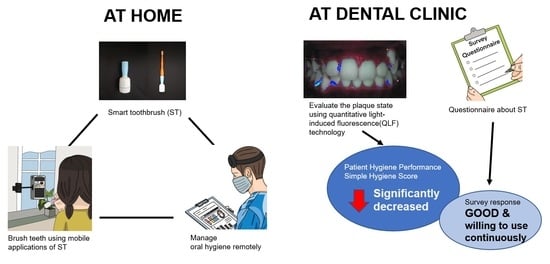
Effectiveness of an Oral Health Education Program Using a Smart Toothbrush with Quantitative Light-Induced Fluorescence Technology in Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Setting
2.2. Participants
- (i)
- Korean children aged 6–12 years, well-nourished, and in good general health.
- (ii)
- Children with plaque accumulation on the buccal surface on teeth who require tooth brushing instruction (TBI) and good brushing habits.
- (iii)
- Eruption state of permanent first molars and central incisors.
- (iv)
- Children or parents who use android software smartphone.
- (i)
- Children with molar–incisor hypoplasia.
- (ii)
- Medically compromised children (neurological disorders and cerebral palsy).
- (iii)
- Children or caregivers who withdrew their consent.
2.3. Plaque Assessment
2.4. Clinical Procedures
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loe, H. Oral hygiene in the prevention of caries and periodontal disease. Int. Dent. J. 2000, 50, 129–139. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.; Marcenes, W.; Collaborators, G.O.H. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Jepsen, S.; Blanco, J.; Buchalla, W.; Carvalho, J.C.; Dietrich, T.; Dörfer, C.; Eaton, K.A.; Figuero, E.; Frencken, J.E.; Graziani, F. Prevention and control of dental caries and periodontal diseases at individual and population level: Consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017, 44, S85–S93. [Google Scholar] [CrossRef] [Green Version]
- WHO Organization. Ending Childhood Dental Caries; WHO Implementation Manual; WHO Organization: Geneva, Switzerland, 2019. [Google Scholar]
- American Academy of Pediatric Dentistry. Caries-Risk Assessment and Management for Infants, Children, and Adolescents; The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022; pp. 266–272. [Google Scholar]
- Paunio, P.; Rautava, P.; Sillanpää, M.; Kaleva, O. Dental health habits of 3-year-old Finnish children. Community Dent. Oral Epidemiol. 1993, 21, 4–7. [Google Scholar] [CrossRef]
- Unkel, J.H.; Fenton, S.J.; Hobbs, G., Jr.; Frere, C.L. Toothbrushing ability is related to age in children. ASDC J. Dent. Child. 1995, 62, 346–348. [Google Scholar]
- Sandstrom, A.; Cressey, J.; Stecksen-Blicks, C. Tooth-brushing behaviour in 6–12 year olds. Int. J. Paediatr. Dent. 2011, 21, 43–49. [Google Scholar] [CrossRef]
- Pujar, P.; Subbareddy, V.V. Evaluation of the tooth brushing skills in children aged 6-12 years. Eur. Arch. Paediatr. Dent. 2013, 14, 213–219. [Google Scholar] [CrossRef]
- Ogasawara, T.; Watanabe, T.; Kasahara, H. Readiness for toothbrushing of young children. ASDC J. Dent. Child. 1992, 59, 353–359. [Google Scholar]
- Mohebbi, S.Z.; Virtanen, J.I.; Murtomaa, H.; VAHID-GOLPAYEGANI, M.; Vehkalahti, M.M. Mothers as facilitators of oral hygiene in early childhood. Int. J. Paediatr. Dent. 2008, 18, 48–55. [Google Scholar] [CrossRef]
- Adachi, M.; Takahashi, M.; Shinkawa, H.; Mori, H.; Nishimura, T.; Nakamura, K. Longitudinal association between smartphone ownership and depression among schoolchildren under COVID-19 pandemic. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 239–243. [Google Scholar] [CrossRef]
- Lee, K.H.; Choi, Y.Y.; Jung, E.S. Effectiveness of an oral health education programme using a mobile application for older adults: A randomised clinical trial. Gerodontology 2021, 40, 47–55. [Google Scholar] [CrossRef]
