User Perceptions of ROTEM-Guided Haemostatic Resuscitation: A Mixed Qualitative–Quantitative Study
Abstract
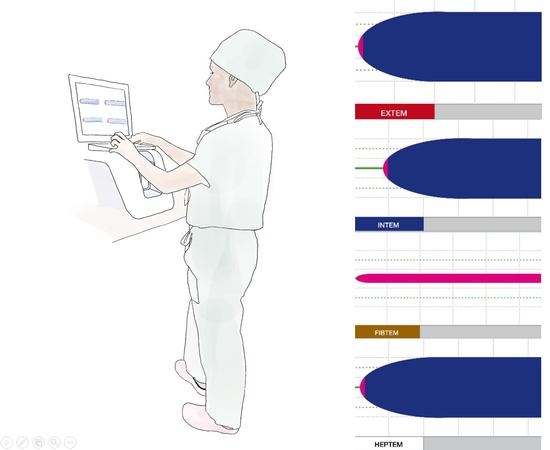
:1. Introduction
2. Materials and Methods
2.1. Approval and Consent
2.2. Study Design
2.3. Previous High-Fidelity Simulation Study
2.4. Participant Interviews and Online Survey
2.5. Outcomes and Statistical Analyses
2.5.1. Part I: Participant Interviews
2.5.2. Part II: Online Survey
2.6. Statistical Analysis
3. Results
3.1. Study and Participant Characteristics
3.2. Part I: Qualitative Analysis of Interview Answers
3.2.1. Word Count Analysis
3.2.2. Coding Template
3.2.3. Statements about ROTEM: Major Topics and Subthemes
3.2.4. Themes
3.3. Part II: Analysis of Statements Evaluated in the Online Survey
4. Discussion
4.1. Principal Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wikkelsø, A.; Wetterslev, J.; Møller, A.M.; Afshari, A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst. Rev. 2016, 2018, CD007871. [Google Scholar] [CrossRef] [PubMed]
- Riehl, K.; Lefering, R.; Maegele, M.; Caspers, M.; Migliorini, F.; Schenker, H.; Driessen, A. Is ROTEM Diagnostic in Trauma Care Associated with Lower Mortality Rates in Bleeding Patients?—A Retrospective Analysis of 7461 Patients Derived from the TraumaRegister DGU((R)). J. Clin. Med. 2022, 11, 6150. [Google Scholar] [CrossRef] [PubMed]
- Serraino, G.F.; Murphy, G.J. Routine use of viscoelastic blood tests for diagnosis and treatment of coagulopathic bleeding in cardiac surgery: Updated systematic review and meta-analysis. Br. J. Anaesth. 2017, 118, 823–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luz, L.T.; Nascimento, B.; Shankarakutty, A.K.; Rizoli, S.; Adhikari, N.K. Effect of thromboelastography (TEG(R)) and rotational thromboelastometry (ROTEM(R)) on diagnosis of coagulopathy, transfusion guidance and mortality in trauma: Descriptive systematic review. Crit Care 2014, 18, 518. [Google Scholar] [CrossRef] [Green Version]
- Weber, C.F.; Zacharowski, K. Point of Care 2.0: Coagulation Monitoring Using Rotem(R) Sigma and Teg(R) 6S. Anasthesiol. Intensiv. Notf. Schmerzther 2018, 53, 412–424. [Google Scholar]
- Whiting, D.; DiNardo, J.A. TEG and ROTEM: Technology and clinical applications. Am. J. Hematol. 2014, 89, 228–232. [Google Scholar] [CrossRef]
- Neerman-Arbez, M.; De Moerloose, P.; Casini, A. Laboratory and Genetic Investigation of Mutations Accounting for Congenital Fibrinogen Disorders. Semin. Thromb. Hemost. 2016, 42, 356–365. [Google Scholar]
- Gonzalez, E.; Moore, E.E.; Moore, H.B.; Chapman, M.P.; Chin, T.L.; Ghasabyan, A.; Sauaia, A. Goal-directed Hemostatic Resuscitation of Trauma-induced Coagulopathy: A Pragmatic Randomized Clinical Trial Comparing a Viscoelastic Assay to Conventional Coagulation Assays. Ann. Surg. 2016, 263, 1051–1059. [Google Scholar] [CrossRef]
- Wake, E.; Walters, K.; Winearls, J.; Marshall, A.P. Implementing and sustaining Point of Care ROTEM(R) into a trauma activation protocol for the management of patients with traumatic injury: A mixed-methods study. Aust. Crit. Care 2022, in press. [Google Scholar] [CrossRef]
- Kvint, S.; Schuster, J.; Kumar, M.A. Neurosurgical applications of viscoelastic hemostatic assays. Neurosurg. Focus 2017, 43, E9. [Google Scholar] [CrossRef] [Green Version]
- Weber, C.F.; Görlinger, K.; Meininger, D.; Herrmann, E.; Bingold, T.; Moritz, A.; Zacharowski, K. Point-of-care testing: A prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology 2012, 117, 531–547. [Google Scholar] [CrossRef] [Green Version]
