Journal Description
Allergies
Allergies
is an international, peer-reviewed, open access journal on allergy and immunology published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 28.1 days after submission; acceptance to publication is undertaken in 7.9 days (median values for papers published in this journal in the second half of 2023).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Latest Articles
The Indirect Costs of Avoidance in Food Allergy Management: A Scoping Review
Allergies 2024, 4(2), 42-53; https://doi.org/10.3390/allergies4020004 - 08 Apr 2024
Abstract
►
Show Figures
Background: Food allergy management requires avoidance of allergenic food. While the direct costs of food allergy management have been described, avoidance may also contribute to time and opportunity costs. We aimed to conduct a scoping review of the peer-reviewed literature on the indirect
[...] Read more.
Background: Food allergy management requires avoidance of allergenic food. While the direct costs of food allergy management have been described, avoidance may also contribute to time and opportunity costs. We aimed to conduct a scoping review of the peer-reviewed literature on the indirect costs of food allergy, and to characterise these costs through a series of fictitious case studies. Methods: We performed a scoping review, guided by Arskey and O’Malley’s methodological framework, and reported using the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews. Eligible studies included original, peer-reviewed, English language literature with no lower limits to publication dates, which addressed the indirect costs of food allergy, including time and opportunity costs. A search strategy was developed by content experts with experience performing multi-database scoping reviews. The search was performed on 10 July 2023, managed using Rayyan (Cambridge, USA), and screened for eligibility. Results: Searches yielded 104 articles. After deduplication, 96 articles were screened at the title and abstract level; 12 articles were included following full-text screening. Of these, three studies were performed on adults with food allergy, eight studies were based on data collected from caregivers of children with food allergy, and one study made use of data reflecting adults and caregivers of children with food allergy. Collectively, indirect costs were identified as higher amongst those with vs. without food allergy. The few studies on age and food allergy differences (e.g., type and number of food allergies, history of reaction) are equivocal. Conclusions: The limited body of peer-reviewed literature supports that food allergy commonly carries substantial indirect costs across diverse measurement tools, albeit with age-group differences.
Full article
Open AccessArticle
Impact of a Pharmacist-Driven Penicillin Allergy De-Labeling Pilot Program in Preoperative Cardiothoracic and Spine Surgery Patients at a Quaternary Hospital
by
Hannah Crum, Brandon Gagnon, Alexis Thumann, Abbey Sidebottom, Marc Vacquier and Krista Gens
Allergies 2024, 4(2), 30-41; https://doi.org/10.3390/allergies4020003 - 26 Mar 2024
Abstract
Documented penicillin allergies are associated with an increased risk of surgical site infections (SSIs), and first-line antibiotics (e.g., cefazolin) are associated with a lower risk of SSIs. The goal of this study was to evaluate the effect of a pharmacist-driven penicillin allergy de-labeling
[...] Read more.
Documented penicillin allergies are associated with an increased risk of surgical site infections (SSIs), and first-line antibiotics (e.g., cefazolin) are associated with a lower risk of SSIs. The goal of this study was to evaluate the effect of a pharmacist-driven penicillin allergy de-labeling pilot program on the use of preoperative cefazolin in selected surgery patients with documented penicillin allergies. This single-center, quasi-experimental study included adult patients with a charted penicillin allergy who underwent CT or spine surgery in 2021 (control group) or during the 6-month intervention pilot (October 2022–March 2023). In the intervention group, qualifying patients were interviewed via phone to assess allergy history. Qualified patients were de-labeled or referred to an allergist for outpatient skin testing and/or oral challenge. The primary outcome was the rate of cefazolin use preoperatively. Secondary outcomes included 30-day SSIs, Clostridioides difficile infection, acute kidney injury, readmission, and hospital length of stay. Of the intervention group, 57 (79.2%) patients completed the interview. Cefazolin was used preoperatively in 71.0% (152) of the control group versus 88.9% (64) of the intervention group (p < 0.002). There were no clinically significant differences in secondary outcomes. The pharmacist-driven penicillin allergy de-labeling pilot program in CT and spine surgery patients was associated with increased cefazolin use.
Full article
(This article belongs to the Section Drug Allergy)
►▼
Show Figures
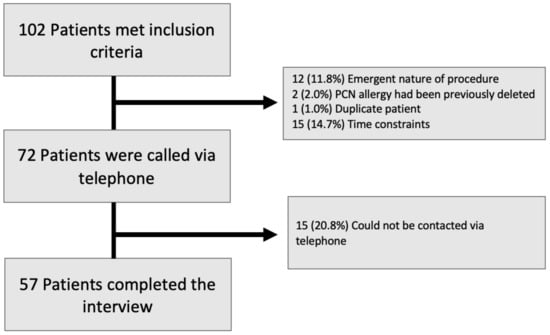
Figure 1
Open AccessReview
Mechanisms and Comparative Treatments of Allergic Rhinitis including Phototherapy
by
Roy Kennedy
Allergies 2024, 4(1), 17-29; https://doi.org/10.3390/allergies4010002 - 16 Feb 2024
Abstract
The treatment of allergic conditions presents a challenge for both seasonal allergic rhinitis and perennial rhinitis sufferers. The increasing prevalence of both of these types of allergic responses requires the use of a range of treatments which can provide relief. The treatment of
[...] Read more.
The treatment of allergic conditions presents a challenge for both seasonal allergic rhinitis and perennial rhinitis sufferers. The increasing prevalence of both of these types of allergic responses requires the use of a range of treatments which can provide relief. The treatment of allergic rhinitis has been considered under the ARIA (Allergic Rhinitis and its Impact on Asthma) guidelines. Current treatment options include medication and avoidance for those with reduced responses, but more expensive treatments include immunotherapy and the use of monoclonal antibodies (mAb). All treatments target specific parts of the inflammatory response which includes mast cells, eosinophils and basophils. Phototherapy can be a useful addition to these treatments, and combinations of UV-B (5%), UV-A (25%) and visible light (70%) in phototherapy treatments have been shown to reduce the severity of symptoms. Phototherapy consisting of visible wavelengths and infrared light (660 nm 940 nm) was shown to be particularly effective in treating perennial rhinitis. The use of a range of wavelengths in the control of allergic responses is described in this paper. Phototherapy can form part of an effective treatment regime for allergic rhinitis sufferers which can exploit synergies in the control of the condition elicited through several pathways.
