oxygen saturation, to be tracked remotely from the patients’ homes, providing a better understanding of their real needs. Home-based telerehabilitation can also be a viable alternative to hospital-based programs. Here, we highlight the full extent of health benefits of HRC in COPD, particularly for patients with a higher risk of exacerbations, multiple comorbidities, and limited access to health services.
Full article
(This article belongs to the Special Issue The Asthma, Rhinitis and Chronic Pulmonary Diseases)
►▼
Show Figures
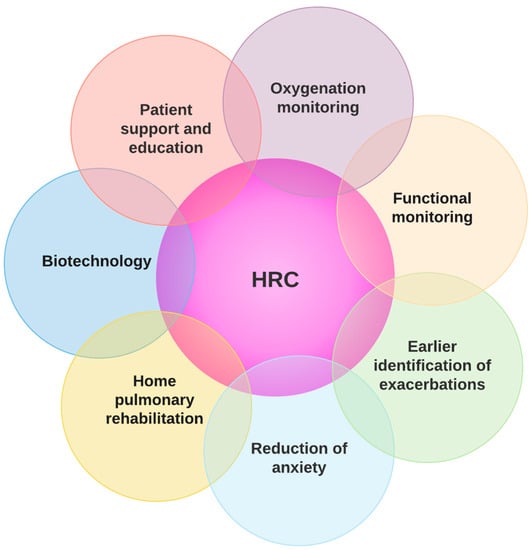
Figure 1
Open AccessArticle
Recurrent Acute Otitis Media Could Be Related to the Pro-Inflammatory State That Causes an Incorrect Diet
by
Fernando M. Calatayud-Sáez, Blanca Calatayud and Ana Calatayud
Sinusitis 2022, 6(2), 36-48; https://doi.org/10.3390/sinusitis6020006 - 22 Aug 2022
Cited by 3
Abstract
Introduction: Acute Otitis Media (AOM) is the most commonly-occurring bacterial complication in childhood. After making certain corrections to the patients’ dietary habits, which we found to be excessively high in animal-based and industrially-processed foods, we observed a significant reduction in recurrent colds and
[...] Read more.
Introduction: Acute Otitis Media (AOM) is the most commonly-occurring bacterial complication in childhood. After making certain corrections to the patients’ dietary habits, which we found to be excessively high in animal-based and industrially-processed foods, we observed a significant reduction in recurrent colds and their bacterial complications. We promote an original way of treating these diseases, since until now the conventional treatment is based on pharmacological and surgical treatment. From our point of view, the mucosa that covers the entire ENT area is in a pro-inflammatory and hyper-reactive state, as a consequence of the alterations produced by an inadequate diet. For us there is no difference in the nutritional treatment of the different mucous membranes that cover the ENT area. The purpose of the study was to assess the effects of the Traditional Mediterranean Diet (TMD) on patients diagnosed with Recurring Acute Otitis Media (RAOM). Methods: prospective pre-postest comparison study with 48 girls and 42 boys aged 1–5 years, each of whom had been and included on the 1-year programme “Learning to eat the Mediterranean Way”, designed to encourage the adoption of the TMD. We studied clinical and therapeutic variables and various anthropometric parameters. Results: all the symptomatic indicators studied (number and intensity of episodes of otitis and emergency admissions) showed a positive and statistically significant evolution in RAOM. By the end of the study, none of the patients met the criteria for classification as RAOM, and 60% percent of patients did not present any further episodes of AOM. In line with the above, the use of anti-microbial drugs and symptomatic treatments reduced considerably; the use of antibiotics dropped from 4.30 occasions/patient/year, to 0.66 (p < 0.001), and the used of symptomatic treatments dropped from 7.63 to 2.75 (p < 0.001). The level of family satisfaction was very high. Conclusions: the adoption of the Traditional Mediterranean Diet has been demonstrated to significantly reduce occurrence of acute otitis media and may contribute to the treatment of patients diagnosed with recurrent acute otitis media.
