Advances in Neurostimulation: Understanding of the Mechanisms and Clinical Applications
(Closed)
Share This Topical Collection
Editors
 Prof. Dr. Chris Baeken
Prof. Dr. Chris Baeken
 Prof. Dr. Chris Baeken
Prof. Dr. Chris Baeken
E-Mail
Website
Collection Editor
1. Department of Psychiatry and Medical Psychology, Ghent Experimental Psychiatry (GHEP) Lab, Universiteit Gent - C, Heymanslaan 10, 9000 Gent, Belgium
2. Department of Psychiatry, UZBrussel, Laarbeeklaan 103, 1090 Brussels, Belgium
3. Eindhoven University of Technology, Department of Electrical Engineering, The Netherlands
Interests: brain stimulation; psychiatry; brain imaging; neuroscience; treatment-resistance
 Dr. Virginie Moulier
Dr. Virginie Moulier
 Dr. Virginie Moulier
Dr. Virginie Moulier
E-Mail
Website
Collection Editor
1. University Department of Psychiatry, Centre Hospitalier du Rouvray, Sotteville-lès-Rouen, France
2. Unité de Recherche Clinique (URC), EPS Ville Evrard, Neuilly-sur-Marne, France
Interests: neurostimulation (rTMS, ECT, tDCS); emotion processing; mood disorder; structural and functional neuroimaging; pedophilia; sexual disorders; sexual molesters
Topical Collection Information
Dear Colleagues,
Brain stimulation methods been part of the clinical routine in psychiatry for several years, offering a therapeutic alternative to pharmacological and psychotherapeutic treatments. Whether they are noninvasive brain stimulation techniques, such as repetitive transcranial magnetic stimulation (rTMS), transcranial direct current stimulation (TDCS) or electroconvulsive therapy (ECT), or more invasive techniques, such as deep brain stimulation (DBS) or (transcunaneous) vagus nerve stimulation ((t)VNS), they demonstrate efficacy in several psychiatric disorders, including when those disorders have proven resistant to the current treatment algorithms. There is no doubt that new clinical applications will emerge or have their efficacy confirmed in the coming years. Identifying the factors of clinical response or resistance to these techniques is important for the optimization of therapeutic outcomes.
However, the physiological mechanisms underlying neurostimulation are not yet fully understood. Exploring the effects of these techniques with brain activity measures (functional magnetic resonance imaging (fMRI), positron emission tomography (PET) or electroencephalography (EEG), etc.) or biological measures (hormones, neuroplasticity, inflammation, etc.) can help us to better understand the neurobiological bases of these methods.
Besides neuropsychiatry, this Topical Collection also seeks to promote new effective clinical applications in brain stimulation, such as personality or somatic disorders, and advances in understanding of their mechanisms, including studies with healthy subjects.
Original research articles, systematic reviews/meta-analyses are welcome.
Prof. Dr. Chris Baeken
Dr. Virginie Moulier
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs).
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- Brain stimulation
- rTMS
- TDCS
- ECT
- DBS
- VNS
- Brain imaging
Published Papers (16 papers)
Open AccessReview
Revisiting the Rotational Field TMS Method for Neurostimulation
by
Yiftach Roth, Samuel Zibman, Gaby S. Pell, Abraham Zangen and Aron Tendler
Cited by 1 | Viewed by 1675
Abstract
Transcranial magnetic stimulation (TMS) is a non-invasive technique that has shown high efficacy in the treatment of major depressive disorder (MDD) and is increasingly utilized for various neuropsychiatric disorders. However, conventional TMS is limited to activating only a small fraction of neurons that
[...] Read more.
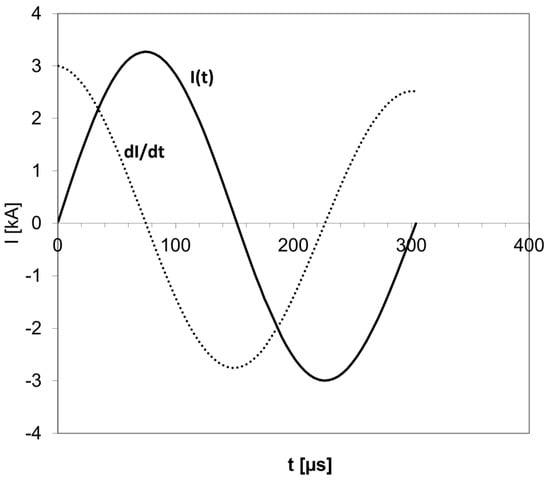
Transcranial magnetic stimulation (TMS) is a non-invasive technique that has shown high efficacy in the treatment of major depressive disorder (MDD) and is increasingly utilized for various neuropsychiatric disorders. However, conventional TMS is limited to activating only a small fraction of neurons that have components parallel to the induced electric field. This likely contributes to the significant variability observed in clinical outcomes. A novel method termed rotational field TMS (rfTMS or TMS 360°) enables the activation of a greater number of neurons by reducing the sensitivity to orientation. Recruitment of a larger number of neurons offers the potential to enhance efficacy and reduce variability in the treatment of clinical indications for which neuronal recruitment and organization may play a significant role, such as MDD and stroke. The potential of the method remains to be validated in clinical trials. Here, we revisit and describe in detail the rfTMS method, its principles, mode of operation, effects on the brain, and potential benefits for clinical TMS.