- Kim, K.D.; Jeong, J.S.; Lee, H.N.; Gu, Y.; Kim, K.S.; Lee, J.W.; Park, W. Efficacy of computer-assisted, 3D motion-capture toothbrushing instruction. Clin. Oral Investig. 2015, 19, 1389–1394. [Google Scholar] [CrossRef]
- Kim, K.-S.; Yoon, T.-H.; Lee, J.-W.; Kim, D.-J. Interactive toothbrushing education by a smart toothbrush system via 3D visualization. Comput. Methods Programs Biomed. 2009, 96, 125–132. [Google Scholar] [CrossRef]
- Lee, H.-K.; Hwang, S.-J.; Cho, S.-P.; Lee, D.-R.; You, S.-H.; Lee, K.-J.; Kim, Y.-H.; Choi, H.-S. Novel algorithm for the hemiplegic gait evaluation using a single 3-axis accelerometer. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 3964–3966. [Google Scholar] [CrossRef]
- Lee, J.-W.; Lee, K.-H.; Kim, K.-S.; Kim, D.-J.; Kim, K. Development of smart toothbrush monitoring system for ubiquitous healthcare. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, NewYork, NY, USA, 30 August–3 September 2006; pp. 6422–6425. [Google Scholar] [CrossRef]
- Lee, J.B.; Choi, D.H.; Mah, Y.J.; Pang, E.K. Validity assessment of quantitative light-induced fluorescence-digital (QLF-D) for the dental plaque scoring system: A cross-sectional study. BMC Oral Health 2018, 18, 187. [Google Scholar]
- Angelopoulou, M.V.; Oulis, C.J.; Kavvadia, K. School-based oral health-education program using experiential learning or traditional lecturing in adolescents: A clinical trial. Int. Dent. J. 2014, 64, 278–284. [Google Scholar] [CrossRef]
- Barrickman, R.W.; Penhall, O. Graphing indexes reduces plaque. J. Am. Dent. Assoc. 1973, 87, 1404–1408. [Google Scholar] [CrossRef]
- Soltani, M.K.; Jafari, F.; Taheri, M.; Soltanian, A.R.; Khoshhal, M.; Torkaman, S. Effect of 5 oral hygiene teaching methods on orthodontic patients: A single-blind randomized controlled clinical trial. Avicenna J. Dent. Res. 2019, 11, 41–47. [Google Scholar] [CrossRef]
- Solanki, R.; Tuli, A.; Dhawan, P.; Khanduri, N.; Singh, A. QLF-D: A Contemporary Plaque Control Tool in Children. Int. J. Clin. Pediatr. Dent. 2021, 14, 502. [Google Scholar] [CrossRef]
- Park, S.-W.; Kahharova, D.; Lee, J.-Y.; Lee, E.-S.; de Jong, E.d.J.; Khudanov, B.; Kim, B.-I. Clinical assessment of an automated fluorescent plaque index scoring with quantitative light-induced fluorescence. Photodiagn. Photodyn. Ther. 2020, 32, 102011. [Google Scholar] [CrossRef]
- Lee, J.; Kim, S.; Jeong, T.; Shin, J.; Lee, E.; Kim, J. Effectiveness of Oral Health Education Program using Home-using Portable Device for Children. J. Korean Acad. Pediatr. Dent. 2019, 46, 301–309. [Google Scholar] [CrossRef] [Green Version]
- Hellstadius, K.; Åsman, B.; Gustafsson, A. Improved maintenance of plaque control by electrical toothbrushing in periodontitis patients with low compliance. J. Clin. Periodontol. 1993, 20, 235–237. [Google Scholar] [CrossRef]
- Khudanov, B.; Jung, H.I.; Kahharova, D.; Lee, J.-W.; Hamidov, I.; Lee, E.-S.; Kim, B.-I. Effect of an oral health education program based on the use of quantitative light-induced fluorescence technology in Uzbekistan adolescents. Photodiagn. Photodyn. Ther. 2018, 21, 379–384. [Google Scholar] [CrossRef]
- Çolak, H.; Dülgergil, Ç.T.; Dalli, M.; Hamidi, M.M. Early childhood caries update: A review of causes, diagnoses, and treatments. J. Nat. Sci. Biol. Med. 2013, 4, 29. [Google Scholar]
- Milsom, K.; Blinkhorn, A.; Tickle, M. The incidence of dental caries in the primary molar teeth of young children receiving National Health Service funded dental care in practices in the North West of England. Br. Dent. J. 2008, 205, E14. [Google Scholar] [CrossRef]