Full article
(This article belongs to the Special Issue Rhinosinusitis, Otitis, Tubaritis, Adenoiditis, and Other Inflammatory Diseases (-Itis), Mediated by Immunological Alterations Caused by Inadequate Nutrition)
►▼
Show Figures
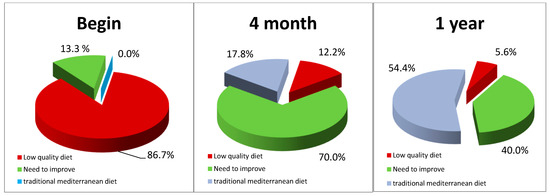
Figure 1
Open AccessReview
The Role of Dual Bronchodilation and the Conscientious Use of Inhaled Corticosteroid in COPD
by
Ricardo G. Figueiredo, Lucas F. Araujo and José de Bessa Junior
Sinusitis 2022, 6(2), 32-35; https://doi.org/10.3390/sinusitis6020005 - 05 Aug 2022
Abstract
Chronic obstructive pulmonary disease (COPD) is a global public health burden that stands out as a leading cause of mortality around the world, especially in less developed countries. COPD treatment should be centered on the individual necessities of each patient, integrating pharmacological therapy,
[...] Read more.
Chronic obstructive pulmonary disease (COPD) is a global public health burden that stands out as a leading cause of mortality around the world, especially in less developed countries. COPD treatment should be centered on the individual necessities of each patient, integrating pharmacological therapy, immunization, nutritional support, pulmonary rehabilitation and control of comorbidities. Combining a long-acting antimuscarinic (LAMA) with a long-acting beta2-agonist (LABA) bronchodilator has proven to be more effective than monotherapy with LABA or LAMA, in terms of the functional improvement of forced expiratory volume (FEV1), symptoms and life quality and may be helpful in patients with progressive dyspnea. The eosinophil blood count is a simple biomarker that could guide personalized treatment strategies by identifying patients with greater clinical benefits of inhaled corticosteroid (ICS) treatment. However, one critical concern is the increased risk of pneumonia in individuals treated with ICS.
Full article
(This article belongs to the Special Issue The Asthma, Rhinitis and Chronic Pulmonary Diseases)
►▼
Show Figures

Figure 1
Open AccessEditorial
Promotion and Restoration of Health with the Amazing Mediterranean Diet versus an Increase in Childhood Pathology Due to the Disastrous Diet of ‘Western Civilisation’
by
Fernando M. Calatayud-Sáez
Sinusitis 2022, 6(2), 26-31; https://doi.org/10.3390/sinusitis6020004 - 15 Jul 2022
Cited by 1
Abstract
‘Understand your honours that it is not so much that the traditional diet rooted in our homes has a miraculous character, as that the diet that modernity imposes on us is unhealthy and inadequate for the human intestines [...]
Full article
(This article belongs to the Special Issue Rhinosinusitis, Otitis, Tubaritis, Adenoiditis, and Other Inflammatory Diseases (-Itis), Mediated by Immunological Alterations Caused by Inadequate Nutrition)
Open AccessEditorial
Allergic Rhinosinusitis and Airway Diseases
by
Sy Duong-Quy
Sinusitis 2022, 6(1), 21-25; https://doi.org/10.3390/sinusitis6010003 - 14 May 2022
Abstract
The concept of united airway disease interaction, which comprises chronic rhinosinusitis and other lower airway disorders such as asthma, has been recognized for over a decade [...]
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
►▼
Show Figures
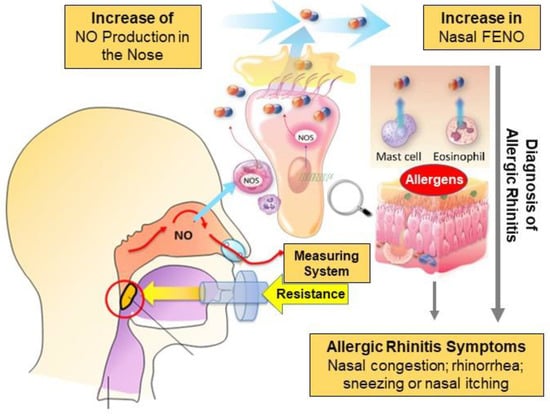
Figure 1
Open AccessReview
Promoting Equity When Using the SNOT-22 Score: A Scoping Review and Literature Review
by
Abigail Weaver and Andrew Wood
Sinusitis 2022, 6(1), 15-20; https://doi.org/10.3390/sinusitis6010002 - 16 Jan 2022
Cited by 1
Abstract
It is established that non-white people experience worse health outcomes than white people within the same population. Equity addresses differences between patient subgroups, allowing needs-based distribution of resources. The use of quality-of-life (QoL) tools to assist clinical decision making such as the SNOT-22
[...] Read more.