Full article
►▼
Show Figures
Open AccessReview
Efficacy and Safety of Transcranial Electric Stimulation during the Perinatal Period: A Systematic Literature Review and Three Case Reports
by
Andrew Laurin, Noémie Nard, Marine Dalmont, Samuel Bulteau, Cloé Bénard, Olivier Bonnot, Norbert Winer, Françoise Dupont, Gisèle Apter, Frédérique Terranova-Commessie, Olivier Guillin, Wissam El-Hage, Anne Sauvaget and Maud Rothärmel
Cited by 4 | Viewed by 2313
Abstract
Introduction: The perinatal period is an at-risk period for the emergence or decompensation of psychiatric disorders. Transcranial electrical stimulation (tES) is an effective and safe treatment for many psychiatric disorders. Given the reluctance to use pharmacological treatments during pregnancy or breastfeeding, tES
[...] Read more.
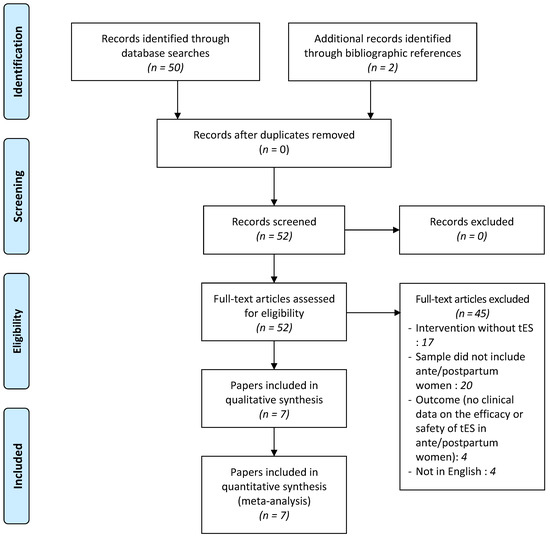
Introduction: The perinatal period is an at-risk period for the emergence or decompensation of psychiatric disorders. Transcranial electrical stimulation (tES) is an effective and safe treatment for many psychiatric disorders. Given the reluctance to use pharmacological treatments during pregnancy or breastfeeding, tES may be an interesting treatment to consider. Our study aims to evaluate the efficacy and safety of tES in the perinatal period through a systematic literature review followed by three original case reports.
Method: Following PRISMA guidelines, a systematic review of MEDLINE and ScienceDirect was undertaken to identify studies on tES on women during the perinatal period. The initial research was conducted until 31 December 2021 and search terms included: tDCS, transcranial direct current stimulation, tACS, transcranial alternating current stimulation, tRNS, transcranial random noise stimulation, pregnancy, perinatal, postnatal, and postpartum.
Results: Seven studies reporting on 33 women during the perinatal period met the eligibility criteria. No serious adverse effects for the mother or child were reported. Data were limited to the use of tES during pregnancy in patients with schizophrenia or unipolar depression. In addition, we reported three original case reports illustrating the efficacy and safety of tDCS: in a pregnant woman with bipolar depression, in a pregnant woman with post-traumatic stress disorder (sham tDCS), and in a breastfeeding woman with postpartum depression.
Conclusions: The results are encouraging, making tES a potentially safe and effective treatment in the perinatal period. Larger studies are needed to confirm these initial results, and any adverse effects on the mother or child should be reported. In addition, research perspectives on the medico-economic benefits of tES, and its realization at home, are to be investigated in the future.
Full article
►▼
Show Figures
Open AccessArticle
Neuromodulation Using Transcranial Focused Ultrasound on the Bilateral Medial Prefrontal Cortex
by
Young Goo Kim, Song E. Kim, Jihye Lee, Sungeun Hwang, Seung-Schik Yoo and Hyang Woon Lee
Cited by 10 | Viewed by 4034
Abstract
Transcranial focused ultrasound (tFUS) is a promising technique of non-invasive brain stimulation for modulating neuronal activity with high spatial specificity. The medial prefrontal cortex (mPFC) has been proposed as a potential target for neuromodulation to prove emotional and sleep qualities. We aim to
[...] Read more.
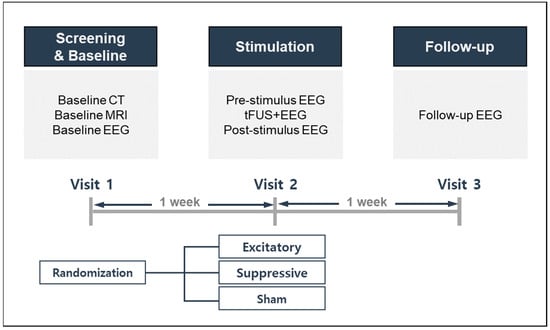
Transcranial focused ultrasound (tFUS) is a promising technique of non-invasive brain stimulation for modulating neuronal activity with high spatial specificity. The medial prefrontal cortex (mPFC) has been proposed as a potential target for neuromodulation to prove emotional and sleep qualities. We aim to set up an appropriate clinical protocol for investigating the effects of tFUS stimulation of the bilateral mPFC for modulating the function of the brain-wide network using different sonication parameters. Seven participants received 20 min of 250 kHz tFUS to the bilateral mPFC with excitatory (70% duty cycle with sonication interval at 5 s) or suppressive (5% duty cycle with no interval) sonication protocols, which were compared to a sham condition. By placing the cigar-shaped sonication focus on the falx between both mPFCs, it was possible to simultaneously stimulate the bilateral mPFCs. Brain activity was analyzed using continuous electroencephalographic (EEG) recording during, before, and after tFUS. We investigated whether tFUS stimulation under the different conditions could lead to distinctive changes in brain activity in local brain regions where tFUS was directly delivered, and also in adjacent or remote brain areas that were not directly stimulated. This kind of study setting suggests that dynamic changes in brain cortical responses can occur within short periods of time, and that the distribution of these responses may differ depending on local brain states and functional brain architecture at the time of tFUS administration, or perhaps, at least temporarily, beyond the stimulation time. If so, tFUS could be useful for temporarily modifying regional brain activity, modulating functional connectivity, or reorganizing brain functions associated with various neuropsychiatric diseases, such as insomnia and depression.
