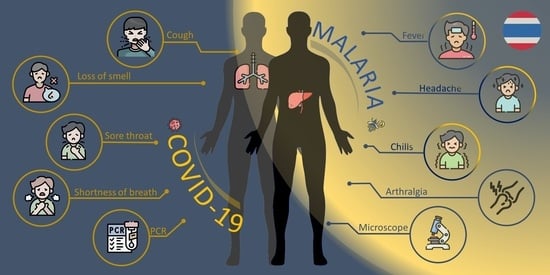
Co-Infection with Plasmodium vivax and COVID-19 in Thailand
Abstract
:1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, L.; Wang, Y.; Ye, D.; Liu, Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int. J. Antimicrob. Agents 2020, 55, 105948. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/table (accessed on 10 February 2022).
- Gutman, J.R.; Lucchi, N.W.; Cantey, P.T.; Steinhardt, L.C.; Samuels, A.M.; Kamb, M.L.; Kapella, B.K.; McElroy, P.D.; Udhayakumar, V.; Lindblade, K.A. Malaria and Parasitic Neglected Tropical Diseases: Potential Syndemics with COVID-19? Am. J. Trop. Med. Hyg. 2020, 103, 572–577. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Malaria Report 2021. Available online: https://www.who.int/publications/i/item/9789240040496 (accessed on 6 December 2021).
- Di Gennaro, F.; Marotta, C.; Locantore, P.; Pizzol, D.; Putoto, G. Malaria and COVID-19: Common and Different Findings. Trop. Med. Infect. Dis. 2020, 5, 141. [Google Scholar] [CrossRef]
- Malaria Online Database, Thailand Malaria Elimination Program. Available online: http://malaria.ddc.moph.go.th/malariar10/index_newversion.php (accessed on 11 May 2022).
- Singh, B.; Ryan, H.; Kredo, T.; Chaplin, M.; Fletcher, T. Chloroquine or hydroxychloroquine for prevention and treatment of COVID-19. Cochrane Database Syst. Rev. 2021, 2, CD013587. [Google Scholar] [CrossRef] [PubMed]
- Emergency Operations Center DoDC, Ministry of Public Health Thailand. The Coronavirus Disease 2019 Situation. Available online: https://ddc.moph.go.th/viralpneumonia/eng/file/situation/situation-no695-061264.pdf (accessed on 6 December 2021).
- Wilairatana, P.; Masangkay, F.R.; Kotepui, K.U.; Milanez, G.J.; Kotepui, M. Prevalence and characteristics of malaria among COVID-19 individuals: A systematic review, meta-analysis, and analysis of case reports. PLoS Negl. Trop. Dis. 2021, 15, e0009766. [Google Scholar] [CrossRef] [PubMed]
- Hussein, R.; Guedes, M.; Ibraheim, N.; Ali, M.M.; El-Tahir, A.; Allam, N.; Abuakar, H.; Pecoits-Filho, R.; Kotanko, P. CLINICAL MICROBIOLOGY AND INFECTION. Available online: https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(22)00167-7/fulltext (accessed on 15 July 2022).
- Achan, J.; Serwanga, A.; Wanzira, H.; Kyagulanyi, T.; Nuwa, A.; Magumba, G.; Kusasira, S.; Sewanyana, I.; Tetteh, K.; Drakeley, C.; et al. Current malaria infection, previous malaria exposure, and clinical profiles and outcomes of COVID-19 in a setting of high malaria transmission: An exploratory cohort study in Uganda. Lancet Microbe 2022, 3, e62–e71. [Google Scholar] [CrossRef]
- Mahajan, N.N.; Gajbhiye, R.K.; Bahirat, S.; Lokhande, P.D.; Mathe, A.; Rathi, S.; Warty, N.; Mahajan, K.N.; Srivastava, V.; Kuppusamy, P.; et al. Co-infection of malaria and early clearance of SARS-CoV-2 in healthcare workers. J. Med. Virol. 2021, 93, 2431–2438. [Google Scholar] [CrossRef] [PubMed]
- Kishore, R.; Dhakad, S.; Arif, N.; Dar, L.; Mirdha, B.R.; Aggarwal, R.; Kabra, S.K. COVID-19: Possible Cause of Induction of Relapse of Plasmodium vivax Infection. Indian J. Pediatr. 2020, 87, 751–752. [Google Scholar] [CrossRef]
- Mahajan, N.N.; Kesarwani, S.N.; Shinde, S.S.; Nayak, A.; Modi, D.N.; Mahale, S.D.; Gajbhiye, R.K. Co-infection of malaria and dengue in pregnant women with SARS-CoV-2. Int. J. Gynecol. Obstet. 2020, 151, 459–462. [Google Scholar] [CrossRef]