It is established that non-white people experience worse health outcomes than white people within the same population. Equity addresses differences between patient subgroups, allowing needs-based distribution of resources. The use of quality-of-life (QoL) tools to assist clinical decision making such as the SNOT-22 for chronic rhinosinusitis promotes equality, not equity, as quality-of-life (QoL) tools provide the same criteria of symptom scoring across diverse populations. We considered the effects of ethnicity and race on SNOT-22 scores and whether these scores should be adjusted to improve equity. PubMed and MEDLINE provided papers for a scoping review. A combination of the following search terms was used: patient-reported outcome measures (PROM) (OR) quality of life; (AND) race (OR) ethnicity (OR) disparities; (AND) otolaryngology (OR) SNOT-22 (OR) sinusitis. The first study identified no evidence of ethnic variability in SNOT-22 scores. However, the study did not represent the local population, including 86% white people. Other studies identified baseline SNOT-22 disparities with respect to population demographics, gender, and age. Ethnic differences appear to exist in acute sinusitis symptomatology. In other fields both within and outside of otorhinolaryngology, ethnic differences exist with regard to QoL tools. This scoping review identified a paucity of data in rhinology. However, evidence implies some form of correction to QoL scores could help promote equity for non-white patients.
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
Open AccessArticle
Atopic Status in Children with Asthma and Respiratory Allergies—Comparative Analysis of Total IgE, ImmunoCAP Phadiatop/fx5 and Euroimmun Pediatric Immunoblot
by
Snezhina Lazova, Marta Baleva, Stamatios Priftis, Emilia Naseva and Tsvetelina Velikova
Sinusitis 2022, 6(1), 1-14; https://doi.org/10.3390/sinusitis6010001 - 29 Dec 2021
Cited by 2
Abstract
Introduction: An atopic status assessment (skin prick test or specific immunoglobulin (sIgE)) in asthmatic children is considered a milestone in identifying potential risk factors and triggers provoking loss of asthma control and asthma exacerbation. Objective: The study aims to perform a comparative analysis
[...] Read more.
Introduction: An atopic status assessment (skin prick test or specific immunoglobulin (sIgE)) in asthmatic children is considered a milestone in identifying potential risk factors and triggers provoking loss of asthma control and asthma exacerbation. Objective: The study aims to perform a comparative analysis of different laboratory methods for a serological assessment of an atopic status in asthma and respiratory allergies in children. Material and methods: A total of 86 children were included, all of whom were diagnosed with bronchial asthma, aged from 5 to 17 years and screened for total IgE level using enzyme-linked immunosorbent assay (ELISA). In 48 randomly selected children, we performed a semi-quantitative serological in vitro assessment of the specific IgE antibodies against food and aeroallergen, using two different laboratory methods—Euroimmun Immunoblot and ImmunoCAP (Phadiatop/fx5). Results: In 70% of the children with a history of allergies, and 65.3% without clinically manifested allergies, multiscreen test ImmunoCAP Phadiatop/fx5 showed positivity and confirmed atopy. Our results showed a significant moderate to strong correlation between multiscreen ImmunoCAP Phadiatop/fx5, and Euroimmun specific IgE titers against aero-allergens—cats, mites, tree mix and food allergens—soy, wheat (р = 0.006), rice, р = 0.090), apple р = 0.007) and peanut. A sensitivity of 63% and specificity of 73.5% was observed for EUROIMMUN Pediatric (food allergens, IgE titer > 1) compared with the gold standard ImmunoCap/fx5. The mean value of total IgE is significantly higher in children with asthma and concomitant with allergic rhinitis compared to those without allergic rhinitis (mean 202.52 U/mL, IQR 102.50 (24.20–363.95) vs. 316.68, IQR 261.00 (109.20–552.50), p = 0.005). Conclusion: Establishing the spectrum of the most common respiratory and food allergens is an essential factor for maintaining asthma control, both through a strategy to avoid allergen exposure and by developing a recommendation plan. The immunoblotting technique is easily applicable in daily clinical and laboratory practice. It is also a cost-effective and reliable alternative to the “gold standard” ImmunoCAP Phadiatop/fx5 in diagnosing atopy in children.
