Journal Description
Journal of Vascular Diseases
Journal of Vascular Diseases
is an international, peer-reviewed, open access journal on all aspects of cardiovascular, cerebrovascular, and peripheral vascular diseases, published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 25 days after submission; acceptance to publication is undertaken in 41.3 days (median values for papers published in this journal in the second half of 2023).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- JVD is a companion journal of Journal of Clinical Medicine.
subject
Imprint Information
Open Access
ISSN: 2813-2475
Latest Articles
The Comorbidity and Associations between Depression, Cognitive Impairment, and Sleep after Stroke and How They Affect Outcomes: A Scoping Review of the Literature
J. Vasc. Dis. 2024, 3(2), 134-151; https://doi.org/10.3390/jvd3020012 - 01 Apr 2024
Abstract
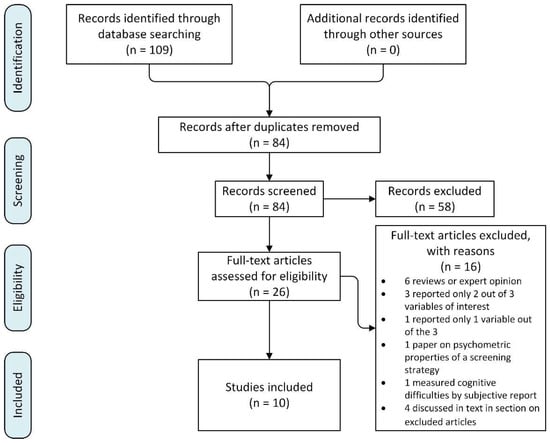
Objectives: post-stroke depression (PSD), cognitive impairment, and sleep disturbances are the most common post-stroke conditions. To aid clinical practice for a highly confounded clinical problem, a clearer understanding of the associations between comorbid PSD, post-stroke cognitive impairment, and sleep disturbances is necessary. Materials
[...] Read more.
Objectives: post-stroke depression (PSD), cognitive impairment, and sleep disturbances are the most common post-stroke conditions. To aid clinical practice for a highly confounded clinical problem, a clearer understanding of the associations between comorbid PSD, post-stroke cognitive impairment, and sleep disturbances is necessary. Materials and Methods: a scoping review of the literature was conducted according to the recommended guidelines using the search term [“stroke (mesh term) AND depression (in the abstract) AND cognitive (in the abstract) AND sleep (in the abstract)”]. Results: 10 studies met the criteria for inclusion. Only one study reported a co-occurrence of post-stroke emotional distress and sleep disturbances at a rate of 10.7%. Poor sleep and cognitive impairment are independent risk factors for PSD. The relationship between post-stroke poor sleep and cognitive impairment is ambiguous. None of the studies examined how PSD, cognitive impairment, and sleep disturbances interact to influence stroke outcomes. Conclusions: the dearth of studies indicates either a lack of awareness of the potential relationship between the three outcomes and the possible range of inter-related non-motor outcomes after stroke or the practical challenges in designing appropriate studies. The included studies had methodological weaknesses in their observational design and use of imprecise, subjective outcome measurements. Important knowledge gaps are identified for future research.
Full article
(This article belongs to the Special Issue Neurologic Injury and Neurodegeneration)
►
Show Figures
Open AccessArticle
Early Results of the Sandwich Technique Using Cyanoacrylate Glue and Polidocanol Foam Sclerotherapy for the Treatment of Varicose Veins
by
Marian Simka and Marcin Skuła
J. Vasc. Dis. 2024, 3(2), 127-133; https://doi.org/10.3390/jvd3020011 - 01 Apr 2024
Abstract
Background: This is a retrospective analysis of the results of treatment for varicose veins using the sandwich technique with cyanoacrylate glue and foam sclerotherapy. This novel method allows for a substantial reduction in the amount of glue needed for vein closure, and
[...] Read more.
Background: This is a retrospective analysis of the results of treatment for varicose veins using the sandwich technique with cyanoacrylate glue and foam sclerotherapy. This novel method allows for a substantial reduction in the amount of glue needed for vein closure, and minimizes the risk of granuloma formation and allergic reaction related to the epifascial administration of cyanoacrylate. Methods: This technique was used in 60 patients, 77 intrafascial veins were managed. Vein closures were performed with Venex cyanoacrylate glue and 1–3% polidocanol foam. All procedures were performed under ultrasonographic control, through direct percutaneous punctures of target veins. Follow-ups were scheduled 1–3 weeks after the procedure. If revealed, unclosed segments of the target veins were obliterated at these follow-up visits, with glue and/or sclerotherapy. Results: There were no serious adverse events intra- or postprocedurally. The technical success rate was 100%. The primary success rate at 1–3 weeks follow-up was 84.4%. The primary assisted success rate, after additional closures, was 100%. Conclusions: We demonstrated that the treatment for varicose veins, using a sandwich technique, which combines cyanoacrylate glue and foam sclerotherapy, can be safe and efficient.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
Open AccessArticle
Bilateral Carotid Calcification Correlates with Regional Cerebral Glucose Metabolism: Insights from PET/CT Imaging of Patients with Cardiovascular Risk Factors
by
Eric M. Teichner, Robert C. Subtirelu, Shiv Patil, Omar Al-Daoud, Chitra Parikh, Linh Nguyen, Jordan Atary, Andrew Newberg, Poul Flemming Høilund-Carlsen and Abass Alavi
J. Vasc. Dis. 2024, 3(2), 112-126; https://doi.org/10.3390/jvd3020010 - 01 Apr 2024
Abstract
Background: Cardiovascular disease is a leading cause of illness and death globally, primarily due to atherosclerosis. This disease reduces blood flow and oxygen delivery to organs, and when it affects the carotid arteries, it can lead to cognitive impairment and dementia. In a
[...] Read more.