- Pusparani, A.; Henrina, J.; Cahyadi, A. Co-infection of COVID-19 and recurrent malaria. J. Infect. Dev. Ctries. 2021, 15, 625–629. [Google Scholar] [CrossRef]
- Ray, M.; Vazifdar, A.; Shivaprakash, S. Co-infection with Malaria and Coronavirus Disease-2019. J. Glob. Infect. Dis. 2020, 12, 162–163. [Google Scholar] [CrossRef]
- Sardar, S.; Sharma, R.; Alyamani, T.Y.M.; Aboukamar, M. COVID-19 and Plasmodium vivax malaria co-infection. IDCases 2020, 21, e00879. [Google Scholar] [CrossRef] [PubMed]
- Shahid, Z.; Karim, N.; Shahid, F.; Yousaf, Z. COVID-19 Associated Imported Plasmodium vivax Malaria Relapse: First Reported Case and Literature Review. Res. Rep. Trop. Med. 2021, 12, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Schantz-Dunn, J.; Nour, N.M. Malaria and pregnancy: A global health perspective. Rev. Obstet. Gynecol. 2009, 2, 186–192. [Google Scholar] [PubMed]
- Caglar, B.; Karaali, R.; Balkan, I.I.; Mete, B.; Aygun, G. COVID-19 and Plasmodium ovale Malaria: A Rare Case of Co-Infection. Korean J. Parasitol. 2021, 59, 399–402. [Google Scholar] [CrossRef]
- Chen, M.; Gao, S.; Ai, L.; Chen, J.; Feng, T.; Chen, Z.; Zhang, X.; Deng, S.; Lin, Z.; Tang, Y.; et al. The First Reported Case of COVID-19 and Plasmodium ovale Malaria Coinfection—Guangdong Province, China, January 2021. China CDC Wkly. 2021, 3, 454–455. [Google Scholar] [CrossRef]
- Papaccio, M.; Castellani, R.; Zanardini, C.; Sartori, E.; Prefumo, F.; Saccani, B. Pregnancy and COVID-19: Do not overlook malaria. Int. J. Gynaecol. Obstet. 2021, 153, 550–551. [Google Scholar] [CrossRef]
- Battle, K.E.; Baird, J.K. The global burden of Plasmodium vivax malaria is obscure and insidious. PLoS Med. 2021, 18, e1003799. [Google Scholar] [CrossRef]
- Kunno, J.; Supawattanabodee, B.; Sumanasrethakul, C.; Wiriyasivaj, B.; Kuratong, S.; Kaewchandee, C. Comparison of Different Waves during the COVID-19 Pandemic: Retrospective Descriptive Study in Thailand. Adv. Prev. Med. 2021, 2021, 5807056. [Google Scholar] [CrossRef]
- Haddawy, P.; Lawpoolsri, S.; Sa-Ngamuang, C.; Su Yin, M.; Barkowsky, T.; Wiratsudakul, A.; Kaewkungwal, J.; Khamsiriwatchara, A.; Sa-Angchai, P.; Sattabongkot, J.; et al. Effects of COVID-19 government travel restrictions on mobility in a rural border area of Northern Thailand: A mobile phone tracking study. PLoS ONE 2021, 16, e0245842. [Google Scholar] [CrossRef]
- Osei, S.A.; Biney, R.P.; Anning, A.S.; Nortey, L.N.; Ghartey-Kwansah, G. Low incidence of COVID-19 case severity and mortality in Africa; Could malaria co-infection provide the missing link? BMC Infect. Dis. 2022, 22, 78. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.I.H.; Albashir, A.A.D.; Elawad, O.; Homeida, A. Malaria and COVID-19: Unmasking their ties. Malar. J. 2020, 19, 457. [Google Scholar] [CrossRef] [PubMed]
- Nasomsong, W.; Luvira, V.; Phiboonbanakit, D. Case Report: Dengue and COVID-19 Coinfection in Thailand. Am. J. Trop. Med. Hyg. 2020, 104, 487–489. [Google Scholar] [CrossRef] [PubMed]
- Douglas, N.M.; Nosten, F.; Ashley, E.A.; Phaiphun, L.; van Vugt, M.; Singhasivanon, P.; White, N.J.; Price, R.N. Plasmodium vivax recurrence following falciparum and mixed species malaria: Risk factors and effect of antimalarial kinetics. Clin. Infect. Dis. 2011, 52, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Shanks, G.D.; White, N.J. The activation of vivax malaria hypnozoites by infectious diseases. Lancet Infect. Dis. 2013, 13, 900–906. [Google Scholar] [CrossRef]