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
►▼
Show Figures
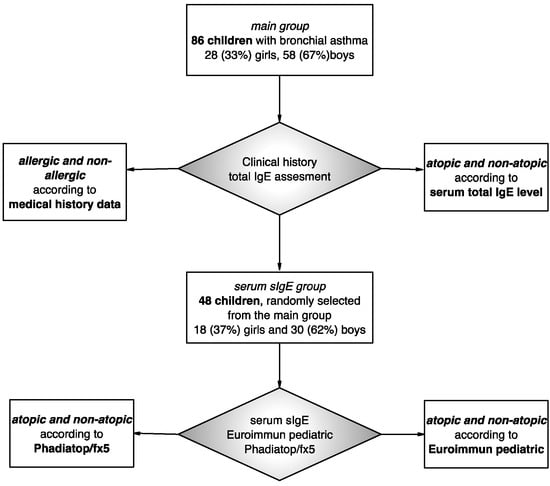
Figure 1
Open AccessCase Report
Clearance of Bone Substitute in Gel Form Accidentally Dispersed into the Sinus Cavity during Transcrestal Maxillary Sinus Floor Elevation: Two-Case Report
by
Fabio Bernardello, Teresa Lombardi and Claudio Stacchi
Sinusitis 2021, 5(2), 132-140; https://doi.org/10.3390/sinusitis5020014 - 27 Oct 2021
Cited by 1
Abstract
Sinus membrane perforation is the most frequent intraoperative complication occurring during maxillary sinus floor elevation. Although numerous techniques for perforation management are present, grafting material dissemination may still occur, representing a potential trigger factor leading to acute or chronic sinusitis. This case report
[...] Read more.
Sinus membrane perforation is the most frequent intraoperative complication occurring during maxillary sinus floor elevation. Although numerous techniques for perforation management are present, grafting material dissemination may still occur, representing a potential trigger factor leading to acute or chronic sinusitis. This case report describes two cases of xenogeneic bone substitute in gel form accidentally dispersed into the sinus cavity during maxillary sinus floor elevation with a transcrestal approach. In both cases, immediately postoperative radiographic imaging showed an important amount of gel graft dislodged into the sinus cavity as a consequence of hidden perforations that remained undetected during surgery. Patients were monitored for 6 months after surgery and reported no signs or symptoms related to possible sinus disease. Control radiographs showed no sinus membrane hypertrophy and/or presence of residual disseminated gel, confirming complete clearance of the accidentally dispersed graft through the ostiomeatal complex. In order to minimize postoperative complications, bone substitutes in gel form could represent an interesting alternative to granular grafts for their easier clearance from the maxillary sinus cavity in case of accidental dissemination during sinus augmentation procedures.
