Effects of Metabolic Syndrome and Sex on Stress Coping Strategies in Individuals with Depressive Disorder
Abstract
:1. Introduction
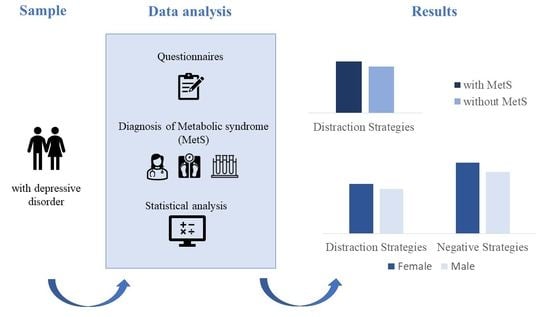
2. Materials and Methods
2.1. Procedure
2.2. Psychological Inventories
2.3. Physiological Assessment
- Serum triglycerides levels ≥ 150 mg/dL (or treatment for hyperlipidemia);
- HDL cholesterol < 40 mg/dL in men or <50 mg/dL in women;
- Blood pressure ≥ 130/85 mmHg (or diagnosed hypertension);
- Fasting blood glucose ≥ 100 mg/dL (or presence of Type 2 diabetes).
2.4. Statistical Analyses
3. Results
3.1. Descriptive Statistics
3.2. Chi-Square Test and t-Test
3.3. Multivariate Effects
3.4. ANCOVAs
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593. [Google Scholar] [CrossRef] [PubMed]
- Van de Velde, S.; Bracke, P.; Levecque, K. Gender Differences in Depression in 23 European Countries. Cross-National Variation in the Gender Gap in Depression. Soc. Sci. Med. 2010, 71, 305–313. [Google Scholar] [CrossRef]
- WHO. Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 21 February 2023).
- Greenberg, P.E.; Fournier, A.-A.; Sisitsky, T.; Simes, M.; Berman, R.; Koenigsberg, S.H.; Kessler, R.C. The Economic Burden of Adults with Major Depressive Disorder in the United States (2010 and 2018). Pharmacoeconomics 2021, 39, 653–665. [Google Scholar] [CrossRef] [PubMed]
- Han, K.-M.; Kim, M.S.; Kim, A.; Paik, J.-W.; Lee, J.; Ham, B.-J. Chronic Medical Conditions and Metabolic Syndrome as Risk Factors for Incidence of Major Depressive Disorder: A Longitudinal Study Based on 4.7 Million Adults in South Korea. J. Affect. Disord. 2019, 257, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic Syndrome-a New World-Wide Definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Wang, H.H.; Lee, D.K.; Liu, M.; Portincasa, P.; Wang, D.Q.-H. Novel Insights into the Pathogenesis and Management of the Metabolic Syndrome. Pediatr. Gastroenterol. Hepatol. Nutr. 2020, 23, 189. [Google Scholar] [CrossRef]
- McCracken, E.; Monaghan, M.; Sreenivasan, S. Pathophysiology of the Metabolic Syndrome. Clin. Dermatol. 2018, 36, 14–20. [Google Scholar] [CrossRef]
- The DECODE Study Group. Does the Constellation of Risk Factors with and without Abdominal Adiposity Associate with Different Cardiovascular Mortality Risk? Int. J. Obes. 2008, 32, 757–762. [Google Scholar] [CrossRef]
- Gami, A.S.; Witt, B.J.; Howard, D.E.; Erwin, P.J.; Gami, L.A.; Somers, V.K.; Montori, V.M. Metabolic Syndrome and Risk of Incident Cardiovascular Events and Death. J. Am. Coll. Cardiol. 2007, 49, 403–414. [Google Scholar] [CrossRef]
- Silarova, B.; Giltay, E.J.; Van Reedt Dortland, A.; Van Rossum, E.F.C.; Hoencamp, E.; Penninx, B.W.J.H.; Spijker, A.T. Metabolic Syndrome in Patients with Bipolar Disorder: Comparison with Major Depressive Disorder and Non-Psychiatric Controls. J. Psychosom. Res. 2015, 78, 391–398. [Google Scholar] [CrossRef]
- Vancampfort, D.; Stubbs, B.; Mitchell, A.J.; De Hert, M.; Wampers, M.; Ward, P.B.; Rosenbaum, S.; Correll, C.U. Risk of Metabolic Syndrome and Its Components in People with Schizophrenia and Related Psychotic Disorders, Bipolar Disorder and Major Depressive Disorder: A Systematic Review and Meta-Analysis. World Psychiatry 2015, 14, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Dalkner, N.; Bengesser, S.A.; Birner, A.; Fellendorf, F.T.; Fleischmann, E.; Großschädl, K.; Lenger, M.; Maget, A.; Platzer, M.; Queissner, R.; et al. Metabolic Syndrome Impairs Executive Function in Bipolar Disorder. Front. Neurosci. 2021, 15, 717824. [Google Scholar] [CrossRef] [PubMed]
