Novel Biomarkers for Alzheimer’s Disease and Other Neurodegenerative Diseases
A topical collection in Cells (ISSN 2073-4409). This collection belongs to the section "Cellular Pathology".
Viewed by 55180Editors
Interests: exosomes; extracellular vesicles; biomarkers; Tau; insulin resistance; complement
Interests: exosomes; extracellular vesicles; biomarkers; Tau; insulin resistance; complement
Topical Collection Information
Dear Colleagues,
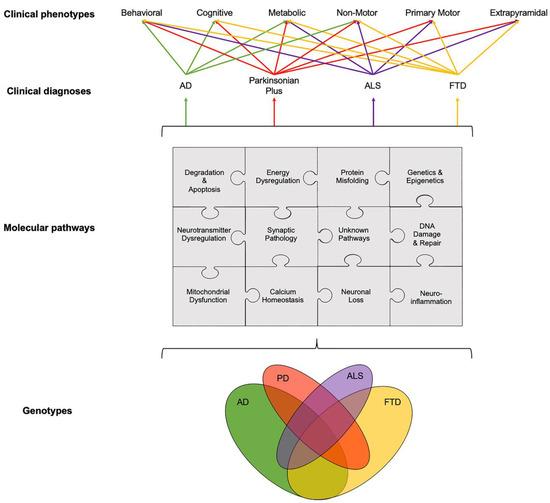
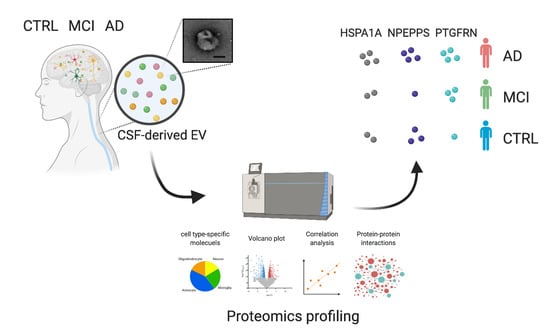
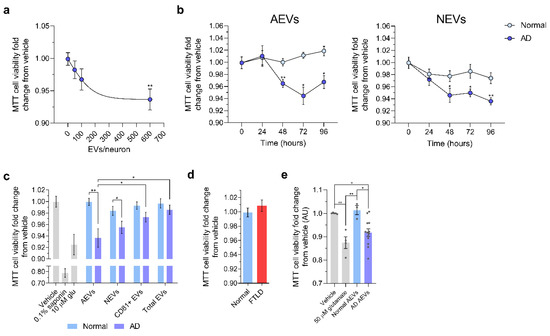
The importance of biomarkers for clinical and preclinical diagnosis of Alzheimer’s disease and other neurodegenerative disorders is increasingly being recognized as an essential aspect of the worldwide effort to improve clinical outcomes and as a stepstone for therapeutic discovery. Traditional cerebrospinal fluid, peripheral blood, and neuroimaging biomarkers have made valuable contributions to our understanding of the evolution of these diseases but may have reached a plateau of potential impact. Novel approaches to biomarker discovery and validation are required for further progress to be made. This Topical Collection aims to showcase novel candidate biomarkers and innovative approaches to biomarker discovery, with an emphasis on scientific rigor and reproducibility. Extracellular vesicle-based biomarkers and multi-omic approaches will be featured as particularly promising examples, but methodological challenges will be readily acknowledged and addressed.
Dr. Dimitrios Kapogiannis
Dr. Erden Eren
Collection Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Alzheimer’s Disease
- neurodegenerative diseases
- biomarkers
- neuroinflammation
- Tau
- exosomes
- extracellular vesicles