State-of-the-Art Molecular Mechanisms and Pathophysiology of Head and Neck Diseases in Australia
(Closed)
Share This Topical Collection
Editor
Topical Collection Information
Dear Colleagues,
This Topical Collection of International Journal of Molecular Sciences showcases original research and review articles written by researchers involved in the study of head and neck diseases in Australia. Topics covered in this Topical Collection will range from life-threatening conditions such as cancer and immune-mediated diseases to less severe but extremely prevalent and potentially debilitating pathologies such as dental caries and periodontal disease. Questions of fundamental importance pertaining to craniofacial morphogenesis, as well as how alterations of this process disrupt normal development and lead to craniofacial diseases, are also welcome.
With one third of its universities being in the world’s top 200 (QS 2022), Australia is at the forefront of higher education and research. The field of dental and head and neck research makes no exception: in the last few years, researchers down under have elucidated novel pathophysiological mechanisms that have informed the development of innovative diagnostic tools and targeted preventive and/or therapeutic strategies for head and neck diseases.
Hence, the aim of this Topical Collection is to advance biomedical research in head and neck medicine by showcasing Australia’s recent and most significant discoveries in basic and translational research that will become the life-changing breakthroughs of tomorrow.
Potential topics include, but are not limited to:
- head and neck cancer
- oral mucosal diseases
- periodontal disease
- dental caries
- oral/dental anatomy and histology
- craniofacial morphogenesis
- tissue engineering
Prof. Dr. Nicola Cirillo
Collection Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. International Journal of Molecular Sciences is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript.
There is an Article Processing Charge (APC) for publication in this
open access journal. For details about the APC please see here.
Submitted papers should be well formatted and use good English. Authors may use MDPI's
English editing service prior to publication or during author revisions.
Keywords
- wound healing
- oral carcinogenesis
- enamel demineralization
- oral immunology
- host-pathogen interactions
Published Papers (2 papers)
Open AccessArticle
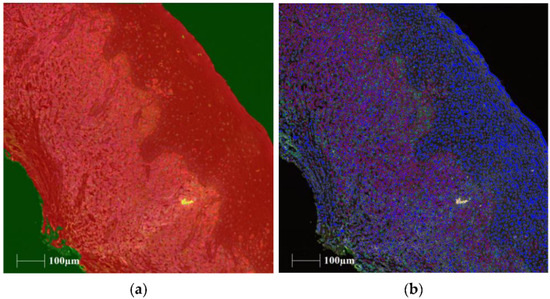
Characterization of Mucosal-Associated Invariant T Cells in Oral Lichen Planus
by
Lara Marie DeAngelis, Nicola Cirillo, Alexis Perez-Gonzalez and Michael McCullough
Cited by 1 | Viewed by 1352
Abstract
Oral lichen planus (OLP) is an inflammatory condition of unknown cause that has been associated with concurrent candidal infection. Mucosal-associated invariant T (MAIT) cells express the T cell receptor TCRVα7.2 and are activated by riboflavin intermediates produced by microbes. The interaction between MAIT
[...] Read more.
Oral lichen planus (OLP) is an inflammatory condition of unknown cause that has been associated with concurrent candidal infection. Mucosal-associated invariant T (MAIT) cells express the T cell receptor TCRVα7.2 and are activated by riboflavin intermediates produced by microbes. The interaction between MAIT cells,
Candida, and OLP is unknown. This study aimed to determine mucosal-associated T cell presence in OLP and whether the abundance of these cells changed due to the presence of either
Candida or symptoms, using multiplex immunohistochemistry (mIHC). Ninety formalin fixed-paraffin-embedded (FFPE) tissue samples were assessed using mIHC for the cellular markers CD3, interleukin 18 receptor one (IL18R1), TCRVα7.2, CD161, CD8, and major histocompatibility complex class I-related (MR-1) protein. The samples were stratified into five groups on the basis of clinical (presence/absence of symptoms) and microbiological (presence/absence of
Candida) criteria. Results demonstrated the presence of MAIT cell phenotypes in OLP inflammatory infiltrate within the connective tissue. Significant differences existed between different OLP groups with the percentage of log(CD3
+ CD161
+) and log(CD3
+ TCRVα7.2
+) positive cells (
p < 0.001 and
p = 0.005 respectively). Significant differences also existed with the relative abundance of triple-stained log(CD3
+ CD161
+ IL18R1
+) cells (
p = 0.004). A reduction in log(CD3
+ CD161
+ IL18R1
+) cells was observed in lesional tissue of patients with symptomatic OLP with and without
Candida when compared to controls. When present in OLP, MAIT cells were identified within the connective tissue. This study demonstrates that mIHC can be used to identify MAIT cell phenotypes in OLP. Reduced percentage of log(CD3
+ CD161
+ IL18R1
+) cells seen in symptomatic OLP with and without
Candida suggests a role for these cells in OLP pathogenesis.