Full article
(This article belongs to the Special Issue Feature Papers 2023)
►▼
Show Figures
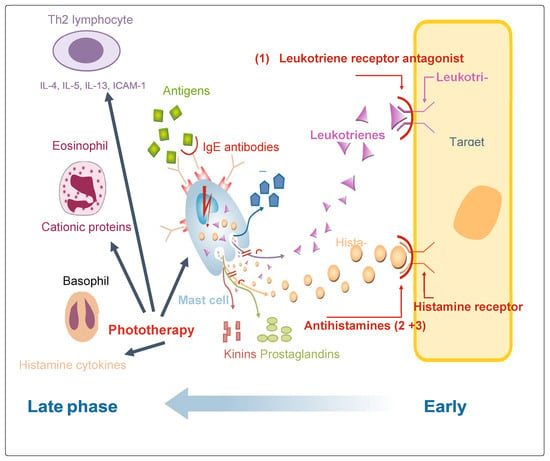
Figure 1
Open AccessReview
Allergenicity and Conformational Diversity of Allergens
by
Clarissa A. Seidler, Ricarda Zeindl, Monica L. Fernández-Quintero, Martin Tollinger and Klaus R. Liedl
Allergies 2024, 4(1), 1-16; https://doi.org/10.3390/allergies4010001 - 11 Jan 2024
Abstract
Allergens are substances that cause abnormal immune responses and can originate from various sources. IgE-mediated allergies are one of the most common and severe types of allergies, affecting more than 20% of the population in Western countries. Allergens can be subdivided into a
[...] Read more.
Allergens are substances that cause abnormal immune responses and can originate from various sources. IgE-mediated allergies are one of the most common and severe types of allergies, affecting more than 20% of the population in Western countries. Allergens can be subdivided into a limited number of families based on their structure, but this does not necessarily indicate the origin or the route of administration of the allergen, nor is the molecular basis of allergenicity clearly understood. This review examines how understanding the allergenicity of proteins involves their structural characterization and elucidates the study of conformational diversity by nuclear magnetic resonance spectroscopy. This article also discusses allergen cross-reactivity and the mechanisms by which IgE antibodies recognize and bind to allergens based on their conformational and linear epitopes. In addition, we outline how the pH, the proteolytic susceptibility and the endosomal degradation affect the outcome of allergic reactions, and how this is correlated with conformational changes and secondary structure rearrangement events. We want to emphasize the importance of considering structural diversity and dynamics, proteolytic susceptibility and pH-dependent factors to fully comprehend allergenicity.
Full article
(This article belongs to the Special Issue Feature Papers 2023)
►▼
Show Figures
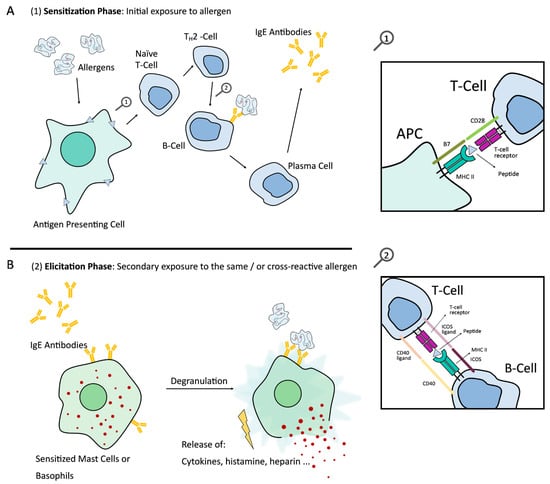
Figure 1
Open AccessReview
Allergic Rhinitis Systematic Review Shows the Trends in Prevalence in Children and Adolescents in Greece since 1990
by
Christos Kogias, Aikaterini Drylli, Demosthenes Panagiotakos, Konstantinos Douros and George Antonogeorgos
Allergies 2023, 3(4), 220-228; https://doi.org/10.3390/allergies3040014 - 06 Nov 2023
Abstract
Allergic rhinitis is the most common immune disorder worldwide, affecting approximately 10–40% of the general population. It is characterized by an inflammatory response of the nasal mucosa following exposure to non-infectious, inhaled, and airborne allergens that are defined based on the period of
[...] Read more.
Allergic rhinitis is the most common immune disorder worldwide, affecting approximately 10–40% of the general population. It is characterized by an inflammatory response of the nasal mucosa following exposure to non-infectious, inhaled, and airborne allergens that are defined based on the period of exposure to the allergen as annual, seasonal, or episodic. A variety of factors are found to relate to the prevalence of allergic rhinitis, i.e., sex, race, age, seasonality, personal and family-positive atopic history, as well as exposure to environmental and epigenetic factors. In addition to the local inflammation in the nasal mucosa, systemic inflammation is activated in the entire respiratory system, such as rhinoconjunctivitis, asthma, sinusitis, and otitis media with effusion. The aim of this study was to evaluate the trends in the prevalence of allergic rhinitis in the Greek pediatric and adolescent population since 1990. Research was performed in electronic databases (PubMed, ScienceDirect, and Cochrane Library) using appropriate MeSH terms for related studies from 1990 to 2023. We found 12 studies, 11 prospective and 1 cross-sectional, conducted in the cities of Athens, Thessaloniki, Patras and Evros prefecture, with sample sizes varying from 517 to 3076 subjects aged 6–17 years old. The prevalence of allergic rhinitis showed geographic and temporal variability, ranging between 2.1 and 32.5% in children and 25.3 and 30.8% in adolescents, with increasing trends. Factors such as gender (male), age (8–10 years), environmental exposures (moisture, mites, and fungi), positive atopic profile, and family history (asthma and eczema) were related to the manifestation of the disease. The need for systematic research in the Greek child and adolescent population is vital to recognize, prognosis, and control allergic rhinitis manifestations.
Full article
(This article belongs to the Section Rhinology/Allergic Rhinitis)
Open AccessArticle
Effect of Eriobotrya japonica Leaf Supplements on Allergic Rhinitis Symptoms and Skin Conditions in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study
by
Masumi Nagae, Maki Nagata, Masako Matsumoto, Naomichi Takemoto, Yhiya Amen, Dongmei Wang, Yuri Yoshimitsu and Kuniyoshi Shimizu
Allergies 2023, 3(4), 202-219; https://doi.org/10.3390/allergies3040013 - 30 Oct 2023
Abstract
►▼
Show Figures
Eriobotrya japonica (E. japonica) leaves have been used as an herbal traditional medicine in China and Japan owing to their anti-inflammatory and protective effects against skin conditions and allergy symptoms. These beneficial effects are likely mediated by the various triterpenoids present
[...] Read more.