Full article
►▼
Show Figures
Open AccessReview
Benefits from Repetitive Transcranial Magnetic Stimulation in Post-Stroke Rehabilitation
by
Michał Starosta, Natalia Cichoń, Joanna Saluk-Bijak and Elżbieta Miller
Cited by 18 | Viewed by 4930
Abstract
Stroke is an acute neurovascular central nervous system (CNS) injury and one of the main causes of long-term disability and mortality. Post-stroke rehabilitation as part of recovery is focused on relearning lost skills and regaining independence as much as possible. Many novel strategies
[...] Read more.
Stroke is an acute neurovascular central nervous system (CNS) injury and one of the main causes of long-term disability and mortality. Post-stroke rehabilitation as part of recovery is focused on relearning lost skills and regaining independence as much as possible. Many novel strategies in neurorehabilitation have been introduced. This review focuses on current evidence of the effectiveness of repetitive transcranial magnetic stimulation (rTMS), a noninvasive brain stimulation (NIBS), in post-stroke rehabilitation. Moreover, we present the effects of specific interventions, such as low-frequency or high-frequency rTMS therapy, on motor function, cognitive function, depression, and aphasia in post-stroke patients. Collected data suggest that high-frequency stimulation (5 Hz and beyond) produces an increase in cortical excitability, whereas low-frequency stimulation (≤1 Hz) decreases cortical excitability. Accumulated data suggest that rTMS is safe and can be used to modulate cortical excitability, which may improve overall performance. Side effects such as tingling sensation on the skin of the skull or headache are possible. Serious side effects such as epileptic seizures can be avoided by adhering to international safety guidelines. We reviewed clinical studies that present promising results in general recovery and stimulating neuroplasticity. This article is an overview of the current rTMS state of knowledge related to benefits in stroke, as well as its cellular and molecular mechanisms. In the stroke rehabilitation literature, there is a key methodological problem of creating double-blinding studies, which are very often impossible to conduct.
Full article
Open AccessReview
Understanding the Effects of Transcranial Electrical Stimulation in Numerical Cognition: A Systematic Review for Clinical Translation
by
Giulia Lazzaro, Elisa Fucà, Cristina Caciolo, Andrea Battisti, Floriana Costanzo, Cristiana Varuzza, Stefano Vicari and Deny Menghini
Cited by 6 | Viewed by 2461
Abstract
Atypical development of numerical cognition (dyscalculia) may increase the onset of neuropsychiatric symptoms, especially when untreated, and it may have long-term detrimental social consequences. However, evidence-based treatments are still lacking. Despite plenty of studies investigating the effects of transcranial electrical stimulation (tES) on
[...] Read more.
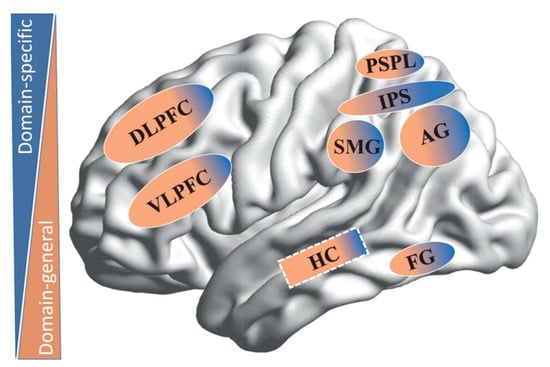
Atypical development of numerical cognition (dyscalculia) may increase the onset of neuropsychiatric symptoms, especially when untreated, and it may have long-term detrimental social consequences. However, evidence-based treatments are still lacking. Despite plenty of studies investigating the effects of transcranial electrical stimulation (tES) on numerical cognition, a systematized synthesis of results is still lacking. In the present systematic review (PROSPERO ID: CRD42021271139), we found that the majority of reports (20 out of 26) showed the effectiveness of tES in improving both number (80%) and arithmetic (76%) processing. In particular, anodal tDCS (regardless of lateralization) over parietal regions, bilateral tDCS (regardless of polarity/lateralization) over frontal regions, and tRNS (regardless of brain regions) strongly enhance number processing. While bilateral tDCS and tRNS over parietal and frontal regions and left anodal tDCS over frontal regions consistently improve arithmetic skills. In addition, tACS seems to be more effective than tDCS at ameliorating arithmetic learning. Despite the variability of methods and paucity of clinical studies, tES seems to be a promising brain-based treatment to enhance numerical cognition. Recommendations for clinical translation, future directions, and limitations are outlined.
Full article
►▼
Show Figures
Open AccessArticle
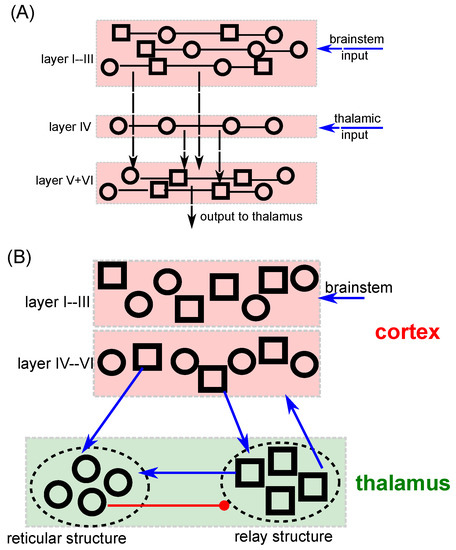
Mathematical Model Insights into EEG Origin under Transcranial Direct Current Stimulation (tDCS) in the Context of Psychosis
by
Joséphine Riedinger and Axel Hutt
Cited by 3 | Viewed by 2214
Abstract
Schizophrenia is a psychotic disease that develops progressively over years with a transition from prodromal to psychotic state associated with a disruption in brain activity. Transcranial Direct Current Stimulation (tDCS), known to alleviate pharmaco-resistant symptoms in patients suffering from schizophrenia, promises to prevent
[...] Read more.