Full article
(This article belongs to the Special Issue Feature Papers in Sinusitis 2021)
►▼
Show Figures
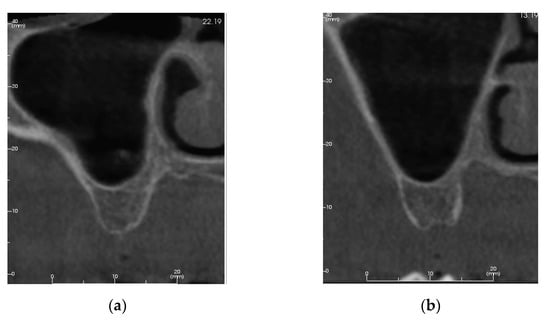
Figure 1
Open AccessArticle
Study of Nasal Fractional Exhaled Nitric Oxide (FENO) in Children with Allergic Rhinitis
by
Sy Duong-Quy, Thuy Nguyen-Thi-Dieu, Khai Tran-Quang, Tram Tang-Thi-Thao, Toi Nguyen-Van, Thu Vo-Pham-Minh, Quan Vu-Tran-Thien, Khue Bui-Diem, Vinh Nguyen-Nhu, Lam Hoang-Thi and Timothy Craig
Sinusitis 2021, 5(2), 123-131; https://doi.org/10.3390/sinusitis5020013 - 08 Oct 2021
Cited by 2
Abstract
(1) Background: Exhaled nitric oxide (NO) has been considered as a biomarker of airway inflammation. The measurement of fractional exhaled NO (FENO) is a valuable test for assessing local inflammation in subjects with allergic rhinitis (AR). (2) Objective: To evaluate (a) the correlation
[...] Read more.
(1) Background: Exhaled nitric oxide (NO) has been considered as a biomarker of airway inflammation. The measurement of fractional exhaled NO (FENO) is a valuable test for assessing local inflammation in subjects with allergic rhinitis (AR). (2) Objective: To evaluate (a) the correlation between nasal FENO with anthropometric characteristics, symptoms of AR and nasal peak flows in children without and with AR; and (b) the cut-off of nasal FENO for diagnosis of AR in symptomatic children. (3) Methods: The study was a descriptive and cross-sectional study in subjects with and without AR < 18 years old. All clinical and functional characteristics of the study subjects were recorded for analysis. They were divided into healthy subjects for the control group and subjects with AR who met all inclusion criteria. (4) Results: 100 subjects (14 ± 3 years) were included, including 32 control subjects and 68 patients with AR. Nasal FENO in AR patients was significantly higher than in control subjects: 985 ± 232 ppb vs. 229 ± 65 ppb (p < 0.001). In control subjects, nasal FENO was not correlated with anthropometric characteristics and nasal inspiratory or expiratory peak flows (IPF or EPF) (p > 0.05). There was a correlation between nasal FENO and AR symptoms in AR patients and nasal IPF and EPF (p = 0.001 and 0.0001, respectively). The cut-off of nasal FENO for positive AR diagnosis with the highest specificity and sensitivity was ≥794 ppb (96.7% and 92.6%, respectively). (5) Conclusion: The use of nasal FENO as a biomarker of AR provides a useful tool and additional armamentarium in the management of allergic rhinitis.
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
►▼
Show Figures
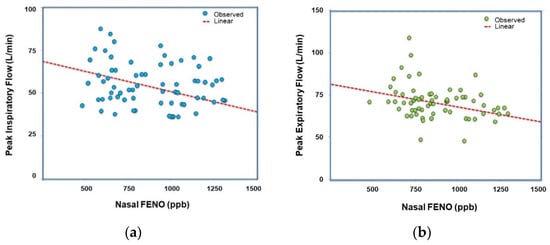
Figure 1
Open AccessReview
Olfactory Disorders in Post-Acute COVID-19 Syndrome
by
Laura Araújo, Vanessa Arata and Ricardo G. Figueiredo
Sinusitis 2021, 5(2), 116-122; https://doi.org/10.3390/sinusitis5020012 - 24 Sep 2021
Cited by 5
Abstract
Altered smell is one of the most prevalent symptoms in acute COVID-19 infection. Although most patients recover normal neurosensory function in a few weeks, approximately one-tenth of patients report long-term smell dysfunction, including anosmia, hyposmia, parosmia and phantosmia, with a particularly notable impact
[...] Read more.
Altered smell is one of the most prevalent symptoms in acute COVID-19 infection. Although most patients recover normal neurosensory function in a few weeks, approximately one-tenth of patients report long-term smell dysfunction, including anosmia, hyposmia, parosmia and phantosmia, with a particularly notable impact on quality of life. In this complex scenario, inflammation and cellular damage may play a key role in the pathogenesis of olfactory dysfunctions and may affect olfactory signaling from the peripheral to the central nervous system. Appropriate management of smell disturbances in COVID-19 patients must focus on the underlying mechanisms and the assessment of neurosensorial pathways. This article aims to review the aspects of olfactory impairment, including its pathophysiology, epidemiology, and clinical management in post-acute COVID-19 syndrome (PACS).