Full article
►▼
Show Figures
Open AccessReview
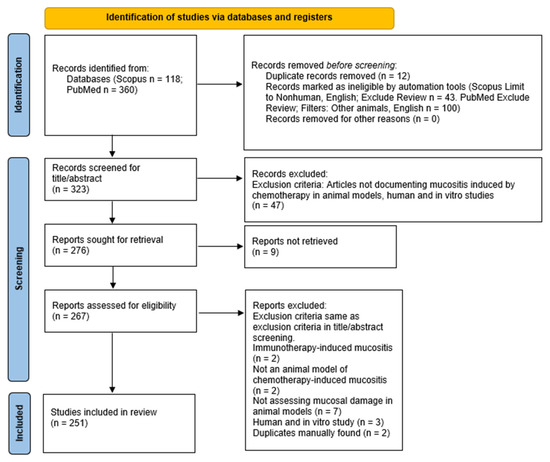
Experimental Chemotherapy-Induced Mucositis: A Scoping Review Guiding the Design of Suitable Preclinical Models
by
Junhua Huang, Alan Yaw Min Hwang, Yuting Jia, Brian Kim, Melania Iskandar, Ali Ibrahim Mohammed and Nicola Cirillo
Cited by 10 | Viewed by 3433
Abstract
Mucositis is a common and most debilitating complication associated with the cytotoxicity of chemotherapy. The condition affects the entire alimentary canal from the mouth to the anus and has a significant clinical and economic impact. Although oral and intestinal mucositis can occur concurrently
[...] Read more.
Mucositis is a common and most debilitating complication associated with the cytotoxicity of chemotherapy. The condition affects the entire alimentary canal from the mouth to the anus and has a significant clinical and economic impact. Although oral and intestinal mucositis can occur concurrently in the same individual, these conditions are often studied independently using organ-specific models that do not mimic human disease. Hence, the purpose of this scoping review was to provide a comprehensive yet systematic overview of the animal models that are utilised in the study of chemotherapy-induced mucositis. A search of PubMed/MEDLINE and Scopus databases was conducted to identify all relevant studies. Multiple phases of filtering were conducted, including deduplication, title/abstract screening, full-text screening, and data extraction. Studies were reported according to the updated Preferred Reporting Items for Systematic reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines. An inter-rater reliability test was conducted using Cohen’s Kappa score. After title, abstract, and full-text screening, 251 articles met the inclusion criteria. Seven articles investigated both chemotherapy-induced intestinal and oral mucositis, 198 articles investigated chemotherapy-induced intestinal mucositis, and 46 studies investigated chemotherapy-induced oral mucositis. Among a total of 205 articles on chemotherapy-induced intestinal mucositis, 103 utilised 5-fluorouracil, 34 irinotecan, 16 platinum-based drugs, 33 methotrexate, and 32 other chemotherapeutic agents. Thirteen articles reported the use of a combination of 5-fluorouracil, irinotecan, platinum-based drugs, or methotrexate to induce intestinal mucositis. Among a total of 53 articles on chemotherapy-induced oral mucositis, 50 utilised 5-fluorouracil, 2 irinotecan, 2 methotrexate, 1 topotecan and 1 with other chemotherapeutic drugs. Three articles used a combination of these drugs to induce oral mucositis. Various animal models such as mice, rats, hamsters, piglets, rabbits, and zebrafish were used. The chemotherapeutic agents were introduced at various dosages via three routes of administration. Animals were mainly mice and rats. Unlike intestinal mucositis, most oral mucositis models combined mechanical or chemical irritation with chemotherapy. In conclusion, this extensive assessment of the literature revealed that there was a large variation among studies that reproduce oral and intestinal mucositis in animals. To assist with the design of a suitable preclinical model of chemotherapy-induced alimentary tract mucositis, animal types, routes of administration, dosages, and types of drugs were reported in this study. Further research is required to define an optimal protocol that improves the translatability of findings to humans.
Full article
►▼
Show Figures