Schizophrenia is a psychotic disease that develops progressively over years with a transition from prodromal to psychotic state associated with a disruption in brain activity. Transcranial Direct Current Stimulation (tDCS), known to alleviate pharmaco-resistant symptoms in patients suffering from schizophrenia, promises to prevent such a psychotic transition. To understand better how tDCS affects brain activity, we propose a neural cortico-thalamo-cortical (CTC) circuit model involving the Ascending Reticular Arousal System (ARAS) that permits to describe major impact features of tDCS, such as excitability for short-duration stimulation and electroencephalography (EEG) power modulation for long-duration stimulation. To this end, the mathematical model relates stimulus duration and Long-Term Plasticity (LTP) effect, in addition to describing the temporal LTP decay after stimulus offset. This new relation promises to optimize future stimulation protocols. Moreover, we reproduce successfully EEG-power modulation under tDCS in a ketamine-induced psychosis model and confirm the N-methyl-d-aspartate (NMDA) receptor hypofunction hypothesis in the etiopathophysiology of schizophrenia. The model description points to an important role of the ARAS and the
-rhythm synchronicity in CTC circuit in early-stage psychosis.
Full article
►▼
Show Figures
Open AccessArticle
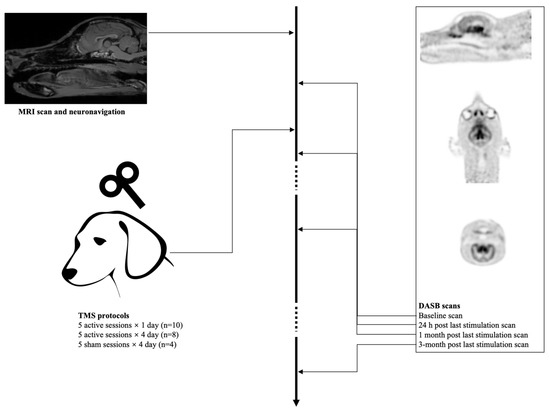
Accelerated HF-rTMS Modifies SERT Availability in the Subgenual Anterior Cingulate Cortex: A Canine [11C]DASB Study on the Serotonergic System
by
Yangfeng Xu, Mitchel Kappen, Kathelijne Peremans, Dimitri De Bundel, Ann Van Eeckhaut, Nick Van Laeken, Filip De Vos, Andre Dobbeleir, Jimmy H. Saunders and Chris Baeken
Cited by 1 | Viewed by 2220
Abstract
Repetitive transcranial magnetic stimulation (rTMS) is thought to partly exert its antidepressant action through the serotonergic system. Accelerated rTMS may have the potential to result in similar but faster onset of clinical improvement compared to the classical daily rTMS protocols, but given that
[...] Read more.
Repetitive transcranial magnetic stimulation (rTMS) is thought to partly exert its antidepressant action through the serotonergic system. Accelerated rTMS may have the potential to result in similar but faster onset of clinical improvement compared to the classical daily rTMS protocols, but given that delayed clinical responses have been reported, the neurobiological effects of accelerated paradigms remain to be elucidated including on this neurotransmitter system. This sham-controlled study aimed to evaluate the effects of accelerated high frequency rTMS (aHF-rTMS) over the left frontal cortex on the serotonin transporter (SERT) in healthy beagle dogs. A total of twenty-two dogs were randomly divided into three unequal groups: five active stimulation sessions (five sessions in one day,
n = 10), 20 active stimulation sessions (five sessions/day for four days,
n = 8), and 20 sham stimulation sessions (five sessions/day for four days,
n = 4). The SERT binding index (BI) was obtained at baseline, 24 h post stimulation protocol, one month, and three months post stimulation by a [
11C]DASB PET scan. It was found that one day of active aHF-rTMS (five sessions) did not result in significant SERT BI changes at any time point. For the 20 sessions of active aHF-rTMS, one month after stimulation the SERT BI attenuated in the sgACC. No significant SERT BI changes were found after 20 sessions of sham aHF-rTMS. A total of four days of active aHF-rTMS modified sgACC SERT BI one month post-stimulation, explaining to some extent the delayed clinical effects of accelerated rTMS paradigms found in human psychopathologies.
Full article
►▼
Show Figures
Open AccessArticle
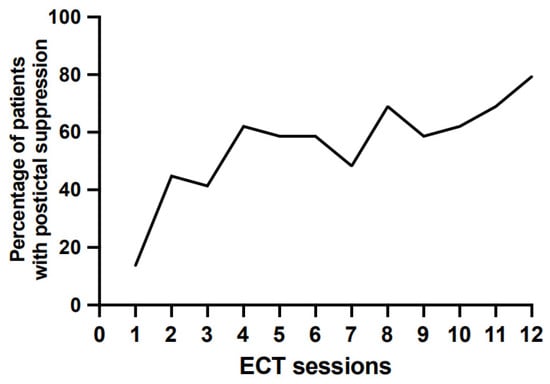
A Retrospective Study of Postictal Suppression during Electroconvulsive Therapy
by
Virginie Moulier, Julien Guehl, Emilie Evêque-Mourroux, Pierre Quesada and Maud Rothärmel
Cited by 3 | Viewed by 1574
Abstract
Background: electroconvulsive therapy (ECT) is the most effective treatment in treatment-resistant depression (TRD), but its response remains partial. Identifying useful indicators to guide decision making for treatment and improve clinical response remains a major issue. The objective of the present retrospective study was
[...] Read more.