- Hui, W.S.; Liu, Z.; Ho, S.C. Metabolic Syndrome and All-Cause Mortality: A Meta-Analysis of Prospective Cohort Studies. Eur. J. Epidemiol. 2010, 25, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Saboya, P.P.; Bodanese, L.C.; Zimmermann, P.R.; da Silva Gustavo, A.; Assumpção, C.M.; Londero, F. Metabolic Syndrome and Quality of Life: A Systematic Review. Rev. Latino-Am. Enferm. 2016, 24, e2848. [Google Scholar] [CrossRef]
- Moradi, Y.; Albatineh, A.N.; Mahmoodi, H.; Gheshlagh, R.G. The Relationship between Depression and Risk of Metabolic Syndrome: A Meta-analysis of Observational Studies. Clin. Diabetes Endocrinol. 2021, 7, 4. [Google Scholar] [CrossRef]
- Limon, V.M.; Lee, M.; Gonzalez, B.; Choh, A.C.; Czerwinski, S.A. The Impact of Metabolic Syndrome on Mental Health-Related Quality of Life and Depressive Symptoms. Qual. Life Res. 2020, 29, 2063–2072. [Google Scholar] [CrossRef]
- Mulvahill, J.S.; Nicol, G.E.; Dixon, D.; Lenze, E.J.; Karp, J.F.; Reynolds, C.F.; Blumberger, D.M.; Mulsant, B.H. Effect of Metabolic Syndrome on Late-Life Depression: Associations with Disease Severity and Treatment Resistance. J. Am. Geriatr. Soc. 2017, 65, 2651–2658. [Google Scholar] [CrossRef]
- Zhong, Y.; Hu, M.; Wang, Q.; Yang, Z.; Zhu, N.; Wang, F.; Zhang, X.; Zhang, C.; Min, J.; Wang, H.; et al. The Prevalence and Related Factors of Metabolic Syndrome in Outpatients with First-Episode Drug-Naive Major Depression Comorbid with Anxiety. Sci. Rep. 2021, 11, 3324. [Google Scholar] [CrossRef]
- Taylor, S.E.; Stanton, A.L. Coping Resources, Coping Processes, and Mental Health. Annu. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef]
- Hammen, C. Stress and Depression. Annu. Rev. Clin. Psychol. 2005, 1, 293–319. [Google Scholar] [CrossRef]
- Monroe, S.M.; Simons, A.D. Diathesis-Stress Theories in the Context of Life Stress Research: Implications for the Depressive Disorders. Psychol. Bull. 1991, 110, 406–425. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, N.; Gyntelberg, F.; Faber, J. The Appraisal of Chronic Stress and the Development of the Metabolic Syndrome: A Systematic Review of Prospective Cohort Studies. Endocr. Connect. 2014, 3, R55–R80. [Google Scholar] [CrossRef] [PubMed]
- Kuo, W.; Bratzke, L.C.; Oakley, L.D.; Kuo, F.; Wang, H.; Brown, R.L. The Association between Psychological Stress and Metabolic Syndrome: A Systematic Review and Meta-Analysis. Obes. Rev. 2019, 20, 1651–1664. [Google Scholar] [CrossRef] [PubMed]
- Tenk, J.; Mátrai, P.; Hegyi, P.; Rostás, I.; Garami, A.; Szabó, I.; Hartmann, P.; Pétervári, E.; Czopf, L.; Hussain, A.; et al. Perceived Stress Correlates with Visceral Obesity and Lipid Parameters of the Metabolic Syndrome: A Systematic Review and Meta-Analysis. Psychoneuroendocrinology 2018, 95, 63–73. [Google Scholar] [CrossRef]
- Razzoli, M.; Pearson, C.; Crow, S.; Bartolomucci, A. Stress, Overeating, and Obesity: Insights from Human Studies and Preclinical Models. Neurosci. Biobehav. Rev. 2017, 76, 154–162. [Google Scholar] [CrossRef]
