Recent Advances in Preeclampsia
Share This Topical Collection
Editor
 Prof. Dr. Berthold Huppertz
Prof. Dr. Berthold Huppertz
 Prof. Dr. Berthold Huppertz
Prof. Dr. Berthold Huppertz
E-Mail
Website
Collection Editor
Division of Cell Biology, Histology and Embryology, Gottfried Schatz Research Center, Medical University of Graz, Graz, Austria
Interests: cell biology; morphology; apoptosis; human placenta; trophoblast; invasion; preeclampsia; IUGR
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
Despite massive research efforts in recent decades, preeclampsia has remained a syndrome of hypotheses. Today, the etiology of the pathways resulting in the clinical symptoms of hypertension and proteinuria still remains obscure. Over time, a number of very promising hypotheses have been developed, but so far, not a single hypothesis has been accepted. The current hypotheses range from shallow trophoblast invasion, which is believed to result in placental hypoxia, to defects of the villous trophoblast resulting in the release of necrotic particles affecting the maternal endothelium, to a maternal failure to adapt to the stress test pregnancy. This Special Collection will summarize all hypotheses and will leave it to the readers to identify the most conclusive explanation.
To further promote submissions of high-quality manuscripts, we are now launching this Special Collection, where we will fully waive the publication fee. We hope you will submit your next manuscript.
Prof. Dr. Berthold Huppertz
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Reproductive Medicine is an international peer-reviewed open access quarterly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 1000 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Published Papers (3 papers)
Open AccessCommentary
17-α Hydroxyprogesterone Caproate Immunology, a Special Focus on Preterm Labor, Preeclampsia, and COVID-19
by
Rasha A. Al-Lami
Viewed by 1777
Abstract
17-α hydroxyprogesterone caproate (17-OHPC) could alter the immune response and inflammation, specifically affecting the risk of preterm labor and preeclampsia. However, the exact immune and inflammatory effects of 17-OHPC remain hard to be identified. The current literature on 17-OHPC immune effects is limited
[...] Read more.
17-α hydroxyprogesterone caproate (17-OHPC) could alter the immune response and inflammation, specifically affecting the risk of preterm labor and preeclampsia. However, the exact immune and inflammatory effects of 17-OHPC remain hard to be identified. The current literature on 17-OHPC immune effects is limited and more research is needed to identify these mechanistic pathways. Further, coronavirus disease 2019 (COVID-19) infection in pregnancy involves heightened immune response, widespread inflammation and high rates of preterm labor and preeclampsia. Since the pathogenesis of preterm labor, preeclampsia and COVID-19 involves inflammation and altered immune response, it is important to explore the possible immune effects of 17-OHPC in pregnant women with COVID-19. This commentary article will explain the immune effects of 17-OHPC and their implications in preterm labor, preeclampsia and COVID-19.
Full article
Open AccessArticle
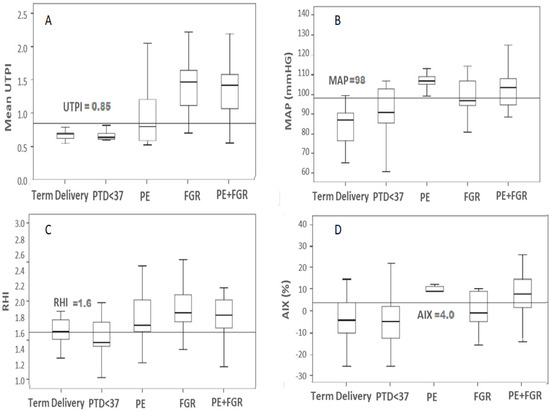
Biophysical Markers of Suspected Preeclampsia, Fetal Growth Restriction and The Two Combined—How Accurate They Are?
by
Adi Sharabi-Nov, Nataša Tul, Kristina Kumer, Tanja Premru Sršen, Vesna Fabjan Vodušek, Teja Fabjan, Josko Osredkar, Kypros H. Nicolaides and Hamutal Meiri
Cited by 1 | Viewed by 2583
Abstract
Objectives—To conduct a secondary analysis of prediction accuracy of biophysical markers for suspected Preeclampsia (PE), Fetal Growth Restriction (FGR) and the two combined near delivery in a Slovenian cohort. Methods—This was a secondary analysis of a database of a total 125 Slovenian pregnant
[...] Read more.
