The Eye in Systemic Diseases (Closed)
A topical collection in Journal of Clinical Medicine (ISSN 2077-0383). This collection belongs to the section "Ophthalmology".
Viewed by 34238Editor
Interests: neurophthalmology; neurodegenerative disorders; glaucoma; retinal diseases; retinal imaging; multiple sclerosis; hereditary ocular diseases; visual pathway; systemic lupus erythematosus; autoimmune diseases; spectral-domain- optical coherence tomography; optical coherence tomography angiography; visual field; microperimetry
Topical Collection Information
Dear Colleagues,
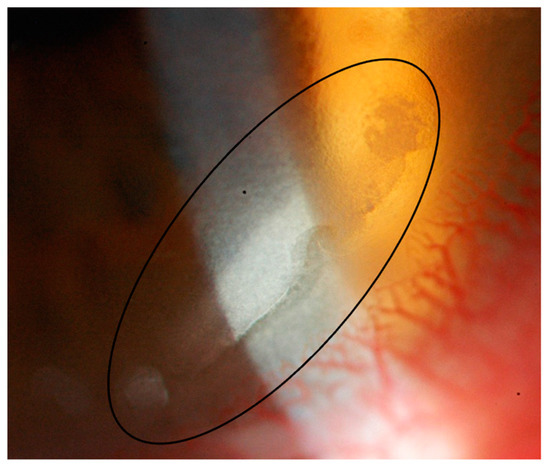
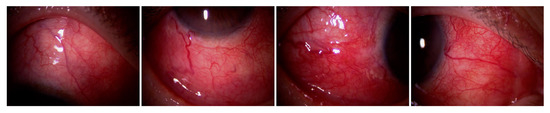
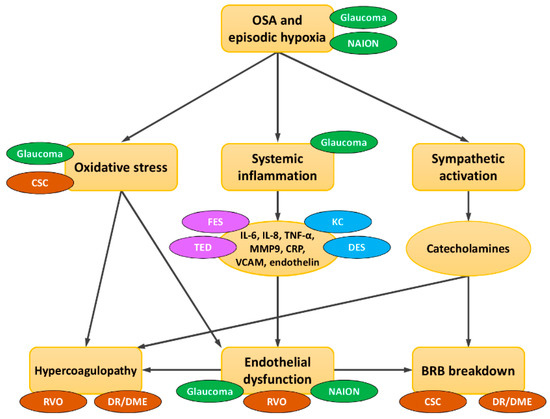
The eye can be considered a window into the human body as a whole, allowing us to detect signs that may suggest or confirm the presence of systemic disease. Moreover, an ocular manifestation may be the first visible presentation of a systemic disorder and/or may offer a relevant diagnostic clue. Ocular signs and symptoms can be present in numerous pathologies affecting different organs and systems, such as endocrine/metabolic, blood/circulatory, malignant, rheumatological/autoimmune, and neurodegenerative diseases.
