Which Is More Important for Health: Sleep Quantity or Sleep Quality?
Abstract
:1. Introduction
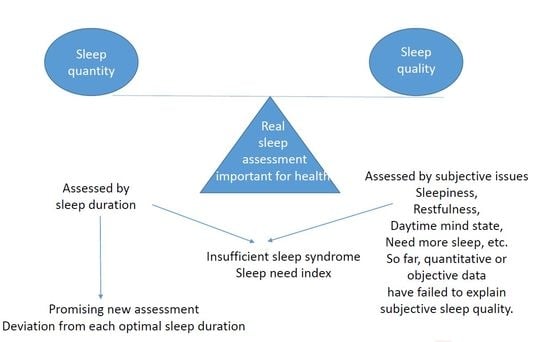
2. Sleep Quantity
3. Insufficient Sleep Syndrome
4. Sleep Need Index (SNI)
5. Future Assessment on Sleep Quantity
6. Sleepiness
7. Sleep Quality
8. Sleep Quantity and Quality in Patients with Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder
9. Quantity Versus Quality
10. Sleep Quality in Children and Adolescents
11. Another Sleep Issues to Be Investigated
12. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Irwin, M.R. Why sleep is important for health: A psychoneuroimmunology perspective. Annu. Rev. Psychol. 2015, 66, 143–172. [Google Scholar] [CrossRef] [Green Version]
- Rajaratnam, S.M.; Arendt, J. Health in a 24-h society. Lancet 2001, 358, 999–1005. [Google Scholar] [CrossRef]
- Kohyama, J. Sleep, serotonin, and suicide in Japan. J. Phsiol. Anthropol. 2011, 30, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Sekine, C.; Watanabe, Y.; Hayashida, M. No More Decline in Sleeping Time, More Time Now Spent on Necessary Activities. Public Opinion Research Division Broadcasting Culture Research Institute, Japan Broadcasting Corporation (NHK). 2016. Available online: https://www.nhk.or.jp/bunken/english/reports/pdf/report_16071301.pdf (accessed on 21 May 2021).
- Ford, E.S.; Cunningham, T.; Croft, J.B. Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep 2015, 38, 829–832. [Google Scholar] [CrossRef] [PubMed]
- Matricciani, L.; Olds, T.; Petkov, J. In search of lost sleep: Secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Rev. 2012, 16, 203–211. [Google Scholar] [CrossRef]
- Yatagai, M.; Takahashi, Y. Basic Lifestyle Habits of Toddlers Based on Data. Research on the Developmental Standard on the Basic Life Style Habit, 3rd ed.; Ichigeisha: Japan, Tokyo, 2016. (In Japanese) [Google Scholar]
- Japan Society of School Health. Annual Reports on Health of Children Attending Elementary Schools and Junior High Schools in 2015–2017; Japan Society of School Health: Japan, Tokyo, 2018. [Google Scholar]
- Sharma, S.; Kavuru, M. Sleep and metabolism: An overview. Int. J. Endocrinol. 2010, 2010, 270832. [Google Scholar] [CrossRef] [Green Version]
- Bin, Y.S.; Marshall, N.S.; Glozier, N. Secular trends in adult sleep duration: A systematic review. Sleep Med. Rev. 2012, 16, 223–230. [Google Scholar] [CrossRef]
- Matricciani, L.; Bin, Y.S.; Lallukka, T.; Kronholm, E.; Dumuid, D.; Paquet, C.; Olds, T. Past, present, and future: Trends in sleep duration and implications for public health. Sleep Health 2017, 5, 317–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hammond, E.C. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am. J. Public Health Nations Health 1964, 54, 11–23. [Google Scholar] [CrossRef]
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychological Association: District of Columbia, WA, USA, 1994. [Google Scholar]
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychological Association: District of Columbia, WA, USA, 2013. [Google Scholar]
- Ford, D.E.; Kamerow, D.B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989, 262, 1479–1484. [Google Scholar] [CrossRef]
- Pilz, L.K.; Keller, L.K.; Lenssen, D.; Roenneberg, T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep 2018, 41. [Google Scholar] [CrossRef] [PubMed]
- Faerman, A.; Kaplan, K.A.; Zeitzer, J.M. Subjective sleep quality is poorly associated with actigraphy and heart rate measures in community-dwelling older men. Sleep Med. 2020, 73, 154–161. [Google Scholar] [CrossRef]