Background: Cardiovascular disease is a leading cause of illness and death globally, primarily due to atherosclerosis. This disease reduces blood flow and oxygen delivery to organs, and when it affects the carotid arteries, it can lead to cognitive impairment and dementia. In a population of 104 individuals, comprising both healthy controls and individuals at elevated risk for developing cardiovascular diseases (CVD) due to identified risk factors, we used PET imaging with 18F-fluorodeoxyglucose (FDG) to assess cerebral glucose metabolism and 18F-sodium fluoride (NaF) to detect atherosclerotic calcification. Our statistical analysis revealed significant differences in metabolic activity between healthy and at-risk individuals in specific brain regions. 18F-FDG uptake in the brain varied inversely with respect to the clinical assessment of cardiovascular risk in regions such as the cuneus (β = −0.030, SE = 0.014, p = 0.035), middle occipital gyrus (β = −0.032, SE = 0.011, p = 0.005), and posterior cingulate gyrus (β = −0.032, SE = 0.015, p = 0.044). In contrast, areas including the basis pontis (β = 0.025, SE = 0.012, p = 0.038) and the pons (β = 0.034, SE = 0.013, p = 0.008) exhibited direct correlations. Notably, carotid 18F-NaF uptake had inverse associations with 18F-FDG uptake in the cerebellum (β = −0.825, SE = 0.354, p = 0.021), medulla (β = −0.888, SE = 0.405, p = 0.029), and posterior cingulate gyrus (β = −1.253, SE = 0.567, p = 0.028), while increased carotid calcification influenced metabolic activity in the fusiform gyrus (β = 1.660, SE = 0.498, p = 0.001) and globus pallidus (β = 1.505, SE = 0.571, p = 0.009). We observed that atherosclerotic plaque accumulation, especially in the carotid arteries, has potential implications for metabolic changes in brain regions governing cognition, emotion, sensory perception, and motor activities. Our findings underscore the possible early interventions that can be used to preempt or delay cognitive deterioration linked with cardiovascular ailments.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Guanylyl Cyclase Activator Improves Endothelial Function by Decreasing Superoxide Anion Concentration
by
Ariane M. Martinelli, Luis Henrique O. de Moraes, Thiago F. de Moraes and Gerson J. Rodrigues
J. Vasc. Dis. 2024, 3(1), 102-111; https://doi.org/10.3390/jvd3010009 - 04 Mar 2024
Abstract
Introduction: Soluble guanylyl cyclase (sGC) activation in vascular smooth muscle has the potential to induce vasodilation. Chronic sGC activation enhanced vascular function in the congestive heart failure animal model. Therefore, sGC activation can lead to vasodilation and improvement in endothelial function. Objective: To
[...] Read more.
Introduction: Soluble guanylyl cyclase (sGC) activation in vascular smooth muscle has the potential to induce vasodilation. Chronic sGC activation enhanced vascular function in the congestive heart failure animal model. Therefore, sGC activation can lead to vasodilation and improvement in endothelial function. Objective: To investigate whether the selective sGC activator can revert the endothelial dysfunction and investigate the mechanism of action. Methods: Wistar rats were split into two groups: normotensive (2K) and hypertensive rats (2K-1C). Intact aortic rings were placed in a myograph and incubated with 0.1 µM ataciguat for 30 min. Cumulative concentration-effect curves were generated for acetylcholine (Ach) to assess endothelial function. The pD2 and maximum relaxant effect (Emax) were measured to Ach. In endothelial cell culture, superoxide anion (O2•−) was detected by using fluorescent probes, including DHE and lucigenin. Results: Ataciguat improved the relaxation induced by acetylcholine in 2K-1C (pD2: 6.99 ± 0.08, n = 6) compared to the control (pD2: 6.43 ± 0.07, n = 6, p < 0.05). The aortic rings were also improved from 2K (pD2: 7.04 ± 0.13, n = 6) compared to the control (pD2: 6.59 ± 0.07, n = 6, p < 0.05). Moreover, Emax was improved by ataciguat treatment in the 2K-1C aorta (Emax: 81.0 ± 1.0; n = 6), and 2K aorta (Emax: 92.98 ± 1.83; n = 6), compared to the control (Emax 2K-1C: 52.14 ± 2.16, n = 6; and Emax 2K: 76.07 ± 4.35, n = 6, p < 0.05). In endothelial cell culture, treatment with ataciguat (0.1, 1, and 10 µM) resulted in a reduction of the superoxide anion formation induced by angiotensin II. Conclusions: Our findings indicated that ataciguat effectively enhanced endothelial function through the inactivation of superoxide anions.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
►▼
Show Figures
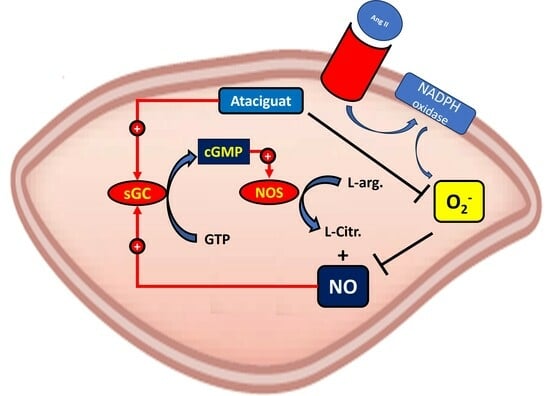
Graphical abstract
Open AccessReview
Aortic Elasticity and Cardiovascular Risk Stratification: A Narrative Review on the Current Understanding
by
Niya Mileva, Tsvetelina Velikova, Toni Velikov and Dobrin Vassilev
J. Vasc. Dis. 2024, 3(1), 88-101; https://doi.org/10.3390/jvd3010008 - 01 Mar 2024
Abstract
Cardiovascular risk stratification is a cornerstone of preventive cardiology, aiming to identify individuals at a higher risk for adverse events. In line with this, aortic elastic properties have gained recognition as crucial indicators of vascular health and predictors of cardiovascular outcomes. This narrative
[...] Read more.
Cardiovascular risk stratification is a cornerstone of preventive cardiology, aiming to identify individuals at a higher risk for adverse events. In line with this, aortic elastic properties have gained recognition as crucial indicators of vascular health and predictors of cardiovascular outcomes. This narrative review delves into the significance of aortic stiffness, compliance, and distensibility in risk assessment, shedding light on their associations with cardiovascular diseases, such as hypertension, atherosclerosis, and coronary artery disease. This review aims to provide an overview of the current knowledge regarding aortic elastic properties and their role in cardiovascular risk stratification. The exploration of potential mechanisms and clinical implications outlines the need for further research to establish precise links between aortic elasticity and cardiovascular risk. Furthermore, the integration of advanced imaging, genetic factors, and personalized medicine is suggested to refine risk assessment strategies and enhance patient care. Ultimately, this review underscores the importance of aortic elastic properties in cardiovascular risk prediction, opening avenues for future research and clinical application.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures
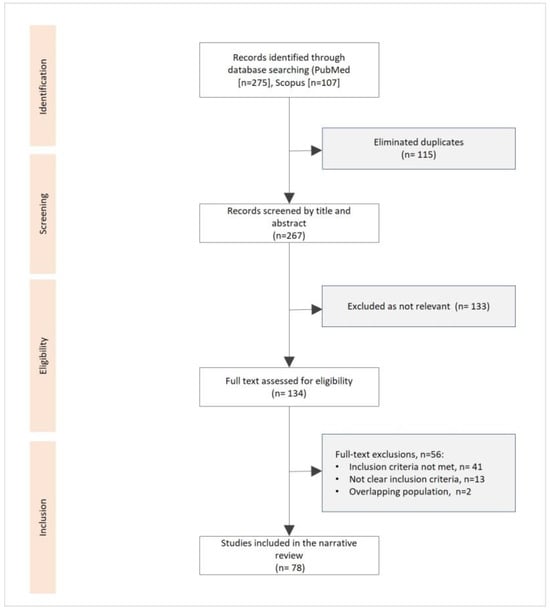
Figure 1
Open AccessOpinion
Enhancing the Management of Pediatric Sickle Cell Disease by Integrating Functional Evaluation to Mitigate the Burden of Vaso-Occlusive Crises
by
Paul Muteb Boma, Alain Ali Kaponda, Jules Panda and Bruno Bonnechère
J. Vasc. Dis. 2024, 3(1), 77-87; https://doi.org/10.3390/jvd3010007 - 01 Mar 2024
Abstract
Sickle cell disease (SCD) imposes a significant health burden, particularly in low- and middle-income countries where healthcare professionals and resources are scarce. This opinion paper delves into the management strategies employed for vaso-occlusive crises (VOCs) in pediatric patients with SCD, advocating for the
[...] Read more.
Sickle cell disease (SCD) imposes a significant health burden, particularly in low- and middle-income countries where healthcare professionals and resources are scarce. This opinion paper delves into the management strategies employed for vaso-occlusive crises (VOCs) in pediatric patients with SCD, advocating for the adoption of a transformative strategy. We explore the integration of functional assessment approaches into existing procedures, highlighting the potential of technology-assisted rehabilitation, including wearable sensors and digital biomarkers, to enhance the effectiveness of managing and preventing VOCs. Rehabilomics, as a comprehensive framework, merges rehabilitation-related data with biomarkers, providing a basis for personalized therapeutic interventions. Despite the promising advantages of these approaches, persistent obstacles such as the limited availability of rehabilitation programs, especially in resource-limited settings, pose challenges. This paper underscores the importance of a collaborative strategy to effectively address the unique obstacles faced by patients with SCD. This collaborative approach involves improving accessibility to rehabilitation services, incorporating technology-supported therapy, and fostering focused research endeavors. The primary objective of this comprehensive approach is to enhance the overall care of SCD patients, with a specific focus on preventing VOCs, as well as providing tailored (neuro)rehabilitation services in resource-limited settings. By examining the current state of SCD management and proposing transformative strategies, this opinion paper seeks to inspire collective action and collaboration to improve outcomes for pediatric SCD patients globally.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Small Paracentral Acute Middle Maculopathy Lesions as Biomarker of Vascular Morbidity: Natural Course
by
Dmitrii S. Maltsev, Alexei N. Kulikov, Maria A. Burnasheva, Yana A. Kalinicheva and Alexander S. Vasiliev
J. Vasc. Dis. 2024, 3(1), 67-76; https://doi.org/10.3390/jvd3010006 - 01 Feb 2024
Abstract
Background: To evaluate the incidence rate of small paracentral acute middle maculopathy (PAMM) lesions in healthy fellow eyes of patients with retinal vein occlusions (RVO). Methods: Patients with unilateral branch RVO or central RVO who were followed up for at least one year
[...] Read more.
Background: To evaluate the incidence rate of small paracentral acute middle maculopathy (PAMM) lesions in healthy fellow eyes of patients with retinal vein occlusions (RVO). Methods: Patients with unilateral branch RVO or central RVO who were followed up for at least one year were included. Fellow healthy eyes were examined with 6 mm optical coherence tomography angiography scans at baseline and at the end of the follow-up. Small resolved PAMM lesions were displayed using structural en face projections of the slab between two segmentation lines of the outer plexiform layer with 0 µm and −9 µm offset. New lesions were identified by overlaying baseline and final structural en face projections. Results: A total of 41 eyes of 41 patients (12 females and 29 males, mean age 63.5 ± 10.1 years) were included. The mean follow-up was 23.6 ± 11.4 months. Among all RVO patients, small resolved PAMM lesions in healthy fellow eyes were found in 39 patients (95.1%). In the whole cohort, the median number of PAMM lesions was 5.5 (95% CI 3.0 to 8.0) (mean 6.5 ± 5.7) at baseline, which increased statistically significantly to 5.5 (95% CI 3.8 to 8.2) (mean 6.7 ± 5.7) at the end of the follow-up period (p = 0.03). Eight (19.5%) patients demonstrated new lesions, with a median number of new lesions of 1 (ranged 1 to 2). Conclusions: Small PAMM lesions seem to be a slowly progressing retinal vascular biomarker.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
►▼
Show Figures
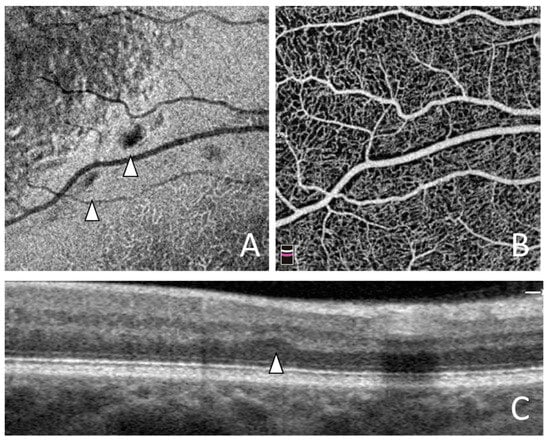
Figure 1
Open AccessBrief Report
Perceived Parental Style Is Better in Adults with Congenital Heart Disease than Healthy Controls—But There Is Work Left to Do in Specific Subgroups
by
Leon Brudy, Julia Hock, Laura Willinger, Renate Oberhoffer-Fritz, Alfred Hager, Peter Ewert and Jan Müller
J. Vasc. Dis. 2024, 3(1), 58-66; https://doi.org/10.3390/jvd3010005 - 01 Feb 2024
Abstract
Objective: To compare perceived parental style in a large cohort of adults with congenital heart disease (ACHD) to healthy reference (RCs). Furthermore, factors associated with perceived parental style were determined in ACHD. Patients and Methods: From September 2016 to April 2019, 912 ACHD
[...] Read more.
Objective: To compare perceived parental style in a large cohort of adults with congenital heart disease (ACHD) to healthy reference (RCs). Furthermore, factors associated with perceived parental style were determined in ACHD. Patients and Methods: From September 2016 to April 2019, 912 ACHD (34.9 ± 10.4 years, 45% female) and 175 RCs (35.8 ± 12.2 years, 53% female) completed the Measure of Parental Style (MOPS) questionnaire. Results: After adjusting for age and sex, ACHD recalled the parental style of both their parents to be significantly less indifferent (mother: ACHD: 1.2 ± 0.01 vs. RC: 1.3 ± 0.03, p < 0.001; father: ACHD: 1.3 ± 0.02 vs. RC: 1.7 ± 0.05, p < 0.001), overcontrolling (mother: ACHD: 1.6 ± 0.63 vs. RC: 1.9 ± 0.62, p < 0.001; father: ACHD: 1.4 ± 0.52 vs. RC: 1.5 ± 0.50, p < 0.001), and abusive (mother: ACHD: 1.2 ± 0.47 vs. RC: 1.4 ± 0.46, p < 0.001; father: ACHD: 1.3 ± 0.59 vs. RC: 1.5 ± 0.57, p < 0.001) than healthy controls did. In ACHD, female sex (β = 0.068, p = 0.017), higher age (β = 0.005, p = 0.003), Ebstein anomaly (β = 0.170, p = 0.005), and cyanotic CHD (β = 0.336, p = 0.004) contribute to perceiving the parental style of at least one of the parents negatively. Conclusions: While ACHD appear to recall the parental style to be less negative, subgroup analysis revealed specific patients at risk. These findings point to the need for interventions in specific subgroups susceptible to psychological distress.
Full article
(This article belongs to the Topic Diagnosis, Management, and Prognostic Assessment of Chronic Disease)
Open AccessArticle
Efficacy of High-Dose Diosmin Therapy in Chronic Venous Disease Treated with Endovenous Ablation: A Quality-of-Life Analysis
by
Antonia Rinaldi, Rita Zeno, Antonio Peluso, Luca del Guercio, Maurizio Sodo, Davide Turchino, Ruggero Iandoli, Davide Costa, Raffaele Serra and Umberto Marcello Bracale
J. Vasc. Dis. 2024, 3(1), 49-57; https://doi.org/10.3390/jvd3010004 - 01 Feb 2024
Abstract
Background. Vasoactive drugs are considered an important therapeutic tool in managing phlebolymphologic disease. The current study was performed to evaluate the results of a high-dose diosmin-based combination (Venoplant 2g) in symptomatic patients with chronic venous disease (CVD), treated with endovascular venous surgery, regarding
[...] Read more.
Background. Vasoactive drugs are considered an important therapeutic tool in managing phlebolymphologic disease. The current study was performed to evaluate the results of a high-dose diosmin-based combination (Venoplant 2g) in symptomatic patients with chronic venous disease (CVD), treated with endovascular venous surgery, regarding the efficacy of this treatment and the clinical signs and patients’ compliance. Methods: We identified, between April 2022 and March 2023, 50 patients with symptomatic CVD who underwent endovenous ablation and additionally were administered high-dose micronized diosmin. Parameters analyzed in the pre- and post-operative period were the venous clinical severity score (VCSS), the calf circumference, and a VEINES-QOL/Sym questionnaire. Treatment efficacy was assessed in post-operative follow-ups at 1 month and 2 months. Results: Quality-of-life analysis showed a significant improvement between t1 and t2 in both tests administered (VEINES-QOL/Sym: 55.2 ± 2.9, 39.2 ± 12.3, p: 0.001) (VCSS: 6.6 ± 1, 5.1 ± 0.7, p: 0.001). At the secondary endpoint, the results maintained the same improvement trend. Calf circumference was significantly reduced between t1 and t3 (41.7 ± 5.1, 38.3 ± 3.4, p: 0.001). Conclusion: High-dose diosmin, combined with sweet clover 320 mg, Centella asiatica 40 mg, and Vitamin C 200 mg, in patients treated with endovenous ablation, can be significantly effective in terms of clinical results in treating superficial venous disease. A patient’s calf circumference was also found to have decreased considerably during follow-up. No adverse effects have been recorded to date.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
Open AccessReview
When Vessels and Sarcomas Combine: A Review of the Inferior Vena Cava Leiomyosarcoma
by
João Martins Gama, Rui Almeida, Rui Caetano Oliveira and José Casanova
J. Vasc. Dis. 2024, 3(1), 34-48; https://doi.org/10.3390/jvd3010003 - 08 Jan 2024
Abstract
Leiomyosarcomas (LMSs) are malignant neoplasms of soft muscle differentiation that can be classified into five distinct groups according to site-related origin: intra-abdominal, subcutaneous or deep soft tissue of the limbs, cutaneous, external genitalia, and vascular. This distinction reflects different biological behaviors as well
[...] Read more.
Leiomyosarcomas (LMSs) are malignant neoplasms of soft muscle differentiation that can be classified into five distinct groups according to site-related origin: intra-abdominal, subcutaneous or deep soft tissue of the limbs, cutaneous, external genitalia, and vascular. This distinction reflects different biological behaviors as well as molecular changes, thus reflecting different prognoses and therapeutic options. Vascular LMSs are the least frequent, arising from the walls of the blood vessels, most commonly from the inferior vena cava. Due to its deep location, symptoms are non-specific, and the disease presents at an advanced stage, sometimes with metastases. Surgery is the treatment of choice, associated with chemo- and radiotherapy. Due to its rarity, most departments have minimal experience handling this disease. This article reviews the current knowledge on vascular leiomyosarcomas, particularly the inferior vena cava leiomyosarcoma.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Evaluation of the Molecular Mechanism of Chlorogenic Acid in the Treatment of Pulmonary Arterial Hypertension Based on Analysis Network Pharmacology and Molecular Docking
by
Jovito Cesar Santos-Álvarez, Juan Manuel Velázquez-Enríquez and Rafael Baltiérrez-Hoyos
J. Vasc. Dis. 2024, 3(1), 11-33; https://doi.org/10.3390/jvd3010002 - 05 Jan 2024
Abstract
Background: Pulmonary arterial hypertension (PAH) is a serious disease characterized by increased pressure in the pulmonary arteries, which can lead to heart failure and death. Chlorogenic acid (CGA) is a natural compound present in several foods and medicinal plants and has been described
[...] Read more.
Background: Pulmonary arterial hypertension (PAH) is a serious disease characterized by increased pressure in the pulmonary arteries, which can lead to heart failure and death. Chlorogenic acid (CGA) is a natural compound present in several foods and medicinal plants and has been described to exert a therapeutic effect in various diseases. However, its potential therapeutic effect on PAH remains undeciphered. In this study, the potential of CGA for the treatment of PAH was investigated using network pharmacology analysis and molecular docking. Methods: Potential CGA targets were obtained from the SwissTargetPrediction and GeneCards databases. Moreover, potential PAH targets were collected from the GeneCards and DisGNET databases. Then, common targets were selected, and a protein-protein network (PPI) was constructed between common CGA and PAH targets using the STRING database. The common hub targets were selected, and GO enrichment analysis was performed via KEGG using the DAVID 6.8 database. Additionally, molecular docking analysis was performed to investigate the interaction between CGA and these potential therapeutic targets. Results: We obtained 168 potential targets for CGA and 5779 potential targets associated with PAH. Among them, 133 were common to both CGA and PAH. The main hub targets identified through PPI network analysis were TP53, HIF1A, CASP3, IL1B, JUN, MMP9, CCL2, VEGFA, SRC, IKBKB, MMP2, CASP8, NOS3, MMP1, and CASP1. KEGG pathway analysis showed that these hub targets are associated with pathways such as lipid and atherosclerosis, fluid shear stress and atherosclerosis, and the IL-17 signaling pathway. In addition, the molecular docking results showed a high binding affinity between CGA and the 15 hub PAH-associated targets, further supporting its therapeutic potential. Conclusions: This study provides preliminary evidence on the underlying molecular mechanism of CGA in the treatment of PAH. The findings suggest that CGA could be a promising option for the development of new PAH drugs.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures
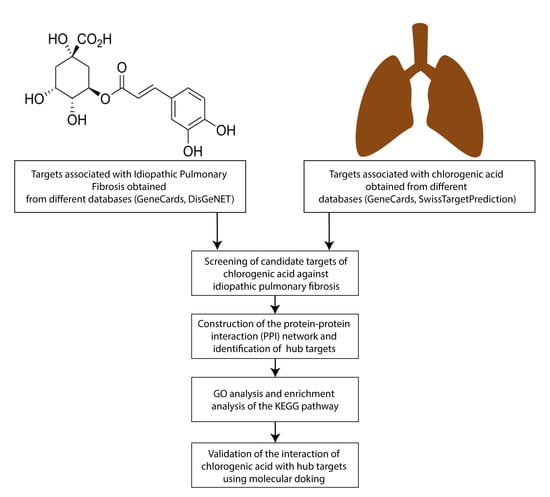
Graphical abstract
Open AccessArticle
Factors Associated with the Evolution of Superficial Vein Thrombosis and Its Impact on the Quality of Life: Results from a Prospective, Unicentric Study
by
Blanca Ros Gómez, Javier Gómez-López, Manuel Quintana-Díaz, Sheila Victoria Calvo Sevilla, Pablo Rodríguez-Fuertes, Fabian Tejeda-Jurado, Paula Berrocal-Espinosa, Juan Francisco Martínez-Ballester, Sonia Rodríguez-Roca, María Angélica Rivera Núñez, Ana M. Martínez Virto, Alberto Martín-Vega, Carmen Fernández-Capitán, Giorgina Salgueiro-Origlia, Raquel Marín-Baselga, Alicia Lorenzo Hernández, Teresa Sancho Bueso, Ramón Puchades Rincón de Arellano, Belén Gutiérrez-Sancerni, Alejandro Díez-Vidal, Sergio Carrasco-Molina and Yale Tung-Chenadd
Show full author list
remove
Hide full author list
J. Vasc. Dis. 2024, 3(1), 1-10; https://doi.org/10.3390/jvd3010001 - 02 Jan 2024
Abstract
Background: Superficial venous thrombosis (SVT) is a common clinical condition caused by inflammation and the presence of a thrombus inside a superficial vein. It has traditionally been considered a benign and banal disorder, although it can progress or can be associated with thromboembolic
[...] Read more.
Background: Superficial venous thrombosis (SVT) is a common clinical condition caused by inflammation and the presence of a thrombus inside a superficial vein. It has traditionally been considered a benign and banal disorder, although it can progress or can be associated with thromboembolic disease of deep territories in up to 20%, asymptomatic or symptomatic pulmonary embolism (PE), especially if it affects the main trunk of the internal saphenous vein. The impact of deep vein thrombosis on the quality of life and its sequelae have long been described in the literature; however, they have not been studied in superficial vein thrombosis. Objectives: We aimed to evaluate the risk factors, management, and complications of SVT and its impact on the quality of life of our patients. Methods: Observational, prospective, single-center study to evaluate the management of SVT. The ultrasound (US) was performed initially on symptomatic patients, during treatment with low-molecular-weight heparin (LMWH), at a follow-up, and at the end of 45 days of treatment. A quality-of-life questionnaire was administered to determine the risk factors, management, and complications of SVT at the moment of diagnosis and at the end of treatment. We included patients referred from the emergency department to a monographic consultation for thromboembolic disease, over 18 years of age with a diagnosis of acute SVT symptomatic, without contraindication to initiate anticoagulation. Results: In total, 63 patients were evaluated between October 2020 and April 2022. The mean age was 65.8 years (SD 13.5), of which 35 were women (55.6%), 39 presented cardiovascular risk factors (61.9%), 25 had a history of previous personal venous thromboembolism (VTE) (39.7%), and 10 had obesity (15.9%), 47 had chronic venous insufficiency or varicose veins (74.9%). During follow-up with ultrasound, 39.7% had partial revascularization, and at discharge, 63.5% had permeabilized the thrombosis against 19% who had residual thrombosis or progression of thrombosis. There was a positive correlation between mobility parameters and improvement in the performance of daily activities (rho = 0.35; p = 0.012) and with improvement in pain/discomfort (rho = 0.37; p = 0.007). An improvement in pain parameters was statistically significantly related to a global assessment health perception (rho = 0.48; p < 0.001). Anxiety and depression parameters were related to a global assessment health perception (rho = 0.462; p = 0.001) and to an overall improvement at 12 months (rho = 0.45; p = 0.001). CONCLUSIONS: Superficial venous thrombosis (SVT) is a highly prevalent disease, which is traditionally considered banal and has good evolution, with heterogeneous management in clinical practice and limited information on patient selection for therapies, current treatment routes, and drug use, as well as outcomes. In recent years, the importance of this entity has become evident due to its frequency in clinical practice, its risk of complications, and the impact it has on the quality of life. This study’s results emphasize the importance of the diagnosis, treatment, and follow-up of superficial venous thrombosis.
Full article
(This article belongs to the Section Peripheral Vascular Diseases)
Open AccessArticle
Abnormal Heart Sound Classification and Model Interpretability: A Transfer Learning Approach with Deep Learning
by
Milan Marocchi, Leigh Abbott, Yue Rong, Sven Nordholm and Girish Dwivedi
J. Vasc. Dis. 2023, 2(4), 438-459; https://doi.org/10.3390/jvd2040034 - 04 Dec 2023
Abstract
Physician detection of heart sound abnormality is complicated by the inherent difficulty of detecting critical abnormalities in the presence of noise. Computer-aided heart auscultation provides a promising alternative for more accurate detection, with recent deep learning approaches exceeding expert accuracy. Although combining phonocardiogram
[...] Read more.
Physician detection of heart sound abnormality is complicated by the inherent difficulty of detecting critical abnormalities in the presence of noise. Computer-aided heart auscultation provides a promising alternative for more accurate detection, with recent deep learning approaches exceeding expert accuracy. Although combining phonocardiogram (PCG) data with electrocardiogram (ECG) data provides more information to an abnormal heart sound classifier, the scarce presence of labelled datasets with this combination impedes training. This paper explores fine-tuning deep convolutional neural networks such as ResNet, VGG, and inceptionv3, on images of spectrograms, mel-spectrograms, and scalograms. By fine-tuning deep pre-trained models on image representations of ECG and PCG, we achieve 91.25% accuracy on the training-a dataset of the PhysioNet Computing in Cardiology Challenge 2016, compared to a previous result of 81.48%. Interpretation of the model’s learned features is also provided, with the results indicative of clinical significance.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures

Figure 1
Open AccessReview
Unravelling the Threads: A Brief Insight into Vascular Dementia
by
Syed Haris Omar
J. Vasc. Dis. 2023, 2(4), 419-437; https://doi.org/10.3390/jvd2040033 - 02 Nov 2023
Abstract
Vascular dementia (VaD), characterized by cognitive decline attributable to cerebrovascular disease, is the second most common type of dementia after Alzheimer’s disease. This review aims to explore the prevalent risk factors, pharmacological interventions, and non-pharmacotherapeutic strategies associated with the condition. Recognized risk factors
[...] Read more.
Vascular dementia (VaD), characterized by cognitive decline attributable to cerebrovascular disease, is the second most common type of dementia after Alzheimer’s disease. This review aims to explore the prevalent risk factors, pharmacological interventions, and non-pharmacotherapeutic strategies associated with the condition. Recognized risk factors include advanced age, hypertension, diabetes mellitus, obesity, and hyperlipidemia with emerging evidence implicating additional lifestyle and genetic factors. Pharmacotherapy for VaD mainly focuses on managing these underlying risk factors, coupled with symptomatic treatments. Therapeutic agents commonly used include antihypertensives, statins, antiplatelet drugs, antidiabetic agents, and specific cognitive enhancers like cholinesterase inhibitors. However, the effectiveness of these treatments remains under continuous study, underscoring the need for comprehensive, individualized treatment plans. Non-pharmacotherapeutic strategies, encompassing lifestyle modifications such as diet and exercise have gained considerable attention. They have shown promise in improving cognitive function and enhancing the quality of life in patients with VaD. The application of a multi-domain intervention approach may provide a more holistic management strategy for VaD. Further research is needed to define the best practices in both pharmacotherapy and non-pharmacotherapy treatments, considering the multifactorial and heterogeneous nature of this condition.
Full article
(This article belongs to the Section Neurovascular Diseases)
►▼
Show Figures

Figure 1
Open AccessOpinion
New Paradigms for Thoracic Outlet Compression and Thoracic Outlet Syndrome, with or without Complications or Sequelae: A Trans-Continental and Trans-Disciplinary Opinion Paper
by
Pierre Abraham, Paul W. Wennberg, Pascal Bauer, Yongquan Gu, Nafi Ouedraogo, Lianrui Guo, Garry Tew, Lucia Mazzolai, Romeo Martini and Samir Henni
J. Vasc. Dis. 2023, 2(4), 413-418; https://doi.org/10.3390/jvd2040032 - 02 Nov 2023
Cited by 1
Abstract
The anatomy of the human shoulder predisposes the neurovascular bundle to compression at different levels of the thoracic outlet during abduction of the arm. There are four possible levels of compression at the thoracic outlet pathway: at the costo-clavicular angle, the inter-scalenic angle,
[...] Read more.
The anatomy of the human shoulder predisposes the neurovascular bundle to compression at different levels of the thoracic outlet during abduction of the arm. There are four possible levels of compression at the thoracic outlet pathway: at the costo-clavicular angle, the inter-scalenic angle, under the pectoralis minor muscle or at the level of the humeral head. The positional thoracic outlet compression (TOC) often remains completely asymptomatic. When symptomatic, compressions are collectively referred to as thoracic outlet syndrome (TOS) and may require surgery if physical therapy fails to improve symptoms. The “thoracic outlet compression with complications or sequelae” (the acronym of which is “TOC-CS”, which can be simplified as “TOX”) will almost invariably lead to surgery to release the compression, and other possible treatment targeting the complications as required. There is a continuum between TOC, TOS and TOX, which are simply different clinical stages of the same mechanical issue, just like the Rutherford grades represent different stages of lower extremity arterial disease. We believe that discriminating between TOC, TOS and TOX clarifies clinical definitions and their respective treatment options. TOC is to be considered as a physiological positional phenomenon, TOS requires medical or surgical treatment and surgery should be considered as a primary option in TOX.
Full article
(This article belongs to the Topic Diagnosis, Management, and Prognostic Assessment of Chronic Disease)
►▼
Show Figures

Figure 1
Open AccessCase Report
Covered Stent Herniation into Coronary Aneurysm Sac—A Case-Inspired Review of Neurointerventional Realignment Techniques
by
Jacek Klaudel, Piotr Radowski, Wojciech Trenkner, Michał Glaza, Krzysztof Pawłowski, Dariusz Surman, Włodzimierz Krasowski and Marek Szołkiewicz
J. Vasc. Dis. 2023, 2(4), 402-412; https://doi.org/10.3390/jvd2040031 - 01 Nov 2023
Abstract
Background: Coronary aneurysms are an infrequent finding in diagnostic angiography, with a reported incidence of 0.35–0.7% in the largest contemporary registries. At least half of them have an atherosclerotic etiology and as such they are often diagnosed in the setting of acute coronary
[...] Read more.
Background: Coronary aneurysms are an infrequent finding in diagnostic angiography, with a reported incidence of 0.35–0.7% in the largest contemporary registries. At least half of them have an atherosclerotic etiology and as such they are often diagnosed in the setting of acute coronary syndrome. The wiring of a thrombosed aneurysm is a difficult task and after successful recanalization, the operator has to decide on the optimal method of aneurysm exclusion. Covered stents are commonly deployed, but their use involves the risk of delivery failure as well as device dislodgement and loss due to their stiffness and size. Moreover, proper stent sizing and apposition is difficult in the case of thrombosed aneurysms. Case presentation: We present a case of coronary aneurysm recanalization and exclusion with a covered stent, with a postdilation-induced stent foreshortening. Due to the subsequent stent migration into the aneurysm sac, its repositioning was attempted. The pitfalls of coronary aneurysm stenting and neurointerventional techniques of prolapsed device realignment are discussed. Conclusions: An adequate landing zone is of the utmost importance in aneurysm exclusion with covered stents. In the case of a short stent anchoring in the normal vessel, another covered or conventional stent should be deployed to mitigate the risk of the device migration.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures
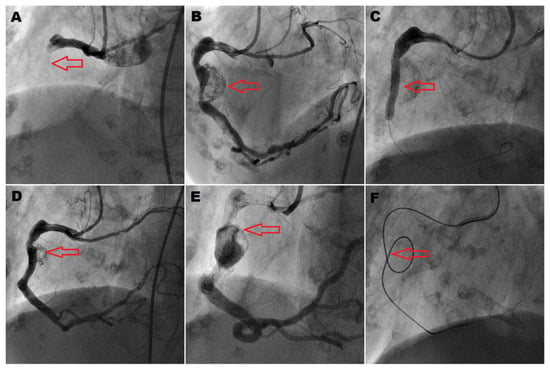
Figure 1
Open AccessCase Report
Arterial and Venous Pressure Monitoring during Cardiopulmonary Resuscitation for Out-of-Hospital Arrests: Four Case Reports
by
Hirokazu Onishi, Tasuku Matsuyama, Yuki Yasutake, Daichi Inaba, Tatsuji Katsue, Masaki Nagama, Yuto Iwasaki and Hitoshi Kano
J. Vasc. Dis. 2023, 2(4), 393-401; https://doi.org/10.3390/jvd2040030 - 07 Oct 2023
Abstract
Background: A new physiological monitoring system that simultaneously measures femoral arterial pressure, femoral venous pressure, and cerebral tissue oxygen saturation during CPR was used to evaluate the quality of cardiopulmonary resuscitation. In this case report, we would like to present four representative cases
[...] Read more.
Background: A new physiological monitoring system that simultaneously measures femoral arterial pressure, femoral venous pressure, and cerebral tissue oxygen saturation during CPR was used to evaluate the quality of cardiopulmonary resuscitation. In this case report, we would like to present four representative cases with this physiological monitoring system during CPR. Cases: We invasively measured femoral arterial pressure and femoral venous pressure if catheters were immediately inserted into the femoral artery and femoral vein for potential candidates who required extracorporeal cardiopulmonary resuscitation but did not receive such interventions. We presented several cases, including two cases in which cardiopulmonary resuscitation resulted in higher femoral arterial pressure compared to femoral venous pressure, an upward trend in cerebral tissue oxygen saturation values was observed, and both instances achieved the return of spontaneous circulation. In contrast, we also presented two patients with significant increases in femoral venous pressure and low cerebral tissue oxygen saturation values. In both cases, the return of spontaneous circulation was not achieved. Conclusions: We presented cases in which the femoral venous pressure exceeded the femoral arterial pressure using a simultaneous physiological monitoring system to monitor arterial pressure, venous pressure, and cerebral tissue oxygen saturation during cardiopulmonary resuscitation. Further case accumulations will be necessary to assess the variations in hemodynamic status during cardiopulmonary resuscitation and the association between each hemodynamic status and outcomes after cardiac arrest.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Urgent Off-Label Use of Flow–Diverter Stents in the Endovascular Management of Tonsillar Loop-Associated Internal Carotid Artery Dissections Presenting with Carotid Occlusion or Near-Occlusion and Major Ischemic Stroke
by
José E. Cohen, Andrei Filioglo, John Moshe Gomori, Asaf Honig, Ronen R. Leker and Hans Henkes
J. Vasc. Dis. 2023, 2(4), 381-392; https://doi.org/10.3390/jvd2040029 - 03 Oct 2023
Abstract
We present our experience with the implantation of flow diverter stents (FDSs) for the management of internal carotid artery (ICA) dissections in tortuous tonsillar loop segments. A total of 16 patients (10 women, 62.5%; mean age 39 ± 8 years; median baseline NIHSS
[...] Read more.
We present our experience with the implantation of flow diverter stents (FDSs) for the management of internal carotid artery (ICA) dissections in tortuous tonsillar loop segments. A total of 16 patients (10 women, 62.5%; mean age 39 ± 8 years; median baseline NIHSS 13; median ASPECTS 8.5) with acute ischemic stroke due to ICA dissection in a tortuous tonsillar loop segment, with/without large intracranial vessel thrombotic occlusion diagnosed between June 2015–February 2022 were included in this retrospective study under a waiver of informed consent. An FDS device was deployed from the petrous ICA toward the upper cervical ICA, completely covering the tonsillar loop. Stentriever-assisted thrombectomy was performed when indicated. A dual antiplatelet regimen was used during and after the procedure. Thrombocyte inhibition levels were evaluated before, during, and after the intervention. The ICA occlusion/near occlusion was successfully recanalized in all 16 patients with mean postangioplasty residual stenosis of 34 ± 14% (range 0–50%). Stent-assisted thrombectomy was performed in 15/16 patients (93.7%), achieving revascularization (TICI 2b–3) in all. There were no procedural complications and no intraprocedural embolic events; one asymptomatic petechial hemorrhage was detected. At 3-month follow-up, mRS 0–2 was seen in all patients. This report provides pilot data for a subsequent study on the use of flow diverter stents for ischemic cerebrovascular conditions. Our encouraging preliminary results await confirmation from further experience and prospective randomized studies.
Full article
(This article belongs to the Section Neurovascular Diseases)
Open AccessArticle
Computed Tomography Imaging Features of Pulmonary Sequestration
by
Tingqian Yang, Zhaoyu Wang, Jun Qiang, Qinxiang Mao, Shufeng Kong, Zhonghua Sun and Yu Li
J. Vasc. Dis. 2023, 2(4), 367-380; https://doi.org/10.3390/jvd2040028 - 01 Oct 2023
Abstract
Background: Pulmonary sequestration (PS), generally diagnosed using computed tomography pulmonary angiography (CTPA), is a rare congenital developmental malformation of the lung that is characterized by nonfunctional lung tissue, independent of the normal lung tissue. This paper summarizes the imaging features of the supplying
[...] Read more.
Background: Pulmonary sequestration (PS), generally diagnosed using computed tomography pulmonary angiography (CTPA), is a rare congenital developmental malformation of the lung that is characterized by nonfunctional lung tissue, independent of the normal lung tissue. This paper summarizes the imaging features of the supplying arteries and draining vessels in patients with PS with an aim to assist in timely clinical diagnosis and operation guidance. Materials and Methods: A total of 55 patients with PS diagnosed using CTPA from multiple clinical centers were retrospectively analyzed. Data included demographic characteristics, imaging features, disease location, isolation type, and the features of supplying and draining vessels, as shown on CTPA images. Results: Of the 55 patients reviewed, 3 (5.45%) were children, 3 (5.45%) were adolescents, and 49 (89.09%) were adults; the mean age was 44 years. Fifty-four (98.18%) patients had intralobar sequestration and one (1.82%) had extralobar sequestration. PS was noted 3.5 times more frequently in the left lower lobe than in the right lower lobe. For the supplying arteries, 47 (85.45%) were derived from the descending thoracic aorta, 1 (1.82%) from the abdominal aorta, 7 (12.73%) from the celiac axis, and 1 (1.82%) from the bronchial artery. The draining vessels were the pulmonary veins in 49 patients (89.09%), the umbilical vein in 1 (1.82%), the venae intercostal in 1 (1.82%), the pulmonary arteries in 11 (20.00%), and the vessels were not shown on the images in 2 patients (3.64%). Conclusion: Clinical presentations of PS are non-specific and can be easily missed or misdiagnosed. However, CTPA can help to improve the diagnostic accuracy and identify the supplying arteries and draining vessels, which significantly contribute to surgical planning.
Full article
(This article belongs to the Section Cardiovascular Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Aerobic Exercise, Training Dose, and Cardiorespiratory Fitness: Effects and Relationships with Resting Plasma Neurotrophic Factors in Alzheimer’s Dementia
by
Dereck L. Salisbury, Danni Li, Michael Todd, Ted K. S. Ng and Fang Yu
J. Vasc. Dis. 2023, 2(3), 351-366; https://doi.org/10.3390/jvd2030027 - 01 Sep 2023
Abstract
Background: Vascular health is increasingly recognized for its roles in the pathogenesis and progression of Alzheimer’s disease (AD). The objective of this study was to investigate effects of exercise training, dose, and cardiorespiratory fitness (CRF) on neurotrophic factors in community-dwelling, older adults with
[...] Read more.
Background: Vascular health is increasingly recognized for its roles in the pathogenesis and progression of Alzheimer’s disease (AD). The objective of this study was to investigate effects of exercise training, dose, and cardiorespiratory fitness (CRF) on neurotrophic factors in community-dwelling, older adults with mild-to-moderate AD dementia. Methods: This was a pilot blood ancillary study of the FIT-AD trial. Participants in the parent study were randomized to 6-month aerobic exercise (AEx) or stretching control. For this ancillary study, resting plasma brain-derived neurotrophic factor (BDNF), irisin, fibroblast growth factor-21 (FGF-21), and insulin-like growth factor-1 (IGF-1) biomarkers were assessed at baseline, 3, and 6 months. Estimates of within- and between- group effect sizes were calculated (Cohen’s d). Relationships of biomarker change with dose and CRF change were explored with multivariable linear regression and repeated measures correlations. Results: The sample (n = 26, 18 AEx/8 stretching) averaged 77.6 ± 6.9 years old, with the majority being male (65.4%), and non-Hispanic White (92.3%); between-group effect sizes were generally small except for irisin (d = −0.44)), AEx group relative to stretching group. Associations of dose and changes in CRF with changes in neurotrophic biomarker were weak (r2 ≤ 0.025). Conclusions: The effects of exercise on BDNF, irisin, IGF-1, and FGF-21 were heterogeneous in AD. Our findings need validation in future, adequately powered exercise studies in AD.
Full article
(This article belongs to the Section Neurovascular Diseases)
►▼
Show Figures
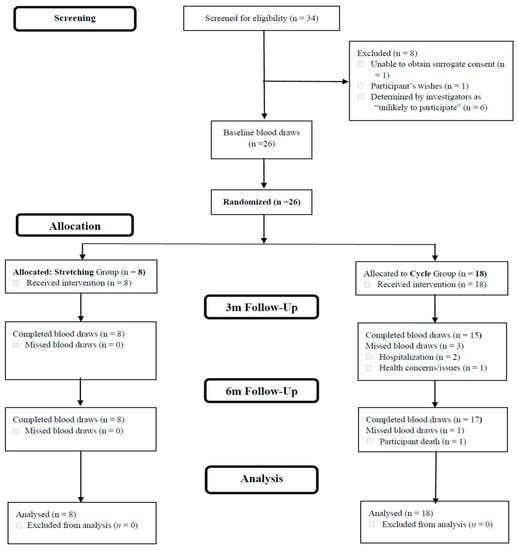
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
JCM, JPM, JVD, Diagnostics, Cancers
Diagnosis, Management, and Prognostic Assessment of Chronic Disease
Topic Editors: Xiude Fan, Enfa Zhao, Yang Xia, Shanshan Shao, Tatsunori Miyata, Dongxing XieDeadline: 5 July 2025
Topic in
JCM, Diagnostics, JPM, Brain Sciences, JVD
Diagnosis and Management of Acute Ischemic Stroke
Topic Editors: Hyo Suk Nam, Byung Moon Kim, Tae-jin Song, Minho HanDeadline: 20 September 2025

Conferences
Special Issues
Special Issue in
JVD
Molecular and Cellular Therapeutic Targets of Aortic Aneurysm
Guest Editor: Yanming LiDeadline: 5 September 2024
Special Issue in
JVD
Therapies for Age-Linked Human Vascular Diseases Using In Vitro and In Vivo Models
Guest Editors: Pazhanichamy Kalailingam, Suresh VeeraperumalDeadline: 7 June 2025