Background: electroconvulsive therapy (ECT) is the most effective treatment in treatment-resistant depression (TRD), but its response remains partial. Identifying useful indicators to guide decision making for treatment and improve clinical response remains a major issue. The objective of the present retrospective study was to determine if clinical response—early (after 5 ECT sessions) or longer-term (after 12 ECT sessions)—was associated with postictal suppression during the first ECT course and/or with postictal suppression frequency during the whole ECT course. Methods: in a retrospective study, the data of 42 patients suffering from treatment-resistant depression and receiving at least 5 ECT sessions were collected. Two sessions per week of bitemporal brief-pulse ECT sessions were administered to patients. Each of the electroencephalography (EEG) recordings were assessed to determine the presence of postictal suppression. Results: the postictal suppression from the first ECT session predicted a better long-term clinical response (after 12 ECT sessions), but not early clinical response (after only 5 ECT sessions). The postictal suppression frequency was associated with neither the short- nor the long-term clinical response. In addition, postictal suppression and short-term cognitive performances were not associated. Conclusions: this EEG indicator is clinically useful if it appears in the first ECT sessions, but it is no longer relevant in the following sessions.
Full article
►▼
Show Figures
Open AccessArticle
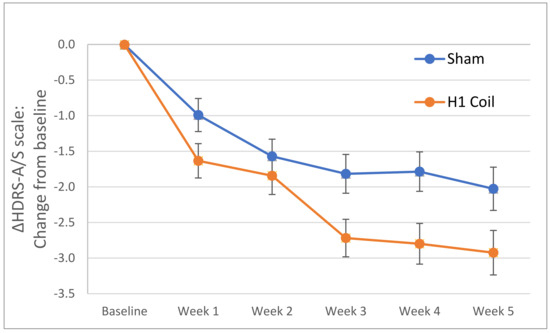
Efficacy of Deep TMS with the H1 Coil for Anxious Depression
by
Gaby S. Pell, Tal Harmelech, Sam Zibman, Yiftach Roth, Aron Tendler and Abraham Zangen
Cited by 12 | Viewed by 3554
Abstract
(1) Background: While the therapeutic efficacy of Transcranial Magnetic Stimulation (TMS) for major depressive disorder (MDD) is well established, less is known about the technique’s efficacy for treating comorbid anxiety. (2) Methods: Data were retrospectively analyzed from randomized controlled trials (RCTs) that used
[...] Read more.
(1) Background: While the therapeutic efficacy of Transcranial Magnetic Stimulation (TMS) for major depressive disorder (MDD) is well established, less is known about the technique’s efficacy for treating comorbid anxiety. (2) Methods: Data were retrospectively analyzed from randomized controlled trials (RCTs) that used Deep TMS with the H1 Coil for MDD treatment. The primary endpoint was the difference relative to sham treatment following 4 weeks of stimulation. The effect size was compared to literature values for superficial TMS and medication treatments. (3) Results: In the pivotal RCT, active Deep TMS compared with sham treatment showed significantly larger improvements in anxiety score (effect size = 0.34,
p = 0.03 (FDR)) which were sustained until 16 weeks (effect size = 0.35,
p = 0.04). The pooled effect size between all the RCTs was 0.55, which compares favorably to alternative treatments. A direct comparison to Figure-8 Coil treatment indicated that treatment with the H1 Coil was significantly more effective (
p = 0.042). In contrast to previously reported studies using superficial TMS and medication for which anxiety has been shown to be a negative predictor of effectiveness, higher baseline anxiety was found to be predictive of successful outcome for the H1-Coil treatment. (4) Conclusions: Deep TMS is effective in treating comorbid anxiety in MDD and, unlike alternative treatments, the outcome does not appear to be adversely affected by high baseline anxiety levels.
Full article
►▼
Show Figures
Open AccessArticle
Ten Sessions of 30 Min tDCS over 5 Days to Achieve Remission in Depression: A Randomized Pilot Study
by
Rémi Moirand, Laetitia Imbert, Frédéric Haesebaert, Gabrielle Chesnoy, Benoit Bediou, Emmanuel Poulet and Jérôme Brunelin
Cited by 5 | Viewed by 2821
Abstract
Although transcranial Direct Current stimulation (tDCS) shows promise in the treatment of major depressive episodes, the optimal parameters and population to target remain unclear. We investigated the clinical interest of a 10 session tDCS regimen in patients with mild to severe treatment-resistant depression,
[...] Read more.
Although transcranial Direct Current stimulation (tDCS) shows promise in the treatment of major depressive episodes, the optimal parameters and population to target remain unclear. We investigated the clinical interest of a 10 session tDCS regimen in patients with mild to severe treatment-resistant depression, in a pilot double-blind, randomized sham-controlled trial. tDCS was delivered over 5 consecutive days (two 30 min sessions per day separated by at least 2 h, 2 mA). The anode and cathode were placed over the left and the right dorsolateral prefrontal cortex, respectively. One month after tDCS, we observed significantly fewer patients who achieved remission (MADRS
10 < 10) in the sham group (0 out of 18 patients) than in the active group (5 out of 21 patients;
p = 0.05). However, no significant difference was observed between the groups regarding the mean scores of severity changes throughout the study period. Bifrontal add-on tDCS delivered twice per day over 5 days, in combination with antidepressant medication, can be a safe and suitable approach to achieve remission in patients with mild to severe treatment-resistant major depressive disorder. However, in regards to the pilot nature and limitations of the present study, further studies are needed before any frank conclusions can be made regarding the use of tDCS with the proposed parameters in clinical settings.