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
►▼
Show Figures
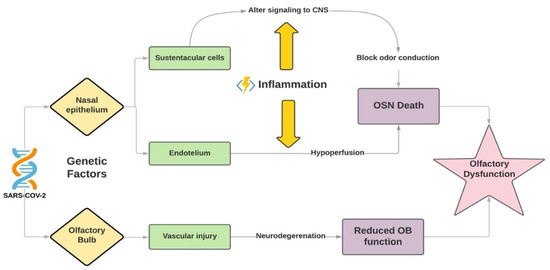
Figure 1
Open AccessArticle
Effects of the Traditional Mediterranean Diet in Childhood Recurrent Acute Rhinosinusitis
by
Fernando M. Calatayud-Sáez, Blanca Calatayud and Ana Calatayud
Sinusitis 2021, 5(2), 101-115; https://doi.org/10.3390/sinusitis5020011 - 02 Sep 2021
Cited by 5
Abstract
Introduction: There are more and more studies that demonstrate the anti-inflammatory effects of the traditional Mediterranean diet (TMD). The aim of the study was to assess the effects of an intervention with the TMD in patients with recurrent acute and chronic rhinosinusitis. Material
[...] Read more.
Introduction: There are more and more studies that demonstrate the anti-inflammatory effects of the traditional Mediterranean diet (TMD). The aim of the study was to assess the effects of an intervention with the TMD in patients with recurrent acute and chronic rhinosinusitis. Material and Methods: We performed a pretest–posttest comparison study in 114 patients (56 girls and 58 boys) aged one to five years who had three or more acute rhinosinusitis episodes in the period of 1 year. They were included for a year in the nutritional program “Learning to eat from the Mediterranean”. The anthropometric, clinical, and therapeutic characteristics were studied. Results: All the studied indicators showed a positive and statistically significant evolution. Of the patients, 53.5% did not have any episode of acute rhinosinusitis, and 26.3% had only one, compared to the 3.37 they had on average in the previous year. The use of antibiotics decreased by 87.6%. The degree of satisfaction of the families was very high. The Mediterranean Diet Quality Index (KIDMED) that assesses the quality of the TMD rose from 7.7 to 11 points. Conclusions: The adoption of the TMD could have promising effects in the prevention and treatment of recurrent acute and chronic rhinosinusitis, limiting the pharmacological and surgical intervention in many of these patients.
Full article
(This article belongs to the Special Issue Allergic Rhinosinusitis and Airway Diseases)
►▼
Show Figures
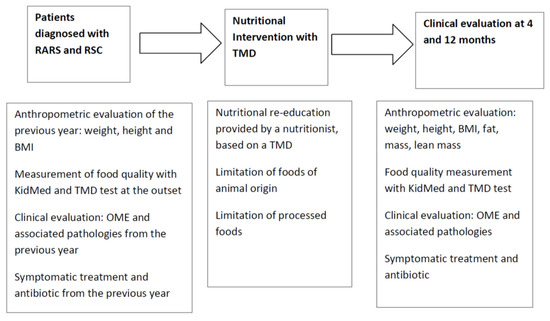
Figure 1
Open AccessArticle
Persistent Nasal Obstruction: An Expression of the Pro-Inflammatory State?
by
Fernando M. Calatayud-Sáez, Blanca Calatayud and Ana Calatayud
Sinusitis 2021, 5(1), 90-100; https://doi.org/10.3390/sinusitis5010010 - 15 Jun 2021
Cited by 5
Abstract
Introduction: During the first years of life, the oro-pharyngeal lymphoid tissue gradually increases in size, causing in some children difficulty breathing and often leading to surgical removal of the tonsils and adenoids. The objective of the study is to assess the effects of
[...] Read more.