- Guha, S.K.; Biswas, M.; Gupta, B.; Acharya, A.; Halder, S.; Saha, B.; Chatterjee, M.; Kundu, P.K.; Maji, A.K. A report on incidence of COVID-19 among febrile patients attending a malaria clinic. Trop. Parasitol. 2021, 11, 38–41. [Google Scholar] [CrossRef]
- Orish, V.N.; Boakye-Yiadom, E.; Ansah, E.K.; Alhassan, R.K.; Duedu, K.; Awuku, Y.A.; Owusu-Agyei, S.; Gyapong, J.O. Is malaria immunity a possible protection against severe symptoms and outcomes of COVID-19? Ghana Med. J. 2021, 55, 56–63. [Google Scholar] [CrossRef]


| Laboratory Test | Result | Normal Range |
|---|---|---|
| Hemoglobin (Hb) | 11.5 | 13.8–17.2 g/dL |
| Hematocrit (Hct) | 34 | 40.7–50.3% |
| Red blood cell count | 4.27 | 3.50–5.50 × 106 cell/uL |
| White blood cell count | 4190 | 4000–10,000 cell/cu.m |
| Platelet count | 92,000 | 140,000–400,000 cell/cu.m |
| Mean corpuscular volume (MCV) | 80.4 | 80–100 fL |
| Mean corpuscular hemoglobin (MCH) | 26.9 | 27–31 pg |
| Mean corpuscular hemoglobin concentration (MCHC) | 33.5 | 31–37 g/dL |
| Neutrophil | 59 | 50–70% |
| Lymphocyte | 21 | 20–40% |
| Monocyte | 16 | 3–8% |
| Eosinophil | 2 | 0–5% |
| Basophil | 0 | 0–2% |
| Atypical lymphocyte | 2 | 0 |
| Red blood cell morphology | Normal | Normal |
| Malaria (Thin–Thick film) | Positive | |
| Malaria type | Plasmodium vivax | |
| Parasitemia | 0.35% | |
| SARS-CoV2 Real time RT-PCR | Detected | |
| Nasopharyngeal swab | N gene Ct = 27.01 | |
| ORF1 ab gene Ct = 25.94 | ||
| Dengue NS1 | Negative | |
| Dengue Ab,IgM | Negative | |
| Dengue Ab,IgG | Negative | |
| Leptospira Antibody | IgM weakly positive |
| Laboratory Test | Result | Normal Range |
|---|---|---|
| Blood urea nitrogen (BUN) | 16 | 7–25 mg/dL |
| Creatinine | 0.68 | 0.70–1.17 mg/dL |
| e-GFR | 132.73 | 97.00–137.00 mL/mon/L |
| Sodium (Na) | 133 | 135–145 mmol/L |
| Potassium (K) | 3.6 | 3.5–5.1 mmol/L |
| Chloride (Cl) | 93 | 99–111 mmol/L |
| Carbon dioxide (CO2) | 24 | 22–33 mmol/L |
| Total Protein | 6.8 | 6.0–8.3 g/dL |
| Albumin (Blood) | 3.5 | 3.2–5.2 g/dL |
| Globulin | 3.3 | 2.0–3.0 g/dL |
| Total Bilirubin | 1.6 | 0–2 mg/dL |
| Direct Bilirubin | 0.6 | 0–0.2 mg/dL |
| Aspartate transaminase (AST) | 22 | 0–35 U/L |
| Alanine transaminase (ALT) | 42 | 0–45 U/L |
| Alkaline phosphatase (ALP) | 133 | 53–128 U/L |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boonyarangka, P.; Phontham, K.; Sriwichai, S.; Poramathikul, K.; Harncharoenkul, K.; Kuntawunginn, W.; Maneesrikhum, N.; Srisawath, S.; Seenuan, C.; Thanyakait, C.; et al. Co-Infection with Plasmodium vivax and COVID-19 in Thailand. Trop. Med. Infect. Dis. 2022, 7, 145. https://doi.org/10.3390/tropicalmed7080145
Boonyarangka P, Phontham K, Sriwichai S, Poramathikul K, Harncharoenkul K, Kuntawunginn W, Maneesrikhum N, Srisawath S, Seenuan C, Thanyakait C, et al. Co-Infection with Plasmodium vivax and COVID-19 in Thailand. Tropical Medicine and Infectious Disease. 2022; 7(8):145. https://doi.org/10.3390/tropicalmed7080145
Chicago/Turabian StyleBoonyarangka, Parat, Kittijarankon Phontham, Sabaithip Sriwichai, Kamonporn Poramathikul, Krit Harncharoenkul, Worachet Kuntawunginn, Napat Maneesrikhum, Sarayouth Srisawath, Chanida Seenuan, Chattakorn Thanyakait, and et al. 2022. "Co-Infection with Plasmodium vivax and COVID-19 in Thailand" Tropical Medicine and Infectious Disease 7, no. 8: 145. https://doi.org/10.3390/tropicalmed7080145