Eriobotrya japonica (E. japonica) leaves have been used as an herbal traditional medicine in China and Japan owing to their anti-inflammatory and protective effects against skin conditions and allergy symptoms. These beneficial effects are likely mediated by the various triterpenoids present in E. japonica leaves. However, the efficacy of E. japonica leaves in the treatment of allergic rhinitis has not been evaluated in humans. Therefore, in the present study, a randomized, controlled, double-blind trial was performed on healthy adults of age >20 (n = 27) who were randomly assigned to receive either 2.5 g of placebo or E. japonica leaf supplements once daily for 4 weeks. The Japanese Allergic Rhinitis Quality of Life Standard Questionnaire (JRQLQ), dermatological allergy symptoms, Dermatology Life Quality Index, and skin condition parameters were assessed at baseline and after 4 weeks. Significant differences were observed in the variability of the itchy nose, itchy eyes, and eye symptoms between the E. japonica supplementation and placebo groups after 4 weeks. Arm skin transepidermal water loss was improved only in the E. japonica supplementation group. This study suggests that E. japonica leaves can be used as a functional food ingredient to relieve allergic symptoms.
Full article
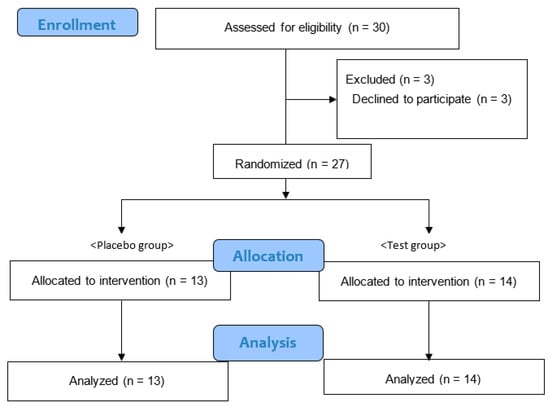
Figure 1
Open AccessArticle
Removal of N-Terminal Peptide Impacts Structural Aspects of an IgE-Reactive Recombinant Der p 5
by
Camilo J. B. Vieira, Raphael C. Silva, Elisânia F. Silveira, Antônio M. S. Fernandes, Dumar A. Jaramillo-Hernández, Luis F. S. Garcés, Larissa M. S. Fonseca, Bruna A. S. Machado, Jamille S. Fernandes, Gabriela P. Pinheiro, Álvaro A. Cruz, Fatima Ferreira, Philip Cooper, Luis G. C. Pacheco, Neuza M. Alcantara-Neves, Carina S. Pinheiro and Eduardo S. da Silva
Allergies 2023, 3(3), 184-201; https://doi.org/10.3390/allergies3030012 - 18 Sep 2023
Abstract
►▼
Show Figures
(1) Background: Modification of the structural elements of allergens is widely used in the field of allergies. The goal of the present research was to express, purify, and characterize the shortened recombinant group 5 allergen of Dermatophagoides pteronyssinus (rDer p 5). (2) Methods:
[...] Read more.
(1) Background: Modification of the structural elements of allergens is widely used in the field of allergies. The goal of the present research was to express, purify, and characterize the shortened recombinant group 5 allergen of Dermatophagoides pteronyssinus (rDer p 5). (2) Methods: rDer p 5 storage stability and aggregation capacity were explored through in silico analysis, dynamic light scattering (DLS), and SDS-PAGE. Serum IgE reactivity and cytokine amount were investigated in sera or cell culture supernatants through ELISA, MULTIPLEX®, and Western blot analysis using sera from sensitized humans from Brazil, Colombia, and Ecuador. (3) Results: Dimeric rDer p 5 was detected through native PAGE, and this result was confirmed by data from DLS. The protein was thermically stable, as it did not degrade at 4 °C for 21 days. The shortened rDer p 5 was classified as a major IgE allergen in Brazil and Colombia, but minor in Ecuador. IL-13, IL-10, IL-1β, and IL-6 were significantly elevated in the sera of rDer p 5-reactive patients. The same cytokines plus IL-5 were more secreted by human cells upon rDer p 5 stimulation. (4) Conclusions: N-terminal peptide deletion led to a higher rDer p 5 folding stability, which, even though dimeric, was an IgE-reactive protein. Therefore, rDer p 5 could be used for molecular diagnostic applications or as backbone for hypoallergen design.
Full article
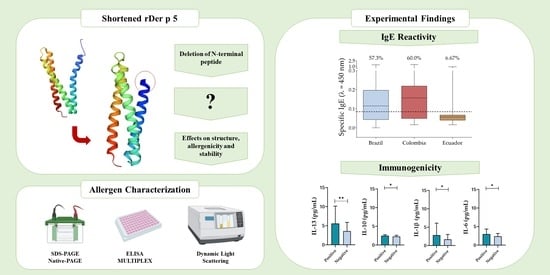
Graphical abstract
Open AccessArticle
The Role of Peamaclein (Pru p 7) in PFAS Patients: An Italian Real-Life Study
by
Marco Spalletti, Valentina Lasala, Paolo Cameli, Laura Bergantini, Marco Saletti, Valerio Beltrami, Elena Bargagli and Miriana d’Alessandro
Allergies 2023, 3(3), 177-183; https://doi.org/10.3390/allergies3030011 - 10 Aug 2023
Abstract
Pollen food allergy syndrome (PFAS) is an allergic reaction to specific foods in persons previously sensitised to pollen. The diagnosis of PFAS is made after taking a patient’s medical history and, in some cases, conducting skin tests and oral food tests with raw
[...] Read more.