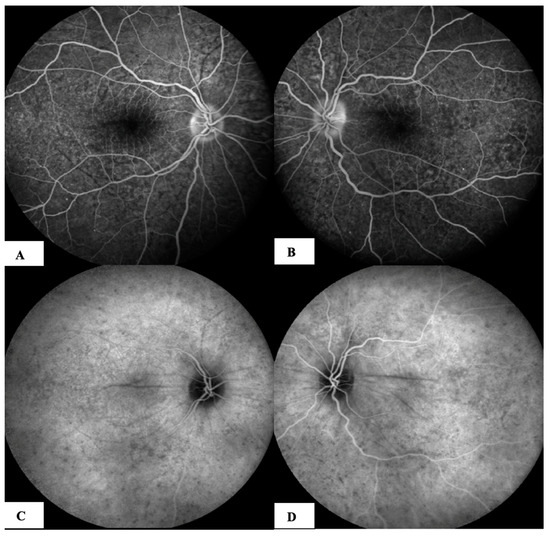
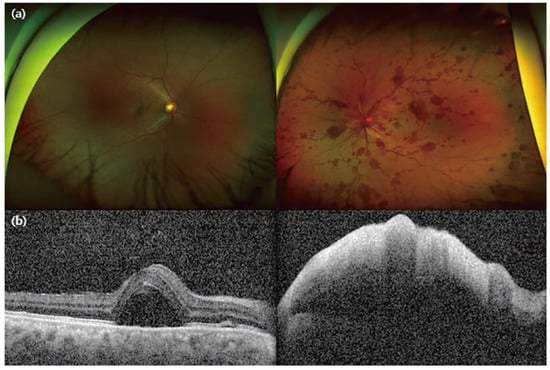
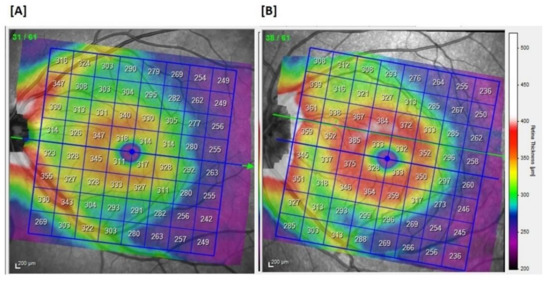
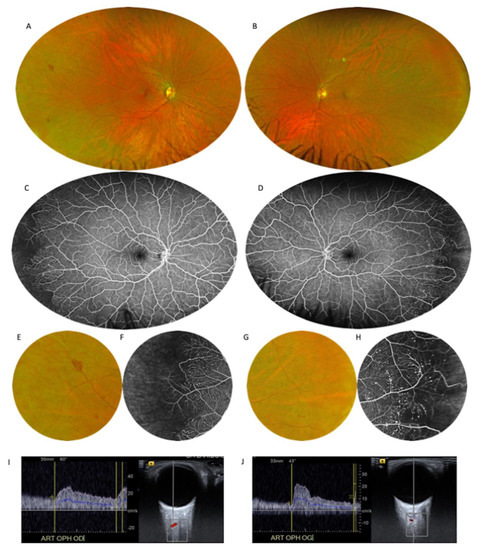
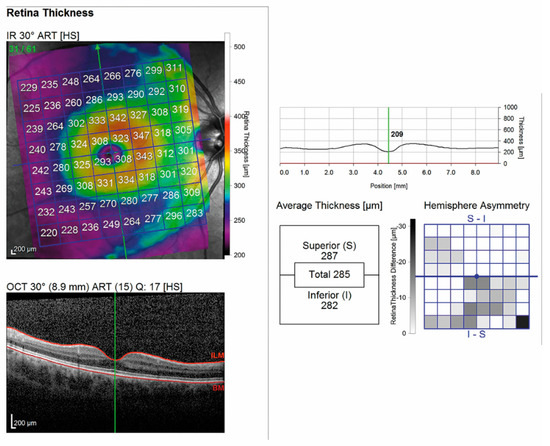
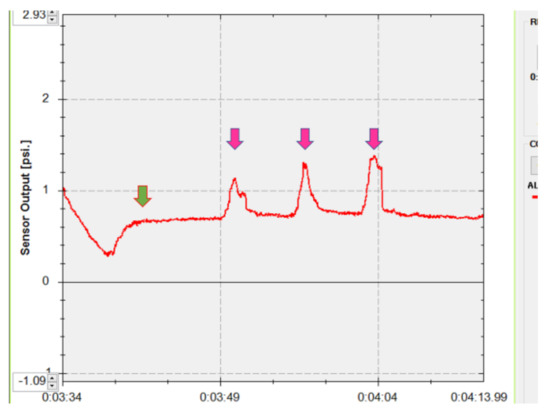
Beyond standard ophthalmological assessment, recent advances in technology have enabled the high-resolution, accurate, and repeatable evaluation of different ocular tissues. For instance, the extensive application of spectral domain optical coherence tomography in ophthalmological practice has greatly widened our knowledge in the study of both the anterior and posterior segments of the eye.
Furthermore, OCT angiography is being successfully applied in the study of vascular alterations of the retina and optic nerve in different systemic diseases potentially involving the eye.
In addition to ophthalmologists, researchers and scientists from other disciplines whose research focuses on this topic are invited to submit original articles or reviews.
Dr. Massimo Cesareo
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Eye
- Systemic diseases
- Retina
- Optical coherence tomography (OCT)
- Angiography (OCTA)