- Görlinger, K.; Dirkmann, D.; Hanke, A.A.; Kamler, M.; Kottenberg, E.; Thielmann, M.; Peters, J. First-line therapy with coagulation factor concentrates combined with point-of-care coagulation testing is associated with decreased allogeneic blood transfusion in cardiovascular surgery: A retrospective, single-center cohort study. Anesthesiology 2011, 115, 1179–1191. [Google Scholar] [CrossRef] [Green Version]
- Mallett, S.V. Clinical Utility of Viscoelastic Tests of Coagulation (TEG/ROTEM) in Patients with Liver Disease and during Liver Transplantation. Semin. Thromb. Hemost. 2015, 41, 527–537. [Google Scholar] [CrossRef] [Green Version]
- Sahli, S.D.; Pedrazzi, N.; Braun, J.; Spahn, D.R.; Kaserer, A.; Plock, J.A. Effect of a factor-based coagulation management on blood product use after major burn injury: A retrospective cohort study. Burns 2021, 47, 1486–1494. [Google Scholar] [CrossRef]
- Simurda, T.; Casini, A.; Stasko, J.; Hudecek, J.; Skornova, I.; Vilar, R.; Neerman-Arbez, M.; Kubisz, P. Perioperative management of a severe congenital hypofibrinogenemia with thrombotic phenotype. Thromb. Res. 2020, 188, 1–4. [Google Scholar] [CrossRef]
- Simurda, T.; Caccia, S.; Asselta, R.; Zolkova, J.; Stasko, J.; Skornova, I.; Kubisz, P. Congenital hypofibrinogenemia associated with a novel heterozygous nonsense mutation in the globular C-terminal domain of the gamma-chain (p.Glu275Stop). J. Thromb. Thrombolysis 2020, 50, 233–236. [Google Scholar] [CrossRef]
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European guideline on management of major bleeding and coagulopathy following trauma: Fifth edition. Crit. Care 2019, 23, 98. [Google Scholar] [CrossRef] [Green Version]
- American Society of Anesthesiologists. Practice guidelines for perioperative blood management: An updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology 2015, 122, 241–275. [Google Scholar] [CrossRef]
- Tibi, P.; McClure, R.S.; Huang, J.; Baker, R.A.; Fitzgerald, D.; Mazer, C.D.; Stone, M.; Chu, D.; Stammers, A.H.; Dickinson, T.; et al. STS/SCA/AmSECT/SABM Update to the Clinical Practice Guidelines on Patient Blood Management. Ann. Thorac. Surg. 2021, 112, 981–1004. [Google Scholar] [CrossRef]
- Rana, A.; Dumka, A.; Singh, R.; Panda, M.K.; Priyadarshi, N.; Twala, B. Imperative Role of Machine Learning Algorithm for Detection of Parkinson’s Disease: Review, Challenges and Recommendations. Diagnostics 2022, 12, 2003. [Google Scholar] [CrossRef]
- Busnatu, Ș.; Niculescu, A.-G.; Bolocan, A.; Petrescu, G.E.D.; Păduraru, D.N.; Năstasă, I.; Lupușoru, M.; Geantă, M.; Andronic, O.; Grumezescu, A.M.; et al. Clinical Applications of Artificial Intelligence—An Updated Overview. J. Clin. Med. 2022, 11, 2265. [Google Scholar] [CrossRef] [PubMed]
- Fryan, L.H.A.; Alazzam, M.B. Survival Analysis of Oncological Patients Using Machine Learning Method. Healthcare 2022, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Kumar, P.; Deb, D.; Unguresan, M.-L.; Muresan, V. Artificial Intelligence and Machine Learning Based Intervention in Medical Infrastructure: A Review and Future Trends. Healthcare 2023, 11, 207. [Google Scholar] [CrossRef] [PubMed]
- Endsley, M.R. Designing for Situation Awareness: An Approach to User-Centered Design, 2nd ed.; CRC Press Inc.: Boca Raton, FL, USA, 2011. [Google Scholar]