Full article
►▼
Show Figures
Open AccessReview
Repetitive Transcranial Magnetic Stimulation (rTMS) as a Promising Treatment for Craving in Stimulant Drugs and Behavioral Addiction: A Meta-Analysis
by
Aurélia Gay, Julien Cabe, Ingrid De Chazeron, Céline Lambert, Maxime Defour, Vikesh Bhoowabul, Thomas Charpeaud, Aurore Tremey, Pierre-Michel Llorca, Bruno Pereira and Georges Brousse
Cited by 11 | Viewed by 7088
Abstract
Addiction is a mental disorder with limited available treatment options. The therapeutic potential of repetitive transcranial magnetic stimulation (rTMS) on it, by targeting craving in particular, has been explored with heterogenous results. This meta-analysis uses updated evidence to assess overall rTMS efficacy on
[...] Read more.
Addiction is a mental disorder with limited available treatment options. The therapeutic potential of repetitive transcranial magnetic stimulation (rTMS) on it, by targeting craving in particular, has been explored with heterogenous results. This meta-analysis uses updated evidence to assess overall rTMS efficacy on craving, differential effects between addiction types clustered into three groups (depressant (alcohol, cannabis, opiate), stimulant (nicotine, cocaine, methamphetamine), and behavioral addiction (gambling, eating disorder)), and stimulation settings. Studies on substance use, gambling, and eating disorders are included, with unrestricted stimulation settings, by searching the PubMed, Embase, PsycINFO, and Cochrane databases up to 30 April 2020. A total of 34 eligible studies (42 units of analysis) were identified. Because of highly significant heterogeneity in primary results, a sensitivity analysis was performed on a remaining sample of 26 studies (30 units of analysis). Analyses performed using random effects model revealed a small effect size favoring active rTMS over shamTMS stimulation in the reduction in craving. We found a significant difference between addiction types, with a persistent small effect only for stimulant and behavioral groups. In these groups we found no difference between the different combinations of target and frequency of stimulation, but a significant correlation between number of sessions and craving reduction. In conclusion, efficacy of rTMS on craving in stimulant and behavioral addiction was highlighted, but recommendations on optimal stimulation settings and its clinical application await further research.
Full article
►▼
Show Figures
Open AccessArticle
Feasibility of Combining Transcranial Direct Current Stimulation and Active Fully Embodied Virtual Reality for Visual Height Intolerance: A Double-Blind Randomized Controlled Study
by
Samuel Bulteau, Andrew Laurin, Kalyane Bach-Ngohou, Morgane Péré, Marie-Anne Vibet, Jean-Benoit Hardouin, Véronique Sebille, Lydie Lagalice, Élodie Faurel-Paul, Didier Acier, Thomas Rabeyron, Valéry-Pierre Riche, Anne Sauvaget, Florian Melki, Toinon Vigier, Matthieu Perreira Da Silva, Olivier Charlet and Yannick Prié
Cited by 5 | Viewed by 3307
Abstract
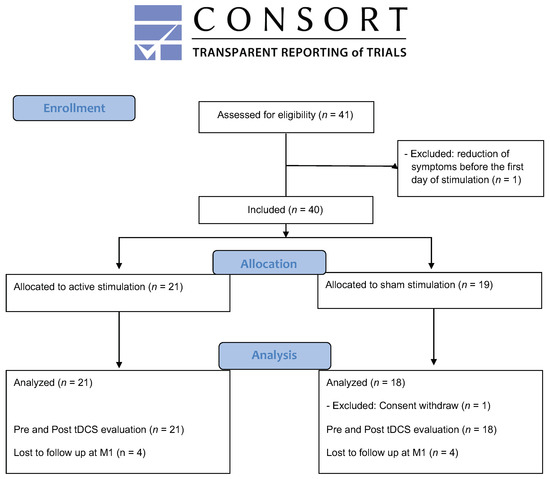
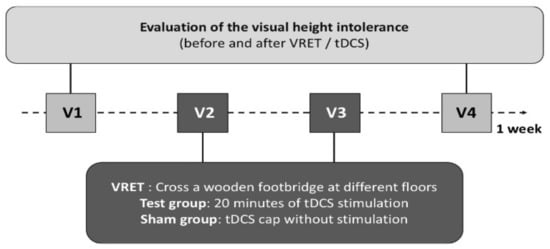
Background: Transcranial Direct Current Stimulation (tDCS) and Virtual Reality Exposure Therapy (VRET) are individually increasingly used in psychiatric research. Objective/Hypothesis: Our study aimed to investigate the feasibility of combining tDCS and wireless 360° full immersive active and embodied VRET to reduce height-induced anxiety.
[...] Read more.
Background: Transcranial Direct Current Stimulation (tDCS) and Virtual Reality Exposure Therapy (VRET) are individually increasingly used in psychiatric research. Objective/Hypothesis: Our study aimed to investigate the feasibility of combining tDCS and wireless 360° full immersive active and embodied VRET to reduce height-induced anxiety. Methods: We carried out a pilot randomized, double-blind, controlled study associating VRET (two 20 min sessions with a 48 h interval, during which, participants had to cross a plank at rising heights in a building in construction) with online tDCS (targeting the ventromedial prefrontal cortex) in 28 participants. The primary outcomes were the sense of presence level and the tolerability. The secondary outcomes were the anxiety level (Subjective Unit of Discomfort) and the salivary cortisol concentration. Results: We confirmed the feasibility of the association between tDCS and fully embodied VRET associated with a good sense of presence without noticeable adverse effects. In both groups, a significant reduction in the fear of height was observed after two sessions, with only a small effect size of add-on tDCS (0.1) according to the SUD. The variations of cortisol concentration differed in the tDCS and sham groups. Conclusion: Our study confirmed the feasibility of the association between wireless online tDCS and active, fully embodied VRET. The optimal tDCS paradigm remains to be determined in this context to increase effect size and then adequately power future clinical studies assessing synergies between both techniques.