Pollen food allergy syndrome (PFAS) is an allergic reaction to specific foods in persons previously sensitised to pollen. The diagnosis of PFAS is made after taking a patient’s medical history and, in some cases, conducting skin tests and oral food tests with raw fruit or vegetables. The aim of the present study was to evaluate the role of Pru p 7 in patients suspected of having PFAS, who show clinical symptoms, positivity for Cup a 1 and negativity for Pru p 1 and Pru p 3. A total of 51 patients (mean age ± standard deviation, 33 ± 15 years; 20 men and 31 women), referred to the respiratory diseases and allergology units of Siena University Hospital, were enrolled retrospectively. All of them underwent allergy consultation and IgE evaluation for Cup a 1, Pru p 1 and Pru p 3 by immuno solid-phase allergen chip (ISAC). Pru p 7 assay was performed by the ImmunoCAP Phadia method in patients who tested positive for Cup a 1 and simultaneously negative for Pru p 1 and Pru p 3 by ISAC. The serum of 51 patients was tested for sensitisation to Pru p 7 by the ImmunoCAP Phadia method, and nine patients (17.65%) were found positive. An area under the receiver operating characteristic (AUROC) curve of 99.51% made it possible to distinguish PFAS and non-PFAS patients on the basis of Pru p 7 values. The best cut-off value was 0.16 kUA/l, which gave a 85.7% sensitivity and 97.73% specificity. This study helps define the role of Pru p 7 in PFAS patients sensitised to cypress pollen and testing negative to Pru p 1 and Pru p 3. A fast, easy and non-invasive diagnostic method is proposed to detect IgE specific for Pru p 7. Inclusion of Pru p 7 in the ISAC assay panel would facilitate the diagnosis of PFAS.
Full article
(This article belongs to the Special Issue Feature Papers 2023)
►▼
Show Figures
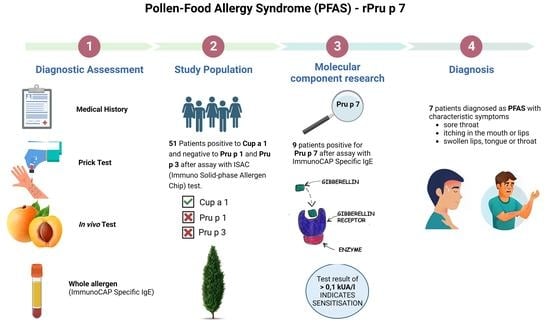
Graphical abstract
Open AccessReview
An Overview of Fruit Allergens: Structural, Functional, Phylogenetical, and Clinical Aspects
by
Annick Barre, Hervé Benoist and Pierre Rougé
Allergies 2023, 3(3), 134-176; https://doi.org/10.3390/allergies3030010 - 13 Jul 2023
Cited by 1
Abstract
Most of the allergenic proteins from fruits identified so far belong to different families of pathogenesis-related (PR) proteins. These PR proteins have been classified in different families of structurally and functionally unrelated proteins, but the majority of all fruit allergens belong to three
[...] Read more.
Most of the allergenic proteins from fruits identified so far belong to different families of pathogenesis-related (PR) proteins. These PR proteins have been classified in different families of structurally and functionally unrelated proteins, but the majority of all fruit allergens belong to three groups, in particular PR-5 thaumatin-like proteins (TLP), PR-10 Bet v 1-like proteins, and PR-14 non-specific lipid transfer proteins (nsTLP). Some allergenic proteins from fruits can also be found among PR-protein families of PR-2 β1,3-glucanase proteins, PR-3 chitinases I, II, IV–VII, and PR-8 chitinases III. In addition, other important fruit allergens occur in protein families unrelated to the PR-protein families, such as the profilins and the newly emerging group of gibberellin-regulated proteins (GBRP). Finally, proteins that belong to seed storage proteins from higher plants, including 2S albumins, 7S globulins (vicilin), and 11S globulins (legumin), must be retained as possible potential fruit allergens resulting from the unintended consumption of the seeds. Here, we present an overview of the structural organization, functional properties, and phylogenetical relationships among these different groups of fruit allergens, supporting the occurrence of cross-reactivity and cross-allergenicity often described between fruit allergens, and the corresponding allergens from vegetables and pollens.
Full article
(This article belongs to the Section Food Allergy)
►▼
Show Figures

Figure 1
Open AccessReview
Genetic and Epigenetic Factors in Risk and Susceptibility for Childhood Asthma
by
Dimitrina Miteva, Snezhina Lazova and Tsvetelina Velikova
Allergies 2023, 3(2), 115-133; https://doi.org/10.3390/allergies3020009 - 14 Jun 2023
Abstract
Asthma is a common respiratory disease that affects people of all ages, characterized by considerable heterogeneity in age, clinical presentation, genetics, epigenetics, environmental factors, treatment response, and prognostic outcomes. Asthma affects more than 330 million people worldwide, of which 33% are children under
[...] Read more.
Asthma is a common respiratory disease that affects people of all ages, characterized by considerable heterogeneity in age, clinical presentation, genetics, epigenetics, environmental factors, treatment response, and prognostic outcomes. Asthma affects more than 330 million people worldwide, of which 33% are children under 14 years, and 27% are adults whose first symptoms occurred in childhood. However, the genetic and epigenetic mechanisms of childhood allergic diseases and asthma are still not fully understood. Here, we conducted a biomedical narrative review of genes associated with the risk, severity, and susceptibility of childhood asthma since it differs from asthma in adults regarding their pathophysiology, development, and outcomes. We also systematized the available information on epigenetic changes associated with childhood asthma.
Full article
(This article belongs to the Section Asthma/Respiratory)
►▼
Show Figures
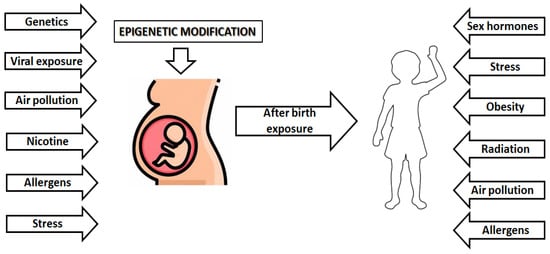
Figure 1
Open AccessArticle
Is Switching of Adrenaline Auto Injector Devices a Concern for Anaphylaxis Management? A CROSS-Sectional Study
by
Caoimhe Cronin, Ciobha O’Kelly, Hannah Keohane, Laura Flores Villarta, Ciara Tobin, Roberto Velasco and Juan Trujillo Wurttele
Allergies 2023, 3(2), 105-114; https://doi.org/10.3390/allergies3020008 - 12 May 2023
Cited by 1
Abstract
Adrenaline auto injectors (AAI) are the mainstay of treatment in anaphylaxis. However, many caregivers of children with food allergies are unable to administer an AAI when assessed. One proposed factor for this finding is the lack of training and familiarity of the different
[...] Read more.