- Maya, M.A.; Kahabuka, F.; Mbawalla, H. Effectiveness of supervised tooth-brushing and use of plaque disclosing agent on children’s tooth-brushing skills and oral hygiene: A cluster randomized trial. EC Dent. Sci. 2018, 17, 1929–1938. [Google Scholar]
- Lee, H.-J.; Lee, Y.-S.; Nam, Y.-O. Comparison of effectiveness on knowledge improvement before and after the oral health education: Focusing on foreign students. J. Korean Soc. Dent. Hyg. 2016, 16, 85–92. [Google Scholar] [CrossRef] [Green Version]








| Gender | Group I | Group II | Group III |
|---|---|---|---|
| Male (number (%)) | 14 (60.9) | 11 (52.4) | 14 (58.3) |
| Female (number (%)) | 9 (39.1) | 10 (47.6) | 10 (41.7) |
| Variables | Group | Baseline | One-Month Check | Three-Month Check | p-Value |
|---|---|---|---|---|---|
| PHP score | Group I | 0.60 ± 0.59 | 0.58 ± 0.52 | 0.36 ± 0.37 | 0.046 * |
| Group II | 0.67 ± 0.73 | 0.50 ± 0.59 | 0.43 ± 0.70 | 0.046 * | |
| Group III | 0.51 ± 0.77 | 0.24 ± 0.34 | 0.39 ± 0.64 | 0.320 | |
| SHS | Group I | 2.35 ± 1.95 | 1.96 ± 1.55 | 1.42 ± 1.49 | 0.017 * |
| Group II | 2.43 ± 1.81 | 1.46 ± 1.51 | 1.03 ± 1.09 | 0.012 * | |
| Group III | 2.29 ± 1.92 | 1.17 ± 1.44 | 1.11 ± 1.31 | 0.001 * | |
| ΔR30 (%) | Group I | 11.78 ± 13.70 | 14.43 ± 15.19 | 10.39 ± 15.19 | 0.679 |
| Group II | 11.33 ± 14.04 | 6.10 ± 8.70 | 9.43 ± 13.93 | 0.144 | |
| Group III | 14.00 ± 27.26 | 5.21 ± 7.34 | 13.38 ± 36.74 | 0.413 | |
| ΔR120 (%) | Group I | 3.09 ± 5.29 | 3.00 ± 5.11 | 2.30 ± 5.37 | 0.343 |
| Group II | 2.33 ± 5.13 | 1.10 ± 2.47 | 1.71 ± 2.92 | 0.372 | |
| Group III | 4.33 ± 13.07 | 0.67 ± 1.69 | 6.21 ± 25.22 | 0.158 |
| Source | p-Value | |
|---|---|---|
| PHP score | Time | 0.020 * |
| Time × group | 0.291 | |
| Group effect | 0.518 | |
| SHS | Time | <0.001 * |
| Time × group | 0.339 | |
| Group effect | 0.626 | |
| ΔR30 (%) | Time | 0.238 |
| Time × group | 0.185 | |
| Group effect | 0.799 | |
| ΔR120 (%) | Time | 0.303 |
| Time × group | 0.366 | |
| Group effect | 0.716 |
| Question | Answer | Baseline | Post-Intervention | |||
|---|---|---|---|---|---|---|
| N | % | N | % | p-Value | ||
| Number of times teeth are brushed per day (n) | 1 | 16 | 23.53 | 17 | 25.00 | 0.762 † |
| 2 | 38 | 55.88 | 34 | 50.00 | ||
| 3<= | 14 | 20.59 | 17 | 25.00 | ||
| Brushing time (min) | Less than 2 | 10 | 14.71 | 3 | 4.41 | 0.018 *, ‡ |
| 2 | 29 | 42.65 | 16 | 23.53 | ||
| 3 | 24 | 35.29 | 38 | 55.88 | ||
| 4 | 4 | 5.88 | 9 | 13.24 | ||
| More than 4 | 1 | 1.47 | 2 | 2.94 | ||
| Difficulty of brushing | Very hard | 1 | 1.47 | 4 | 5.88 | 0.366 ‡ |
| Hard | 23 | 33.82 | 19 | 27.94 | ||
| Little hard | 44 | 64.71 | 45 | 66.18 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Lee, T.; Jung, H.-I.; Park, W.; Song, J.S. Effectiveness of an Oral Health Education Program Using a Smart Toothbrush with Quantitative Light-Induced Fluorescence Technology in Children. Children 2023, 10, 429. https://doi.org/10.3390/children10030429
Lee J, Lee T, Jung H-I, Park W, Song JS. Effectiveness of an Oral Health Education Program Using a Smart Toothbrush with Quantitative Light-Induced Fluorescence Technology in Children. Children. 2023; 10(3):429. https://doi.org/10.3390/children10030429
Chicago/Turabian StyleLee, Jihyun, Taeyang Lee, Hoi-In Jung, Wonse Park, and Je Seon Song. 2023. "Effectiveness of an Oral Health Education Program Using a Smart Toothbrush with Quantitative Light-Induced Fluorescence Technology in Children" Children 10, no. 3: 429. https://doi.org/10.3390/children10030429