Objectives—To conduct a secondary analysis of prediction accuracy of biophysical markers for suspected Preeclampsia (PE), Fetal Growth Restriction (FGR) and the two combined near delivery in a Slovenian cohort. Methods—This was a secondary analysis of a database of a total 125 Slovenian pregnant women attending a high-risk pregnancy clinic due to suspected PE (
n = 31), FGR (
n = 16) and PE + FGR (
n = 42) from 28–39 weeks gestation and their corresponding term (
n = 21) and preterm (PTD,
n = 15) controls. Data for Mean Arterial blood Pressure (MAP) and Uterine artery pulsatility index (UtA PI) estimated by Doppler sonography were extracted from the database of patients who were tested at admission to the high-risk clinic with the suspected complications. The reactive hyperemia index (RHI), and the Augmentation Index (AIX%) were extracted from the patient database using measured values obtained with the assistance of the Endo PAT, a device set to measure the signal of the peripheral arterial tone (PAT) from the blood vessels endothelium. Linear regression coefficients, Box and Whisker plots, Area under the Curve (AUC) of receiver Operation Characteristic (ROC) curves, and multiple regression were used to assess the marker accuracy using detection rate (DR) and false-positive rate (FPR) and previously reported cut-offs for estimating the positive and negative predictive value (NPV and PPV). The SPSS non-parametric statistics (Kruskal Wallis and Mann–Whitney) and Spearman’s regression coefficient were used to assess marker accuracy;
p < 0.05 was considered significant. Results—MAP values reached diagnostic accuracy (AUC = 1.00, DR = 100%) for early PE cases delivered < 34, whereas UtA Doppler PI values yielded such results for early FGR < 34 weeks and the two combined reached such accuracy for PE + FGR. To reach diagnostic accuracy for all cases of the complications, the Endo PAT markers with values for MAP and UtA Doppler PI were required for cases near delivery. Multiple regression analyses showed added value for advanced maternal age and gestational week in risk assessment for all cases of PE, FGR, and PE + FGR. Spearman’s regression coefficient yielded r > 0.6 for UtA Doppler PI over GA for PE and FGR, whereas for RHI over BMI, the regression coefficient was r > 0.5 (
p < 0.001 for each). Very high correlations were also found between UtA Doppler PI and sFlt-1/PlGF or PlGF (r = −0.495,
p < 0.001), especially in cases of FGR. Conclusion—The classical biophysical markers MAP and UtA Doppler PI provided diagnostic accuracy for PE and FGR < 34 wks gestation. A multiple biophysical marker analysis was required to reach diagnostic accuracy for all cases of these complications. The UtA Doppler PI and maternal serum sFlt-1/PlGF or PlGF were equally accurate for early cases to enable the choice of the markers for the clinical use according to the more accessible method.
Full article
►▼
Show Figures
Open AccessArticle
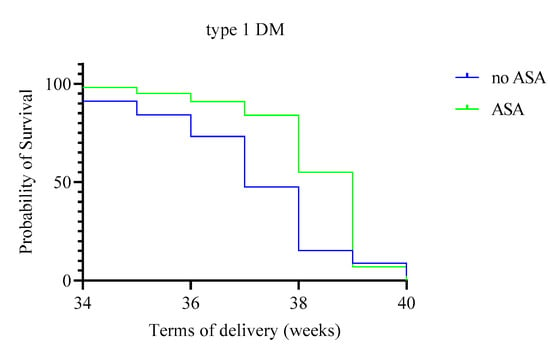
Efficacy of Low Doses of Acetylsalicylic Acid in the Prevention of Preeclampsia in Women with Type 1 and 2 Diabetes Mellitus
by
Roman V. Kapustin, Elizaveta M. Tcybuk, Andrew V. Korenevsky, Ekaterina V. Kopteeva, Elena N. Alekseenkova, Alena V. Tiselko and Olga N. Arzhanova
Cited by 1 | Viewed by 2771
Abstract
Background: The effective approach to preventing preeclampsia (PE) is administering acetylsalicylic acid (ASA) to high-risk patients. However, there are not enough data analyzing the effectiveness of ASA intake by pregnant women with diabetes mellitus (DM). This study aims to evaluate the effect of
[...] Read more.
Background: The effective approach to preventing preeclampsia (PE) is administering acetylsalicylic acid (ASA) to high-risk patients. However, there are not enough data analyzing the effectiveness of ASA intake by pregnant women with diabetes mellitus (DM). This study aims to evaluate the effect of ASA on perinatal outcomes in pregnant women with different types of pregestational DM. Methods: This retrospective study included 735 pregnant women with DM (types 1 and 2). At 12–14 weeks of gestation, some patients were prescribed daily ASA at a 100–150 mg dose continuously for up to 36 weeks. The effect of ASA on the development of PE and other outcomes of pregnancy was assessed. The times of delivery and the onset of PE were evaluated as well. Results: When taking ASA, PE developed significantly less frequently in pregnant women with DM. This was significantly more evident in patients with type 2 DM (OR 0.65; 95% CI: 0.52–0.79). In patients with type 1 DM, the mean period of development of PE was 1.5 weeks later relative to those pregnant women who did not take the drug and was 35.5 weeks of gestation. The OR for the development of preterm birth was reduced by 3 times (OR 0.33; 95% CI: 0.15–0.62). In women with DM who took ASA during pregnancy, babies were born with greater body weight, and the frequency of small for gestational age births decreased. Conclusions: ASA administration is associated with a reduction of the incidence of PE, a delay in its manifestations, and a mitigating the risk of other adverse perinatal outcomes typical for pregnant women with DM.
Full article
►▼
Show Figures