- Kaplan, K.A.; Hardas, P.P.; Redline, S.; Zeitzer, J.M.; Sleep Heart Health Study Research Group. Correlates of sleep quality in midlife and beyond: A machine learning analysis. Sleep Med. 2017, 34, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, K.A.; Hirshman, J.; Hernandez, B.; Stefanick, M.L.; Hoffman, A.R.; Redline, S.; Ancoli-Israel, S.; Stone, K.; Friedman, L.; Zeitzer, J.M. Osteoporotic Fractures in Men (MrOS), Study of Osteoporotic Fractures SOF Research Groups. When a gold standard isn’t so golden: Lack of prediction of subjective sleep quality from sleep polysomnography. Biol. Psychol. 2017, 123, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Clark, A.J.; Salo, P.; Lange, T.; Jennum, P.; Virtanen, M.; Pentti, J.; Kivimäki, M.; Rod, N.H.; Vahtera, J. Onset of impaired sleep and cardiovascular disease risk factors: A longitudinal study. Sleep 2016, 39, 1709–1718. [Google Scholar] [CrossRef]
- Falbe, J.; Davison, K.K.; Franckle, R.L.; Ganter, C.; Gortmaker, S.L.; Smith, L.; Land, T.; Taveras, E.M. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015, 135, e367–e375. [Google Scholar] [CrossRef] [Green Version]
- Kaneko, H.; Morita, H.; Komuro, I. Beautiful harmony of the Japanese precious healthcare legacies for the new imperial era. Circ. J. 2020, 84, 371–373. [Google Scholar] [CrossRef] [Green Version]
- Kaneko, H.; Itoh, H.; Kiriyama, H.; Kamon, T.; Fujiu, K.; Morita, K.; Michihata, N.; Jo, T.; Takeda, N.; Morita, H.; et al. Restfulness from sleep and subsequent cardiovascular disease in the general population. Sci. Rep. 2020, 10, 19674. [Google Scholar] [CrossRef] [PubMed]
- Lao, X.Q.; Liu, X.; Deng, H.B.; Chan, T.C.; Ho, K.F.; Wang, F.; Vermeulen, R.; Tam, T.; Wong, M.; Tse, L.A.; et al. Sleep quality, sleep duration, and the risk of coronary heart disease: A prospective cohort study with 60,586 adults. J. Clin. Sleep Med. 2018, 4, 109–117. [Google Scholar] [CrossRef] [Green Version]
- Moore, P.J.; Adler, N.E.; Williams, D.R.; Jackson, J.S. Socioeconomic status and health: The role of sleep. Psychosom. Med. 2002, 64, 337–344. [Google Scholar] [CrossRef]
- Yang, T.C.; Matthews, S.A.; Chen, V.Y. Stochastic variability in stress, sleep duration, and sleep quality across the distribution of body mass index: Insights from quantile regression. Int. J. Behav. Med. 2014, 21, 282–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, T.C.; Park, K. To what extent do sleep quality and duration mediate the effect of perceived discrimination on health? Evidence from Philadelphia. J. Urban Health Bull. N. Y. Acad. Med. 2015, 92, 1024–1037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruni, O.; Sette, S.; Fontanesi, L.; Baiocco, R.; Laghi, F.; Baumgartner, E. Technology use and sleep quality in preadolescence and adolescence. J. Clin. Sleep Med. 2015, 11, 1433–1441. [Google Scholar] [CrossRef]
- Berentzen, N.E.; Smit, H.A.; Bekkers, M.B.; Brunekreef, B.; Koppelman, G.H.; De Jongste, J.C.; Kerkhof, M.; Van Rossem, L.; Wijga, A.H. Time in bed, sleep quality and associations with cardiometabolic markers in children: The Prevention and Incidence of Asthma and Mite Allergy birth cohort study. J. Sleep Res. 2014, 23, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Roffwarg, H.P.; Muzio, J.N.; Dement, W.C. Ontogenetic development of the human sleep–dream cycle. Science 1966, 152, 604–619. [Google Scholar] [CrossRef] [PubMed]
- Iglowstein, I.; Jenni, O.G.; Molinari, L.; Largo, R.H. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 2003, 111, 302–337. [Google Scholar] [CrossRef]
- National Sleep Foundation. National Sleep Foundation Recommends New Sleep Times. Available online: https://www.sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times (accessed on 21 May 2012).