Adrenaline auto injectors (AAI) are the mainstay of treatment in anaphylaxis. However, many caregivers of children with food allergies are unable to administer an AAI when assessed. One proposed factor for this finding is the lack of training and familiarity of the different AAI devices. The aim of this study is to explore the usage of different brands of adrenaline auto-injectors among caregivers of children with food allergies in Ireland. A cross-sectional study method was employed using an online questionnaire. An amount of 121 (75.58%) caregivers reported that their child carried an Epipen®, 25 (15.82%) carried Jext®, and 12 (7.59%) carried Anapen®. An amount of 48.73% (n = 77) of caregivers had switched brands of AAI at least once before, with lack of availability of their usual device at their pharmacy being the most common reason for this. Factors associated with change were a household income >100,000 € (70% vs. 44.9% of those with less income; p = 0.04) and parents ≥40 years old (59.6% vs. 32.8% of patients whose parents younger; p < 0.01). When asked what they preferred about a particular AAI brand, caregivers appreciated a simple design with minimal steps involved in administration, clear colour coding, online resources, formal training from a healthcare professional, and first-hand experience in using the AAI. These findings show, for the first time, that switching brands is a common occurrence among caregivers of children with food allergies. These findings support the EAACI recommendation to train parents regularly in all available brands of AAI and to retrain parents when switching to different devices.
Full article
(This article belongs to the Special Issue Feature Papers 2023)
►▼
Show Figures
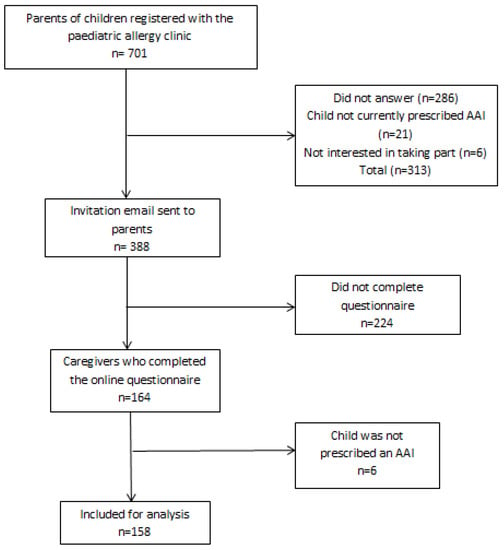
Figure 1
Open AccessReview
Targeting IgE and Th2-Cytokines in Allergy: Brief Updates on Monoclonal Antibodies and Antibody Gene Therapy
by
Henry C. Ezechukwu, Oyelola A. Adegboye, Wahab O. Okunowo and Theophilus I. Emeto
Allergies 2023, 3(2), 90-104; https://doi.org/10.3390/allergies3020007 - 03 Apr 2023
Cited by 1
Abstract
The search for an effective treatment of allergic conditions is an ongoing global health challenge due to the high prevalence of allergies. Epinephrine and glucocorticosteroids remain the oldest and most widely used treatment regimen for allergy, and these medications are for short relief.
[...] Read more.
The search for an effective treatment of allergic conditions is an ongoing global health challenge due to the high prevalence of allergies. Epinephrine and glucocorticosteroids remain the oldest and most widely used treatment regimen for allergy, and these medications are for short relief. In extreme allergy manifestations, the current treatment options aim to use monoclonal antibody (mAb) to target pathological pathways of inflammation involving mast cells, eosinophils, and basophils. These cells have the propensity to induce an allergic-inflammatory response. Studies have shown that they are responsible for several allergic diseases, such as allergic asthma, atopic dermatitis, rhinitis, and conjunctivitis. Studies evaluating monoclonal antibodies against serum IgE (Omalizumab), Th-2 cytokines, such as IL-4, IL-13 (dupilumab), and IL-5 suggest an attenuation of allergic symptoms and improvement in patients’ overall well-being. However, several factors such as cost of production (i.e., antibody purification), host immunogenicity, safety, and efficacy have hindered the availability of purified mAb in developing countries. Gene therapy is a promising tool for treating allergy, and emerging studies have suggested that antibody gene therapy may be the future for treating extreme cases of allergy manifestations. This paper describes the use of purified monoclonal antibodies for treating severe allergic responses and the associated limitations. It explores the prospects of antibody gene therapy for modulating allergy episodes.
Full article
(This article belongs to the Section Physiopathology)
►▼
Show Figures
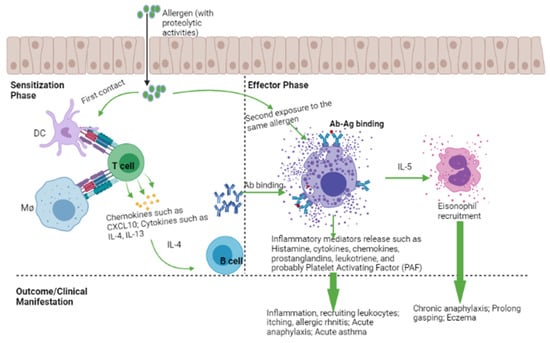
Figure 1
Open AccessReview
Efficacy and Safety of Oral Probiotics in Children with Allergic Rhinitis: A Review
by
Angela Klain, Giulio Dinardo, Cristiana Indolfi, Marcella Contieri, Alessandra Salvatori, Sossio Vitale, Fabio Decimo, Giorgio Ciprandi and Michele Miraglia del Giudice
Allergies 2023, 3(1), 72-89; https://doi.org/10.3390/allergies3010006 - 07 Mar 2023
Abstract
The prevalence of allergic rhinitis is rising, and it is impacting children’s growth and quality of life. To uncover unconventional treatment modalities, research was carried out to clarify the significance of novel components in the pathophysiology of allergic rhinitis. One of these elements
[...] Read more.
The prevalence of allergic rhinitis is rising, and it is impacting children’s growth and quality of life. To uncover unconventional treatment modalities, research was carried out to clarify the significance of novel components in the pathophysiology of allergic rhinitis. One of these elements was gut microbiota, which plays a crucial role in the development and evolution of allergic disorders. Specifically, dysbiosis, defined as impaired microbiota composition, characterizes allergic disorders. In light of this concept, probiotics (beneficial bacteria) may restore gut dysbiosis, rebalance the immune response, and indirectly influence the clinical course of allergic diseases. In this article, we discussed the role of the gut–lung axis in children and reported on new findings. We also reviewed the most relevant studies about probiotics in patients with allergic rhinitis.