- Schulz, C.M.; Endsley, M.R.; Kochs, E.F.; Gelb, A.W.; Wagner, K.J. Situation awareness in anesthesia: Concept and research. Anesthesiology 2013, 118, 729–742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Said, S.; Roche, T.R.; Braun, J.; Ganter, M.T.; Meybohm, P.; Herrmann, J.; Zacharowski, K.; Raimann, F.J.; Piekarski, F.; Rivas, E.; et al. Effects of an Animated Blood Clot Technology (Visual Clot) on the Decision-Making of Users Inexperienced in Viscoelastic Testing: Multicenter Trial. J. Med. Internet Res. 2021, 23, e27124. [Google Scholar] [CrossRef]
- Rössler, J.; Meybohm, P.; Spahn, D.R.; Zacharowski, K.; Braun, J.; Nöthiger, C.B.; Tscholl, D.W. Improving decision making through presentation of viscoelastic tests as a 3D animated blood clot: The Visual Clot. Anaesthesia 2020, 75, 1059–1069. [Google Scholar] [CrossRef]
- Roche, T.R.; Said, S.; Rössler, J.; Gozdzik, M.; Meybohm, P.; Zacharowski, K.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Physicians’ Perceptions of a Situation Awareness–Oriented Visualization Technology for Viscoelastic Blood Coagulation Management (Visual Clot): Mixed Methods Study. JMIR Serious Games 2020, 8, e19036. [Google Scholar] [CrossRef]
- Guetterman, T.C.; Fetters, M.D.; Creswell, J.W. Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research Through Joint Displays. Ann. Fam. Med. 2015, 13, 554–561. [Google Scholar] [CrossRef]
- Smajic, E.; Avdic, D.; Pasic, A.; Prcic, A.; Stancic, M. Mixed Methodology of Scientific Research in Healthcare. Acta Inform. Medica 2022, 30, 57–60. [Google Scholar] [CrossRef]
- Kaur, N.; Vedel, I.; El Sherif, R.; Pluye, P. Practical mixed methods strategies used to integrate qualitative and quantitative methods in community-based primary health care research. Fam. Pract. 2019, 36, 666–671. [Google Scholar] [CrossRef]
- Symon, G.; Cassell, C. Qualitative Organizational Research: Core Methods and Current Challenges; SAGE Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Tanaka, K.A.; Bolliger, D. Point-of-Care Coagulation Testing in Cardiac Surgery. Semin. Thromb. Hemost. 2017, 43, 386–396. [Google Scholar] [CrossRef]
- Van Heer, S.; Cofie, N.; Gutiérrez, G.; Upagupta, C.; Szulewski, A.; Chaplin, T. Shaken and stirred: Emotional state, cognitive load, and performance of junior residents in simulated resuscitation. Can. Med. Educ. J. 2021, 12, 24–33. [Google Scholar] [CrossRef]
- Vella, K.M.; Hall, A.K.; van Merrienboer, J.J.; Ma, W.M.H.; Szulewski, A. An exploratory investigation of the measurement of cognitive load on shift: Application of cognitive load theory in emergency medicine. AEM Educ. Train. 2021, 5, e10634. [Google Scholar] [CrossRef]
- Szulewski, A.; Howes, D.; van Merriënboer, J.J.; Sweller, J. From Theory to Practice: The Application of Cognitive Load Theory to the Practice of Medicine. Acad. Med. 2020, 96, 24–30. [Google Scholar] [CrossRef]
- Gaba, D.M.; Howard, S.; Small, S.D. Situation Awareness in Anesthesiology. Hum. Factors: J. Hum. Factors Ergon. Soc. 1995, 37, 20–31. [Google Scholar] [CrossRef]
- Kang, J.; Hu, J.; Yan, C.; Xing, X.; Tu, S.; Zhou, F. Development and applications of the anaesthetists’ non-technical skills behavioural marker system: Protocol for a systematic review. BMJ Open 2022, 12, e065519. [Google Scholar] [CrossRef]
- Budowski, A.D.; Bergauer, L.; Castellucci, C.; Braun, J.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Roche, T.R. Improved Task Performance, Low Workload, and User-Centered Design in Medical Diagnostic Equipment Enhance Decision Confidence of Anesthesia Providers: A Meta-Analysis and a Multicenter Online Survey. Diagnostics 2022, 12, 1835. [Google Scholar] [CrossRef]