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef]
- WHO. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age. Available online: https://apps.who.int/iris/handle/10665/311664 (accessed on 21 May 2021).
- Mindell, J.A.; Sadeh, A.; Wiegand, B.; How, T.H.; Goh, D.Y. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010, 11, 274–280. [Google Scholar] [CrossRef]
- Carter, B.; Rees, P.; Hale, L.; Bhattacharjee, D.; Paradkar, M.S. Association between portable screen-based media device access or use and sleep outcomes: A systematic review and meta-analysis. JAMA Pediatr. 2016, 170, 1202–1208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quante, M.; Khandpur, N.; Kontos, E.Z.; Bakker, J.P.; Owens, J.A.; Redline, S. Let’s talk about sleep: A qualitative examination of levers for promoting healthy sleep among sleep-deprived vulnerable adolescents. Sleep Med. 2019, 60, 81–88. [Google Scholar] [CrossRef]
- Kohyama, J.; Shiiki, T.; Ohinata-Sugimoto, J.; Hasegawa, T. Potentially harmful sleep habits of 3-year-old children in Japan. J. Dev. Behav. Pediatr. 2002, 23, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, E.; Lee, J.S.; Mori, K.; Kawakubo, K. Clustering patterns of obesity-related multiple lifestyle behaviours and their associations with overweight and family environments: A cross-sectional study in Japanese preschool children. BMJ Open 2016, 6, e012773. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, K.; Hasegawa, T.; Kawahashi, I.; Imada, S. Preschool children’s eating and sleeping habits: Late rising and brunch on weekends is related to several physical and mental symptoms. Sleep Med. 2019, 61, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, J.; Ono, M.; Anzai, Y.; Kishino, A.; Tamanuki, K.; Moriyama, K.; Saito, Y.; Emoto, R.; Fuse, G.; Hatai, Y. Factors associated with sleep duration among pupils. Pediatr. Int. 2020, 62, 716–724. [Google Scholar] [CrossRef]
- Gong, Q.H.; Li, H.; Zhang, X.H.; Zhang, T.; Cui, J.; Xu, G.Z. Associations between sleep duration and physical activity and dietary behaviors in Chinese adolescents: Results from the Youth Behavioral Risk Factor Surveys of 2015. Sleep Med. 2017, 37, 168–173. [Google Scholar] [CrossRef]
- Taheri, S. The link between short SD and obesity: We should recommend more sleep to prevent obesity. Arch. Dis. Child. 2006, 91, 881–884. [Google Scholar] [CrossRef] [Green Version]
- Mindell, J.A.; Owens, J.; Alves, R.; Bruni, O.; Goh, D.Y.; Hiscock, H.; Kohyama, J.; Sadeh, A. Give children and adolescents the gift of a good night’s sleep: A call to action. Sleep Med. 2011, 12, 203–204. [Google Scholar] [CrossRef]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Westchester, IL, USA, 2014. [Google Scholar]
- Carskadon, M.A.; Dement, W.C. Normal human sleep: An overview. In Principles and Practice of Sleep Medicine, 6th ed.; Kryger, M.H., Roth, T., Dement, W.C., Eds.; Elsevier Saunders: Philadelphia, PA, USA, 2017; pp. 15–24. [Google Scholar]
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The global problem of insufficient sleep and its serious public health implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohyama, J.; Anzai, Y.; Ono, M.; Kishino, A.; Tamanuki, K.; Takada, K.; Inoue, K.; Horiuchi, M.; Hatai, Y. Insufficient sleep syndrome: An unrecognized but important clinical entity. Pediatr Int. 2018, 60, 372–375. [Google Scholar] [CrossRef]
- Kohyama, J. Sleep need. In Paediatric Sleep Disorders: A Practical Guide and Cases; Li, A., Ed.; Springer: Berlin, Germany, in press.
