Interdisciplinary Medicine – The Key For Personalized Medicine
A topical collection in Medicina (ISSN 1648-9144).
Viewed by 55264Editor
Interests: heart failure; arterial hypertension; comorbidities; interdisciplinary issues; ultrasonography; arterial diseases; dyslipidemia management; diabetes
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
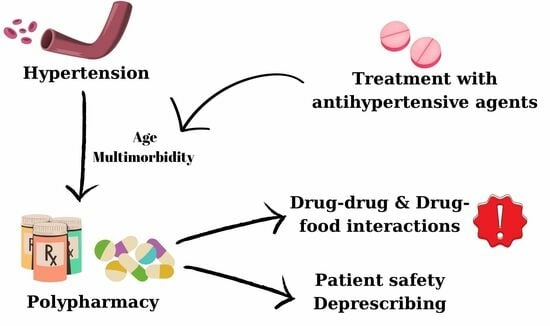
Personalized medicine is the approach that can tailor diagnosis and treatment to ensure the best patient care in uncertain times. The challenging field of medicine and healthcare is rapidly adopting scientific and technological innovations, making interdisciplinary collaborations especially important. In this context, medical disciplines are becoming increasingly interlinked with other specialities and fields. A more interdisciplinary approach to the patient is needed, especially for complex patients with numerous comorbidities, most of them usually elderly and fragile. The greatest challenges to human health lie at the intersection of different medical fields. An interdisciplinary medical team is more and more necessary, with the rapid expansion of medical knowledge.
Given the importance of interdisciplinarity in the field of medicine and research, the journal Medicina is launching this Special Issue.
We encourage you and your colleagues to submit your articles reporting on this topic. Reviews or original articles dealing with interdisciplinary medical issues, as well as articles providing an up-to-date overview of the diagnostic protocols and individualized treatments for patients with multiple comorbidities, are particularly welcome. In addition, we warmly invite you to submit articles reporting on rare diseases.
Dr. Camelia Diaconu
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Medicina is an international peer-reviewed open access monthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 1800 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Interdisciplinarity
- Comorbidities
- Chronic heart failure
- Atrial fibrillation
- Diabetes mellitus
- Cardiovascular risk assessment
- Cancer
- Surgical treatment