Full article
(This article belongs to the Special Issue Probiotics in Allergy, Asthma and Respiratory Infections)
►▼
Show Figures
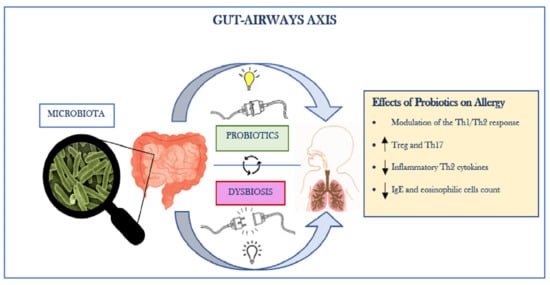
Figure 1
Open AccessArticle
Multiplex Specific IgE Profiling in Neonatal Stool of Preterms Predicts IgE-Mediated Disease
by
Youssouf Sereme, Moïse Michel, Soraya Mezouar, Nicolas Orain, Renaud Cezar, Tran Tu Anh, Pierre Corbeau, Anne Filleron and Joana Vitte
Allergies 2023, 3(1), 58-71; https://doi.org/10.3390/allergies3010005 - 26 Feb 2023
Abstract
►▼
Show Figures
Background: The natural history of immunoglobulin (Ig) E-mediated diseases in preterm infants is still elusive. We aimed at developing a non-invasive tool for detecting specific IgE (sIgE) and eosinophil-derived neurotoxin (EDN) in neonatal fecal samples and evaluating its predictive value for the development
[...] Read more.
Background: The natural history of immunoglobulin (Ig) E-mediated diseases in preterm infants is still elusive. We aimed at developing a non-invasive tool for detecting specific IgE (sIgE) and eosinophil-derived neurotoxin (EDN) in neonatal fecal samples and evaluating its predictive value for the development of IgE-mediated diseases during the first year of life. Methods: We developed a stool extraction protocol, followed by freeze-drying and solubilization. The sIgEs were investigated in neonatal fecal samples from 21 preterm infants with a 300-allergen multiplex and confirmed by a capillary Western blot with a nano-immunoassay. EDN concentration was used to investigate the local eosinophilic component. Results: The multiplexed allergen assay detected sIgE in all of the samples. A Western blot was used to confirm the results. The frequency and levels of sIgE in the neonatal fecal samples differed between the infants who developed IgE-mediated diseases and the controls. Allergen specificity was associated with the development of cow’s milk allergy (CMA) and asthma. The development of CMA was predicted by the sIgE response to milk proteins (sensitivity was 88%; specificity was 78%). The EDN levels predicted the development of IgE-mediated diseases (sensitivity was 100%; specificity was 75%). Conclusion: The non-invasive investigation of neonatal fecal sIgE is a promising tool for predicting the subsequent development of IgE-mediated diseases. Clinical Implications: The non-invasive sIgE and EDN profiling of neonatal fecal samples from preterm infants can predict the development of IgE-mediated diseases.
Full article
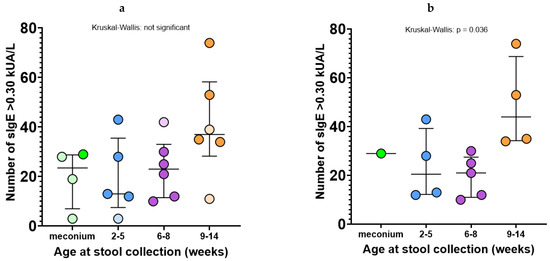
Figure 1
Open AccessArticle
Impacts of Sourdough Technology on the Availability of Celiac Peptides from Wheat α- and γ-Gliadins: In Silico Approach
by
Annick Barre, Hervé Benoist and Pierre Rougé
Allergies 2023, 3(1), 39-57; https://doi.org/10.3390/allergies3010004 - 03 Feb 2023
Cited by 1
Abstract
Celiac peptide-generating α- and γ-gliadins consist of a disordered N-terminal domain extended by an α-helical-folded C-terminal domain. Celiac peptides, primarily located along the disordered part of α- and γ-gliadin molecules, are nicely exposed and directly accessible to proteolytic enzymes occurring in
[...] Read more.
Celiac peptide-generating α- and γ-gliadins consist of a disordered N-terminal domain extended by an α-helical-folded C-terminal domain. Celiac peptides, primarily located along the disordered part of α- and γ-gliadin molecules, are nicely exposed and directly accessible to proteolytic enzymes occurring in the gastric (pepsin) and intestinal (trypsin, chymotrypsin) fluids. More than half of the potential celiac peptides identified so far in gliadins exhibit cleavage sites for pepsin. However, celiac peptides proteolytically truncated by one or two amino acid residues could apparently retain some activity toward HLA-DQ2 and HLA-DQ8 receptors in docking experiments. Together with the uncleaved peptides, these still active partially degraded CD peptides account for the incapacity of the digestion process to inactivate CD peptides from gluten proteins. In contrast, sourdough fermentation processes involve other proteolytic enzymes susceptible to the deep degradation of celiac peptides. In particular, sourdough supplemented by fungal prolyl endoproteases enhances the degrading capacities of the sourdough fermentation process toward celiac peptides. Nevertheless, since tiny amounts of celiac peptides sufficient to trigger deleterious effects on CD people can persist in sourdough-treated bread and food products, it is advisable to avoid consumption of sourdough-treated food products for people suffering from celiac disease. As an alternative, applying the supplemented sourdough process to genetically modified low gluten or celiac-safe wheat lines should result in food products that are safer for susceptible and CD people.