- Léger, D.; du Roscoat, E.; Bayon, V.; Guignard, R.; Pâquereau, J.; Beck, F. Short sleep in young adults: Insomnia or sleep debt? Prevalence and clinical description of short sleep in a representative sample of 1004 young adults from France. Sleep Med. 2011, 12, 454–462. [Google Scholar] [CrossRef]
- Komada, Y.; Breugelmans, R.; Drake, C.L.; Nakajima, S.; Tamura, N.; Tanaka, H.; Inoue, S.; Inoue, Y. Social jetlag affects subjective daytime sleepiness in school-aged children and adolescents: A study using the Japanese version of the Pediatric Daytime Sleepiness Scale (PDSS-J). Chronobiol Int. 2016, 33, 1311–1319. [Google Scholar] [CrossRef]
- Dewald, J.F.; Meijer, A.M.; Oort, F.J.; Kerkhof, G.A.; Bögels, A.M. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med. Rev. 2010, 14, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Zion, M.; Shiloh, E. Evening chronotype and sleepiness predict impairment in executive abilities and academic performance of adolescents. Chronobiol. Int. 2018, 35, 137–145. [Google Scholar] [CrossRef]
- Kohyama, J. Associations of adolescents’ lifestyle habits with their daytime functioning in Japan. Sleep Sci. 2020, 13, 286–292. [Google Scholar]
- Owens, J.A.; Dearth-Wesley, T.; Lewin, D.; Gioia, G.; Whitaker, R.C. Self-regulation and sleep duration, sleepiness, and chronotype in adolescents. Pediatrics 2016, 138, e20161406. [Google Scholar] [CrossRef] [Green Version]
- Gustafsson, M.L.; Laaksonen, C.; Aromaa, M.; Löyttyniemi, E.; Salanterä, S. The prevalence of neck-shoulder pain, back pain and psychological symptoms in association with daytime sleepiness—A prospective follow-up study of school children aged 10 to 15. Scand. J. Pain 2018, 18, 389–397. [Google Scholar] [CrossRef]
- Raine, A.; Venables, P.H. Adolescent daytime sleepiness as a risk factor for adult crime. J. Child Psychol. Psychiatr. Allied Discipl. 2017, 58, 728–735. [Google Scholar] [CrossRef]
- Hoddes, E.; Zarcone, V.; Smythe, H.; Phillips, R.; Dement, W.C. Quantification of sleepiness: A new approach. Psychophysiology 1973, 10, 431–436. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozgonyi, R.; Dombi, I.; Janszky, J.; Kovács, N.; Faludi, B. Low test-retest reliability of the Epworth Sleepiness Scale within a substantial short time frame. J. Sleep Res. 2021, 25, e13277. [Google Scholar]
- Kohyama, J. Determinants of sleepiness among pupils in Kanto district of Japan. J. Behav. Brain Sci. 2021, 11, 97–106. [Google Scholar] [CrossRef]
- Fabbri, M.; Beracci, A.; Martoni, M.; Meneo, D.; Tonetti, L.; Natale, V. Measuring subjective sleep quality: A review. Int. J. Environ. Res. Public Health 2021, 18, 1082. [Google Scholar] [CrossRef]
- Kohyama, J. Factors Affecting the Quality of Sleep in Children. Children 2021, 8, 499. [Google Scholar] [CrossRef]
- Ramlee, F.; Sanborn, A.N.; Tang, N.K.Y. What Sways People’s Judgment of Sleep Quality? A Quantitative Choice-Making Study with Good and Poor Sleepers. Sleep 2017, 40, zsx091. [Google Scholar]
- Bin, Y.S. Is sleep quality more important than sleep duration for public health? Sleep 2016, 39, 1629–1630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fadzil, A. Factors Affecting the Quality of Sleep in Children. Children 2021, 8, 122. [Google Scholar] [CrossRef]
- Lugo, J.; Fadeuilhe, C.; Gisbert, L.; Setien, I.; Delgado, M.; Corrales, M.; Richarte, V.; Ramos-Quiroga, J.A. Sleep in adults with autism spectrum disorder and attention deficit/hyperactivity disorder: A systematic review and meta-analysis. Eur. Neuropsychopharmacol. 2020, 38, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Kim, H.-B.; Lee, K.-W. Association between sleep duration and attention-deficit hyperactivity disorder: A system- atic review and meta-analysis of observational studies. J. Affect. Disord. 2019, 256, 62–69. [Google Scholar] [CrossRef] [PubMed]