- Tscholl, D.W.; Rössler, J.; Said, S.; Kaserer, A.; Spahn, D.R.; Nöthiger, C.B. Situation Awareness-Oriented Patient Monitoring with Visual Patient Technology: A Qualitative Review of the Primary Research. Sensors 2020, 20, 2112. [Google Scholar] [CrossRef] [Green Version]
- Castellucci, C.; Braun, J.; Said, S.; Roche, T.R.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Akbas, S. Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study. Diagnostics 2022, 12, 1269. [Google Scholar] [CrossRef]
- Walter, W.; Haferlach, C.; Nadarajah, N.; Schmidts, I.; Kühn, C.; Kern, W.; Haferlach, T. How artificial intelligence might disrupt diagnostics in hematology in the near future. Oncogene 2021, 40, 4271–4280. [Google Scholar] [CrossRef]
- Tomašev, N.; Glorot, X.; Rae, J.W.; Zielinski, M.; Askham, H.; Saraiva, A.; Mottram, A.; Meyer, C.; Ravuri, S.; Protsyuk, I.; et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 2019, 572, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Ochieng, P.A. An Analysis of the Strengths and Limitation of Qualitative and Quantitative Research Paradigms. Probl. Educ. 21st Century 2009, 13, 13–38. [Google Scholar]






| Participant Characteristics | |
|---|---|
| Interview Participants (n = 77) | |
| Female participants, n (%) | 46 (59.7) |
| Senior physicians, n (%) | 8 (10.4) |
| Resident physicians, n (%) | 35 (45.5) |
| Anaesthesiology nurses, n (%) | 34 (44.2) |
| Anaesthesia experience in years, median (IQR) | 8 (3–10) |
| Number of ROTEM interpretations per year, median (IQR) | 26 (5–41) |
| Online survey participants (n = 52) | |
| Senior physicians, n (%) | 20 (38.5) |
| Resident physicians, n (%) | 17 (32.7) |
| Anaesthesiology nurses, n (%) | 15 (28.8) |
| Anaesthesia experience in years, median (IQR) | 8 (4–10) |
| Number of ROTEM interpretations per year, median (IQR) | 44 (7.75–50) |
| Major Topics and Subthemes | Examples |
|---|---|
| Positive Perceptions about ROTEM (148/288, 51.4%) | |
| Positive design features (30/288, 11%) |
|
| Positive usability features (34/288, 12.5%) |
|
| Quick availability of results (28/288, 10.3%) |
|
| Proven coagulation management tool (16/288, 2.9%) |
|
| High accuracy (36/288, 13.2%) |
|
| Negative perceptions about ROTEM (140/288 48.6%) | |
| Negative design features (12/288, 4.4%) |
|
| Usability problems (48/288, 17.6%) |
|
| Interference susceptibility (8/288, 2.9%) |
|
| Incompleteness (7/288, 2.6%) |
|
| Need for training (54/288, 19.8%) |
|
| Non-codable | |
| |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasciauskaite, G.; Malorgio, A.; Castellucci, C.; Budowski, A.; Schweiger, G.; Kolbe, M.; Grande, B.; Noethiger, C.B.; Spahn, D.R.; Roche, T.R.; et al. User Perceptions of ROTEM-Guided Haemostatic Resuscitation: A Mixed Qualitative–Quantitative Study. Bioengineering 2023, 10, 386. https://doi.org/10.3390/bioengineering10030386
Gasciauskaite G, Malorgio A, Castellucci C, Budowski A, Schweiger G, Kolbe M, Grande B, Noethiger CB, Spahn DR, Roche TR, et al. User Perceptions of ROTEM-Guided Haemostatic Resuscitation: A Mixed Qualitative–Quantitative Study. Bioengineering. 2023; 10(3):386. https://doi.org/10.3390/bioengineering10030386
Chicago/Turabian StyleGasciauskaite, Greta, Amos Malorgio, Clara Castellucci, Alexandra Budowski, Giovanna Schweiger, Michaela Kolbe, Bastian Grande, Christoph B. Noethiger, Donat R. Spahn, Tadzio R. Roche, and et al. 2023. "User Perceptions of ROTEM-Guided Haemostatic Resuscitation: A Mixed Qualitative–Quantitative Study" Bioengineering 10, no. 3: 386. https://doi.org/10.3390/bioengineering10030386