Full article
(This article belongs to the Special Issue Advances in Processing for Food Allergies)
►▼
Show Figures
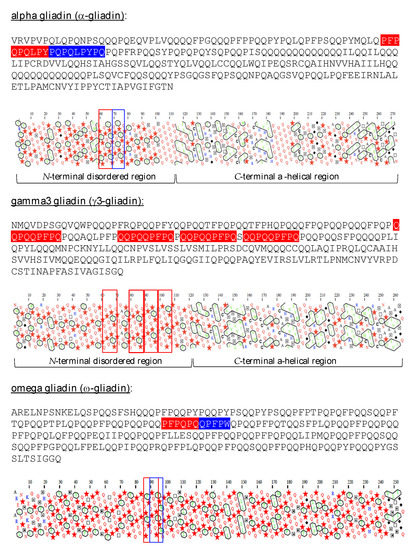
Figure 1
Open AccessSystematic Review
Seed Storage Protein, Functional Diversity and Association with Allergy
by
Abha Jain
Allergies 2023, 3(1), 25-38; https://doi.org/10.3390/allergies3010003 - 18 Jan 2023
Cited by 7
Abstract
Plants are essential for humans as they serve as a source of food, fuel, medicine, oils, and more. The major elements that are utilized for our needs exist in storage organs, such as seeds. These seeds are rich in proteins, show a broad
[...] Read more.
Plants are essential for humans as they serve as a source of food, fuel, medicine, oils, and more. The major elements that are utilized for our needs exist in storage organs, such as seeds. These seeds are rich in proteins, show a broad spectrum of physiological roles, and are classified based on their sequence, structure, and conserved motifs. With the improvements to our knowledge of the basic sequence and our structural understanding, we have acquired better insights into seed proteins and their role. However, we still lack a systematic analysis towards understanding the functional diversity associated within each family and their associations with allergy. This review puts together the information about seed proteins, their classification, and diverse functional roles along with their associations with allergy.
Full article
(This article belongs to the Special Issue Fruit Allergies, New Emerging Allergens)
►▼
Show Figures
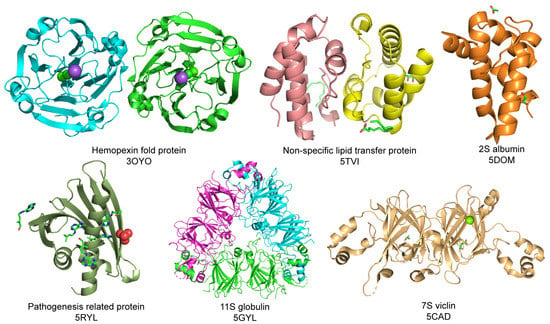
Figure 1
Open AccessArticle
Structural Basis for the IgE-Binding Cross-Reacting Epitopic Peptides of Cup s 3, a PR-5 Thaumatin-like Protein Allergen from Common Cypress (Cupressus sempervirens) Pollen
by
Annick Barre, Hélène Sénéchal, Christophe Nguyen, Claude Granier, Pascal Poncet and Pierre Rougé
Allergies 2023, 3(1), 11-24; https://doi.org/10.3390/allergies3010002 - 10 Jan 2023
Cited by 3
Abstract
The present work was aimed at identifying the IgE-binding epitopic regions on the surface of the Cup s 3 allergen from the common cypress Cupressus sempervirens, that are possibly involved in the IgE-binding cross-reactivity reported between Cupressaceae species. Three main IgE-binding epitopic
[...] Read more.
The present work was aimed at identifying the IgE-binding epitopic regions on the surface of the Cup s 3 allergen from the common cypress Cupressus sempervirens, that are possibly involved in the IgE-binding cross-reactivity reported between Cupressaceae species. Three main IgE-binding epitopic regions were mapped on the molecular surface of Cup s 3, the PR-5 thaumatin-like allergen of common cypress Cupressus sempervirens. They correspond to exposed areas containing either electropositive (R, K) or electronegative (D, E) residues. A coalescence occurs between epitopes #1 and #2, that creates an extended IgE-binding regions on the surface of the allergen. Epitope #3 contains a putative N-glycosylation site which is actually glycosylated and could therefore comprise a glycotope. However, most of the allergenic potency of Cup s 3 depends on non-glycosylated epitopic peptides. The corresponding regions of thaumatin-like allergens from other closely related Cupressaceae (Cryptomeria, Juniperus, Thuja) exhibit a very similar conformation that should account for the IgE-binding cross-reactivity observed among the Cupressaceae allergens.
Full article
(This article belongs to the Section Allergen/Pollen)
►▼
Show Figures
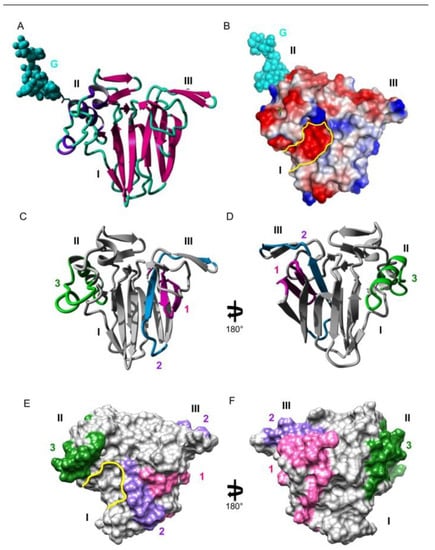
Figure 1
Open AccessArticle
Bacillus subtilis Provides Long-Term Protection in a Murine Model of Allergic Lung Disease by Influencing Bacterial Composition
by
Rosalinda Monroy Del Toro, Ryan Incrocci, Olivia Negris, Shaina McGrath and Julie A. Swartzendruber
Allergies 2023, 3(1), 1-10; https://doi.org/10.3390/allergies3010001 - 23 Dec 2022
Abstract
Probiotics are an attractive target for reducing the incidence of allergic disease. Bacillus subtilis is a gut-associated probiotic bacteria that can suppress allergic lung disease; however, it is not clear for how long this protection lasts. We exposed C57Bl/6 mice to B. subtilis
[...] Read more.
Probiotics are an attractive target for reducing the incidence of allergic disease. Bacillus subtilis is a gut-associated probiotic bacteria that can suppress allergic lung disease; however, it is not clear for how long this protection lasts. We exposed C57Bl/6 mice to B. subtilis via oral gavage and challenged them with intranasal house-dust mite for up to 8 weeks. We found that B. subtilis treatment was able to provide protection from eosinophil infiltration of the airways for 3 weeks. This loss of protection correlated with an increase in the eosinophil chemoattractant CCL24. Additionally, we demonstrate that B. subtilis treatment altered the bacterial composition by increasing the phylum Bacteroidetes and Verrucomicorbiota. The phylum Verrucomicorbiota was reduced in B. subtilis-treated mice at 8 weeks when protection was lost. These results support B. subtilis as a prophylactic for preventing the production of allergic lung disease and highlights that protection can last up to 3 weeks. This work also expands our understanding of how B. subtilis mediates protection and that in addition to modifying the immune system it is also altering the host microbiota.
Full article
(This article belongs to the Section Physiopathology)
►▼
Show Figures
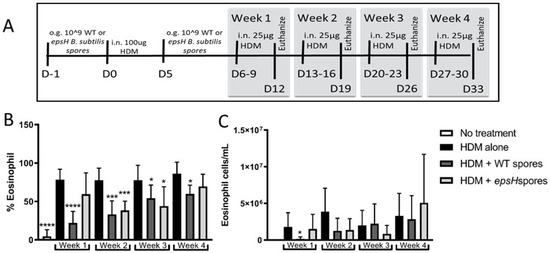
Figure 1
Open AccessArticle
Development of an Allergic Rhinitis Diagnosis Application Using the Total Tear IgE Detection Kit for Examining Nasal Fluid: Comparison and Combination with the Conventional Nasal Smear Examination for Eosinophils
by
Hiroshi Kumanomidou and Mitsuhiro Okano
Allergies 2022, 2(4), 146-153; https://doi.org/10.3390/allergies2040014 - 09 Dec 2022
Abstract
►▼
Show Figures
Allergic rhinitis (AR) is a type I allergic disease characterized by immunoglobulin E (IgE) -mediated hypersensitivity of the nasal mucosa. Here, we focused on a commercial test kit named Allerwatch® (AW) for the diagnosis of allergic conjunctivitis (AC) in which total tear
[...] Read more.
Allergic rhinitis (AR) is a type I allergic disease characterized by immunoglobulin E (IgE) -mediated hypersensitivity of the nasal mucosa. Here, we focused on a commercial test kit named Allerwatch® (AW) for the diagnosis of allergic conjunctivitis (AC) in which total tear IgE is qualitatively detected based on immunochromatography. We evaluated the usefulness of the AW test for detecting total IgE in the nasal discharge of AR and non-allergic rhinitis (non-AR) patients in comparison and combination with the conventional nasal smear examination for eosinophils. Using the AW test, total IgE in nasal fluid was detected in 64.76% of the AR patients and 11.11% of the non-AR patients, with a significant difference between the groups (p < 0.001). As compared to non-AR, the sensitivity and specificity of the detection of total IgE in nasal fluid for detecting AR were 64.76% and 88.89%, respectively. In the AR patients, house dust mites (57.1% of patients) and Japanese cedar pollen (93.3% of patients) were the major sensitizing antigens. When we considered a positive result in either of the two examinations to indicate a positive result, the rate of positivity in AR patients increased to 78.10%. As compared to non-AR, the sensitivity and specificity of the combination of both examinations for detecting AR were 78.10% and 83.33%, respectively. The AW test in the nasal cavity and the qualitative measurement of total IgE in nasal fluid may enable the detection of allergic elements in patients who present to a medical institution with nasal symptoms. In addition, the detection rate is increased when combined with the nasal smear examination for eosinophils.
Full article
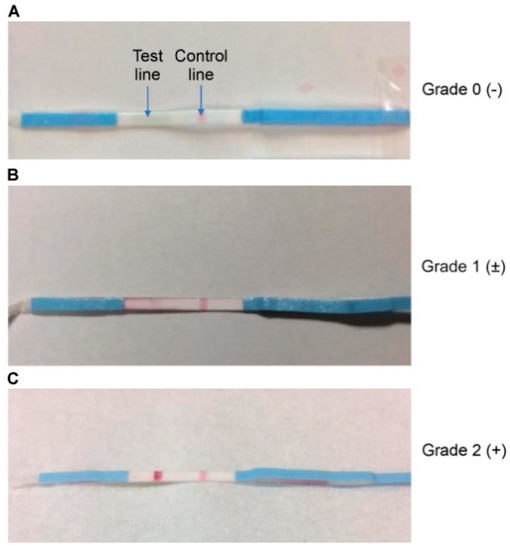
Figure 1
Open AccessReview
A Brief Review of Local Bacteriotherapy for Preventing Respiratory Infections
by
Giorgio Ciprandi, Valerio Damiani, Vittorio Cordara and Maria Angela Tosca
Allergies 2022, 2(4), 138-145; https://doi.org/10.3390/allergies2040013 - 07 Nov 2022
Abstract
Recurrent respiratory infections (RRIs) account for relevant economic and social implications and significantly affect family life. Local Bacteriotherapy (LB) represents an innovative option in preventing RRIs. Local bacteriotherapy consists of administering “good” and safe bacteria (probiotics) by nasal or oral route. In particular,
[...] Read more.
Recurrent respiratory infections (RRIs) account for relevant economic and social implications and significantly affect family life. Local Bacteriotherapy (LB) represents an innovative option in preventing RRIs. Local bacteriotherapy consists of administering “good” and safe bacteria (probiotics) by nasal or oral route. In particular, two strains (Streptococcus salivarius 24SMB and Streptococcus oralis 89a) are commonly used. The present article presents and discusses the literature concerning LB. Infections of airways include the upper and lower respiratory tract. A series of clinical trials investigated the preventive role of LB in preventing upper and lower RIs. These studies demonstrated that LB safely reduced the prevalence and severity of RIs, the use of antibiotics, and absences from school. Therefore, Local Bacteriotherapy may be considered an interesting therapeutic option in RRI prevention.
Full article
(This article belongs to the Special Issue Probiotics in Allergy, Asthma and Respiratory Infections)
►▼
Show Figures
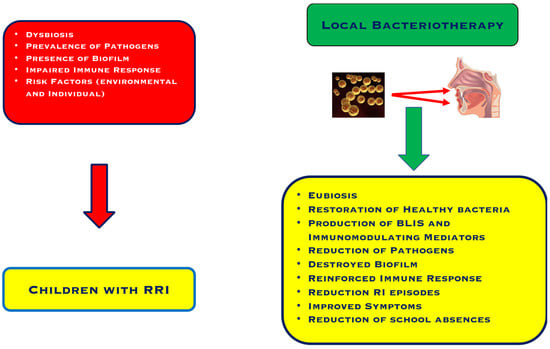
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics

Conferences
Special Issues
Special Issue in
Allergies
Feature Papers 2024
Guest Editors: Pierre Rougé, Carmen CuadradoDeadline: 31 December 2024