Introduction: During the first years of life, the oro-pharyngeal lymphoid tissue gradually increases in size, causing in some children difficulty breathing and often leading to surgical removal of the tonsils and adenoids. The objective of the study is to assess the effects of the Mediterranean diet in children who had chronic upper airway obstruction. Material and methods: This was a prospective study pre-test/post-test comparison. Eighty-seven patients from two to eight years old were recruited. A food reeducation program based on the Mediterranean diet was applied for one year. Clinical, therapeutic, and anthropometric variables were studied. Results: The degree of nasal obstruction decreased in 95.1% of the patients. After the nutritional intervention, the number of colds with bacterial complications decreased by 80.26%; 60.9% had no bacterial complications during the year of the study. The use of antibiotics decreased by 81.94%. Symptomatic treatment decreased by 61.2%. Most patients did not require surgical intervention, and clinical evolution suggested that it would no longer be necessary. Conclusions: We can conclude by saying that the application of the traditional Mediterranean diet could be effective in the prevention and treatment of persistent nasal obstruction, limiting pharmacological and surgical intervention in many of these patients.
Full article
(This article belongs to the Special Issue Feature Papers in Sinusitis 2021)
►▼
Show Figures

Figure 1
Open AccessReview
A Review on the Medicinal and Pharmacological Properties of Traditional Ethnomedicinal Plant Sonapatha, Oroxylum indicum
by
Ganesh Chandra Jagetia
Sinusitis 2021, 5(1), 71-89; https://doi.org/10.3390/sinusitis5010009 - 25 May 2021
Cited by 12
Abstract
Oroxylum indicum, Sonapatha is traditionally used to treat asthma, biliousness, bronchitis, diarrhea, dysentery, fevers, vomiting, inflammation, leukoderma, skin diseases, rheumatoid arthritis, wound injury, and deworm intestine. This review has been written by collecting the relevant information from published material on various ethnomedicinal and
[...] Read more.
Oroxylum indicum, Sonapatha is traditionally used to treat asthma, biliousness, bronchitis, diarrhea, dysentery, fevers, vomiting, inflammation, leukoderma, skin diseases, rheumatoid arthritis, wound injury, and deworm intestine. This review has been written by collecting the relevant information from published material on various ethnomedicinal and pharmacological aspects of Sonapatha by making an internet, PubMed, SciFinder, Science direct, and Google Scholar search. Various experimental studies have shown that Sonapatha scavenges different free radicals and possesses alkaloids, flavonoids, cardio glycosides, tannins, sterols, phenols, saponins, and other phytochemicals. Numerous active principles including oroxylin A, chrysin, scutellarin, baicalein, and many more have been isolated from the different parts of Sonapatha. Sonapatha acts against microbial infection, cancer, hepatic, gastrointestinal, cardiac, and diabetic disorders. It is useful in the treatment of obesity and wound healing in in vitro and in vivo preclinical models. Sonapatha elevates glutathione, glutathione-s-transferase, glutathione peroxidase, catalase, and superoxide dismutase levels and reduces aspartate transaminase alanine aminotransaminase, alkaline phosphatase, lactate dehydrogenase, and lipid peroxidation levels in various tissues. Sonapatha activates the expression of p53, pRb, Fas, FasL, IL-12, and caspases and inhibited nuclear factor kappa (NF-κB), cyclooxygenase (COX-2), tumor necrosis factor (TNFα), interleukin (IL6), P38 activated mitogen-activated protein kinases (MAPK), fatty acid synthetase (FAS), sterol regulatory element-binding proteins 1c (SREBP-1c), proliferator-activated receptor γ2 (PPARγ2), glucose transporter (GLUT4), leptin, and HPV18 oncoproteins E6 and E7 at the molecular level, which may be responsible for its medicinal properties. The phytoconstituents of Sonapatha including oroxylin A, chrysin, and baicalein inhibit the replication of SARS-CoV-2 (COVID-19) in in vitro and in vivo experimental models, indicating its potential to contain COVID-19 infection in humans. The experimental studies in various preclinical models validate the use of Sonapatha in ethnomedicine and Ayurveda.
Full article
(This article belongs to the Special Issue Feature Papers in Sinusitis 2021)
►▼
Show Figures

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics




