Pelvic Instability: Currents Insights (Closed)
A topical collection in Journal of Clinical Medicine (ISSN 2077-0383). This collection belongs to the section "Orthopedics".
Viewed by 37427Editor
Interests: pelvic instability; pelvic reconstruction; non-union; bone regeneration; post fracture fixation complications
Special Issues, Collections and Topics in MDPI journals
Topical Collection Information
Dear Colleagues,
Pelvic instability is a clinical entity usually seen in the female patient population secondary to post-partum ligamentous laxity and hypermobility syndrome. In males, instability can occur due to degenerative conditions but also due to poorly stabilized pelvic fractures that continue to have a degree of mechanical instability.
Chronic pain and functional restriction, amongst others, represent the hallmark of the syndrome. Non-operative treatment modalities may provide temporary suppression of symptoms, but the ultimate treatment is the surgical reconstruction of the pelvic ring in the form of fusion. Management of this condition involves a variety of clinicians and specialties, as well as a combined interdisciplinary approach.
Despite the extensive clinical interest and the availability of several related publications, there is still a lack of consensus regarding the incidence, clinical manifestations, pathophysiology, diagnostics, treatment algorithms, and the final outcome of surgical reconstruction.
We invite both clinicians and scientists to contribute their work in this Special Issue focusing on this important clinical entity with the ultimate aim to advance further our understanding and the results of surgical treatment.
Prof. Dr. Peter V. Giannoudis
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Post-partum
- Pelvic instability
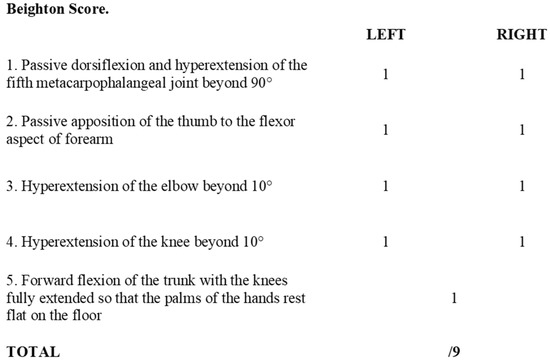
- Hypermobility
- Pubis symphysis dysfunction
- Pelvic fusion
- Sacroiliac joint fusion