Full article
►▼
Show Figures
Open AccessArticle
Cerebellar Transcranial Direct Current Stimulation in Children with Autism Spectrum Disorder: A Pilot Study on Efficacy, Feasibility, Safety, and Unexpected Outcomes in Tic Disorder and Epilepsy
by
Giordano D’Urso, Elena Toscano, Veronica Sanges, Anne Sauvaget, Christine E. Sheffer, Maria Pia Riccio, Roberta Ferrucci, Felice Iasevoli, Alberto Priori, Carmela Bravaccio and Andrea de Bartolomeis
Cited by 13 | Viewed by 2744
Abstract
Patients with autism spectrum disorder (ASD) display distinctive neurophysiological characteristics associated with significant cognitive, emotional, and behavioral symptoms. Transcranial direct current stimulation (tDCS) applied to the frontal or temporoparietal lobes has demonstrated potential to reduce the severity of ASD-related symptoms. Recently, the cerebellum
[...] Read more.
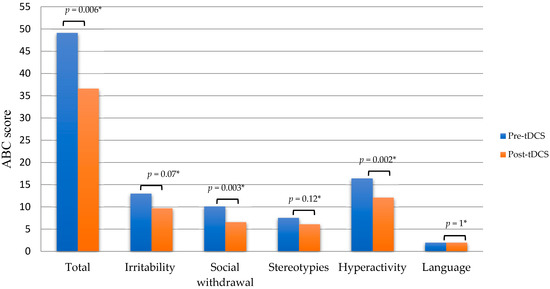
Patients with autism spectrum disorder (ASD) display distinctive neurophysiological characteristics associated with significant cognitive, emotional, and behavioral symptoms. Transcranial direct current stimulation (tDCS) applied to the frontal or temporoparietal lobes has demonstrated potential to reduce the severity of ASD-related symptoms. Recently, the cerebellum has been identified as a brain area involved in ASD pathophysiology. In this open-label pilot study, seven ASD patients aged between 9 and 13 years underwent 20 daily sessions of 20 min cathodal stimulation of the right cerebellar lobe. At the end of the treatment, the Aberrant Behavior Checklist (ABC) scores showed a 25% mean reduction in global severity of symptoms, with a more pronounced reduction in the “social withdrawal and lethargy” (−35%), “hyperactivity and noncompliance” (−26%), and “irritability, agitation, and crying” (−25%) subscales. Minor and no improvement were observed in the “stereotypic behavior” (−18%) and “inappropriate speech” (−0%) subscales, respectively. Improvements were not detected in the two patients who were taking psychotropic drugs during the study. Clinical response showed a symptom-specific time course. Quality of sleep and mood improved earlier than hyperactivity and social withdrawal. The treatment was generally accepted by patients and well tolerated. No serious adverse events were reported. Stimulation also appeared to markedly reduce the severity of tics in a patient with comorbid tic disorder and led to the disappearance of a frontal epileptogenic focus in another patient with a history of seizures. In conclusion, cerebellar tDCS is safe, feasible, and potentially effective in the treatment of ASD symptoms among children. Strategies to improve recruitment and retention are discussed.
Full article
►▼
Show Figures
Open AccessReview
Improvement of Insight with Non-Invasive Brain Stimulation in Patients with Schizophrenia: A Systematic Review
by
Martin Blay, Ondine Adam, Rémy Bation, Filipe Galvao, Jérôme Brunelin and Marine Mondino
Cited by 9 | Viewed by 3174
Abstract
Patients with schizophrenia are often unaware of their condition and the consequences of their illness. This lack of insight results in impaired functioning, treatment non-adherence and poor prognosis. Here, we aimed to investigate the effects of non-invasive brain stimulation (NIBS) on two forms
[...] Read more.
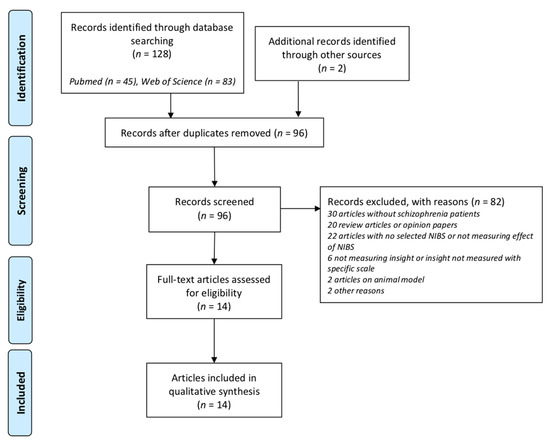
Patients with schizophrenia are often unaware of their condition and the consequences of their illness. This lack of insight results in impaired functioning, treatment non-adherence and poor prognosis. Here, we aimed to investigate the effects of non-invasive brain stimulation (NIBS) on two forms of insight, clinical and cognitive, in patients with schizophrenia. We conducted a systematic review of the literature registered in the PROSPERO database (CRD42020220323) according to PRISMA guidelines. The literature search was conducted in Medline and Web of Science databases based on studies published up until October 2020 that included pre-NIBS and post-NIBS measurements of clinical and/or cognitive insight in adults with schizophrenia. A total of 14 studies were finally included, and their methodological quality was assessed by using the QualSyst tool. Despite the lack of well-conducted large randomized-controlled studies using insight as the primary outcome, the available findings provide preliminary evidence that NIBS can improve clinical insight in patients with schizophrenia, with a majority of studies using transcranial direct current stimulation with a left frontotemporal montage. Further studies should investigate the effect of NIBS on insight as a primary outcome and how these effects on insight could translate into clinical and functional benefits in patients with schizophrenia.