- van der Heijden, K.B.; Stoffelsen, R.J.; Popma, A.; Swaab, H. Sleep, chronotype, and sleep hygiene in children with attention-deficit/hyperactivity disorder, autism spectrum disorder, and controls. Eur. Child Adolesc. Psychiatry 2018, 27, 99–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seow, L.; Tan, X.W.; Chong, S.A.; Vaingankar, J.A.; Abdin, E.; Shafie, S.; Chua, B.Y.; Heng, D.; Subramaniam, M. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: Results from a multi-ethnic population-based study. PLoS ONE 2020, 15, e0235816. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricardo, A.C.; Knutson, K.; Chen, J.; Appel, L.J.; Bazzano, L.; Carmona-Powell, E.; Cohan, J.; Kurella Tamura, M.; Steigerwalt, S.; Thornton, J.D.; et al. The association of sleep duration and quality with CKD progression. J. Am. Soc. Nephrol. 2017, 28, 3708–3715. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.R.; Johnson, A.H.; Shirey, M.R.; Rice, M. Sleep quality in school-aged children: A concept analysis. J. Pediatr. Nurs. 2020, 52, 54–63. [Google Scholar] [CrossRef]
- Blackwell, C.K.; Hartstein, L.E.; Elliott, A.J.; Forrest, C.B.; Ganiban, J.; Hunt, K.J.; Camargo, C.A.; LeBourgeois, M.K., Jr.; Program collaborators for Environmental influences on Child Health Outcomes (ECHO). Better sleep, better life? How sleep quality influences children’s life satisfaction. Qual. Life Res. 2020, 29, 2465–2474. [Google Scholar] [CrossRef]
- Javaheri, S.; Storfer-Isser, A.; Rosen, C.L.; Redline, S. Sleep quality and elevated blood pressure in adolescents. Circulation 2008, 118, 1034–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martikainen, S.; Pesonen, A.K.; Feldt, K.; Jones, A.; Lahti, J.; Pyhälä, R.; Heinonen, K.; Kajantie, E.; Eriksson, J.; Räikkönen, K. Poor sleep and cardiovascular function in children. Hypertension 2011, 58, 16–21. [Google Scholar] [CrossRef] [Green Version]
- Komada, Y.; Ishibashi, Y.; Hagiwara, S.; Kobori, M.; Shimura, A. A Longitudinal Study of Subjective Daytime Sleepiness Changes in Elementary School Children Following a Temporary School Closure Due to COVID-19. Children 2021, 8, 183. [Google Scholar] [CrossRef]
- Duffy, J.F.; Abbott, S.M.; Burgess, H.J.; Crowley, S.J.; Emens, J.S.; Epstein, L.J.; Gamble, K.L.; Hasler, B.P.; Kristo, D.A.; Malkani, R.G.; et al. Workshop report. Circadian rhythm sleep-wake disorders: Gaps and opportunities. Sleep 2021, 44, zsaa281. [Google Scholar] [CrossRef]
- Kolomeichuk, S.N.; Randler, C.; Morozov, A.V.; Gubin, D.G.; Drake, C.L. Social Jetlag and Excessive Daytime Sleepiness from a Sample of Russian Children and Adolescents. Nat. Sci. Sleep 2021, 13, 729–737. [Google Scholar] [CrossRef]
- Morales-Muñoz, I.; Kantojärvi, K.; Uhre, V.M.; Saaren-pää-Heikkilä, O.; Kylliäinen, A.; Pölkki, P.; Himanen, S.L.; Karlsson, L.; Karlsson, H.; Paavonen, E.J.; et al. The Effects of Genetic Background for Diurnal Preference on Sleep Development in Early Childhood. Nat. Sci. Sleep 2021, 13, 219–228. [Google Scholar] [CrossRef]
- Reutrakul, S.; Hood, M.M.; Crowley, S.J.; Morgan, M.K.; Teodori, M.; Knutson, K.L.; Van Cauter, E. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care 2013, 36, 2523–2529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weng, Z.; Ou, W.; Huang, J.; Singh, M.; Wang, M.; Zhu, Y.; Kumar, R.; Lin, S. Circadian Misalignment Rather Than Sleep Duration is Associated with MAFLD: A Population-Based Propensity Score-Matched Study. Nat. Sci. Sleep 2021, 13, 103–111. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kohyama, J. Which Is More Important for Health: Sleep Quantity or Sleep Quality? Children 2021, 8, 542. https://doi.org/10.3390/children8070542
Kohyama J. Which Is More Important for Health: Sleep Quantity or Sleep Quality? Children. 2021; 8(7):542. https://doi.org/10.3390/children8070542
Chicago/Turabian StyleKohyama, Jun. 2021. "Which Is More Important for Health: Sleep Quantity or Sleep Quality?" Children 8, no. 7: 542. https://doi.org/10.3390/children8070542