Full article
►▼
Show Figures
Open AccessArticle
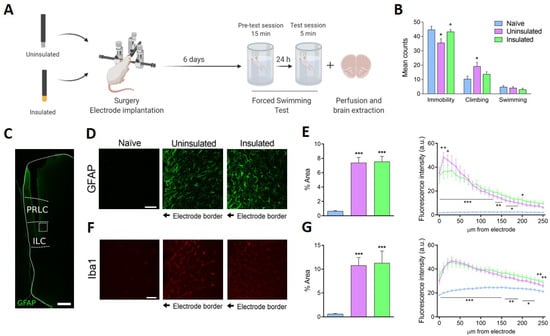
Induced Dipoles and Possible Modulation of Wireless Effects in Implanted Electrodes. Effects of Implanting Insulated Electrodes on an Animal Test to Screen Antidepressant Activity
by
Laura Perez-Caballero, Hector Carceller, Juan Nacher, Vicent Teruel-Marti, Eulalia Pujades, Nieves Casañ-Pastor and Esther Berrocoso
Cited by 2 | Viewed by 1843
Abstract
There is evidence that Deep Brain Stimulation (DBS) produces health benefits in patients even before initiating stimulation. Furthermore, DBS electrode insertion in rat infralimbic cortex (ILC) provokes antidepressant-like effects before stimulation, due to local inflammation and astrogliosis. Consequently, a significant effect of implanting
[...] Read more.
There is evidence that Deep Brain Stimulation (DBS) produces health benefits in patients even before initiating stimulation. Furthermore, DBS electrode insertion in rat infralimbic cortex (ILC) provokes antidepressant-like effects before stimulation, due to local inflammation and astrogliosis. Consequently, a significant effect of implanting electrodes is suspected. External fields, similar in magnitude to the brain’s endogenous fields, induce electric dipoles in conducting materials, in turn influencing neural cell growth through wireless effects. To elucidate if such dipoles influence depressive-like behavior, without external stimulation, the comparative effect of conducting and insulated electrodes along with the glial response is studied in unstressed rats. Naïve and implanted rats with electrically insulated or uninsulated steel electrodes were evaluated in the modified forced swimming test and expression of ILC-glial markers was assessed. An antidepressant-like effect was observed with conducting but not with insulated electrodes. Gliosis was detected in both groups, but astroglial reactivity was larger near uninsulated electrodes. Thus, induced dipoles and antidepressant-like effects were only observed with conducting implants. Such correlation suggests that dipoles induced in electrodes by endogenous fields in turn induce neuron stimulation in a feedback loop between electrodes and neural system. Further research of the effects of unwired conducting implants could open new approaches to regulating neuronal function, and possibly treat neurological disorders.
Full article
►▼
Show Figures
Open AccessArticle
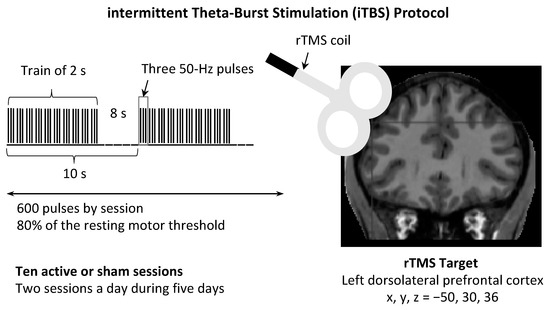
Effect of Intermittent Theta Burst Stimulation on the Neural Processing of Emotional Stimuli in Healthy Volunteers
by
Virginie Moulier, Christian Gaudeau-Bosma, Fanny Thomas, Clémence Isaac, Maxence Thomas, Florence Durand, Palmyre Schenin-King Andrianisaina, Romain Valabregue, Charles Laidi, René Benadhira, Noomane Bouaziz and Dominique Januel
Cited by 2 | Viewed by 3548
Abstract
Background: Intermittent theta burst stimulation (iTBS) is a form of repetitive transcranial magnetic stimulation that has shown to be effective in treatment-resistant depression. Through studying the effect of iTBS on healthy subjects, we wished to attain a greater understanding of its impact on
[...] Read more.
Background: Intermittent theta burst stimulation (iTBS) is a form of repetitive transcranial magnetic stimulation that has shown to be effective in treatment-resistant depression. Through studying the effect of iTBS on healthy subjects, we wished to attain a greater understanding of its impact on the brain. Our objective was to assess whether 10 iTBS sessions altered the neural processing of emotional stimuli, mood and brain anatomy in healthy subjects. Methods: In this double-blind randomized sham-controlled study, 30 subjects received either active iTBS treatment (10 sessions, two sessions a day) or sham treatment over the left dorsolateral prefrontal cortex. Assessments of mood, structural magnetic resonance imaging (MRI) and functional MRI (fMRI) were performed before and after iTBS sessions. During the fMRI, three different categories of stimuli were presented: positive, negative and neutral photographs. Results: This study showed that, during the presentation of negative stimuli (compared with neutral stimuli), 10 sessions of iTBS increased activity in the left anterior insula. However, iTBS did not induce any change in mood, regional gray matter volume or cortical thickness. Conclusions: iTBS modifies healthy subjects’ brain activity in a key region that processes emotional stimuli. (AFSSAPS: ID-RCB 2010A01032-37).
Full article
►▼
Show Figures
Planned Papers
The below list represents only planned manuscripts. Some of these
manuscripts have not been received by the Editorial Office yet. Papers
submitted to MDPI journals are subject to peer-review.
Title: Insights into EEG under transcranial direct current stimulation by a neural model
Authors: Axel Hutt and Joséphine Riedinger