- Hill, D.; Conner, M.; Clancy, F.; Moss, R.; Wilding, S.; Bristow, M.; O’Connor, D.B. Stress and Eating Behaviours in Healthy Adults: A Systematic Review and Meta-Analysis. Health Psychol. Rev. 2022, 16, 280–304. [Google Scholar] [CrossRef]
- Varela, C.; Andrés, A.; Saldaña, C. The Behavioral Pathway Model to Overweight and Obesity: Coping Strategies, Eating Behaviors and Body Mass Index. Eat Weight Disord 2020, 25, 1277–1283. [Google Scholar] [CrossRef]
- Erdmann, G.; Janke, W. Stressverarbeitungsfragebogen: SVF; Stress, Stressverarbeitung und Ihre Erfassung Durch ein Mehrdimensionales Testsystem; Hogrefe: Göttingen, Germany, 2008. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Billings, A.G.; Moos, R.H. The Role of Coping Responses and Social Resources in Attenuating the Stress of Life Events. J. Behav. Med. 1981, 4, 139–157. [Google Scholar] [CrossRef]
- Janke, W.; Erdmann, G. SVF 78: Eine Kurzform des Stressverarbeitungsfragebogens SVF 120; Kurzbeschreibung und Grundlegende Kennwerte; Manual; Hogrefe, Verlag für Psychologie: Göttingen, Germany, 2002. [Google Scholar]
- Matud, M.P. Gender Differences in Stress and Coping Styles. Personal. Individ. Differ. 2004, 37, 1401–1415. [Google Scholar] [CrossRef]
- Tamres, L.K.; Janicki, D.; Helgeson, V.S. Sex Differences in Coping Behavior: A Meta-Analytic Review and an Examination of Relative Coping. Pers. Soc. Psychol. Rev. 2002, 6, 2–30. [Google Scholar] [CrossRef]
- Cairns, K.E.; Yap, M.B.H.; Pilkington, P.D.; Jorm, A.F. Risk and Protective Factors for Depression That Adolescents Can Modify: A Systematic Review and Meta-Analysis of Longitudinal Studies. J. Affect. Disord. 2014, 169, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Holubova, M.; Prasko, J.; Ociskova, M.; Grambal, A.; Slepecky, M.; Kalusová, M.; Kamaradova, D.; Zatkova, M. Quality of Life and Coping Strategies of Outpatients with a Depressive Disorder in Maintenance Therapy—A Cross-Sectional Study. NDT 2017, 14, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Holubova, M.; Prasko, J. The Association between Self-Stigma and Coping Strategies in Depressive Disorder–a Cross-Sectional Study. Eur. Psychiatr. 2017, 41, S530. [Google Scholar] [CrossRef]
- Orzechowska, A.; Bliźniewska-Kowalska, K.; Gałecki, P.; Szulc, A.; Płaza, O.; Su, K.-P.; Georgescu, D.; Gałecka, M. Ways of Coping with Stress among Patients with Depressive Disorders. J. Clin. Med. 2022, 11, 6500. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-Regulation Strategies across Psychopathology: A Meta-Analytic Review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Johnson, D.P.; Whisman, M.A. Gender Differences in Rumination: A Meta-Analysis. Personal. Individ. Differ. 2013, 55, 367–374. [Google Scholar] [CrossRef]
- Kelly, M.A.R.; Sereika, S.M.; Battista, D.R.; Brown, C. The Relationship between Beliefs about Depression and Coping Strategies: Gender Differences. Br. J. Clin. Psychol. 2007, 46, 315–332. [Google Scholar] [CrossRef]
- Hjellset, V.T.; Ihlebæk, C.M.; Bjørge, B.; Eriksen, H.R.; Høstmark, A.T. Health-Related Quality of Life, Subjective Health Complaints, Psychological Distress and Coping in Pakistani Immigrant Women With and Without the Metabolic Syndrome: The InnvaDiab-DEPLAN Study on Pakistani Immigrant Women Living in Oslo, Norway. J. Immigr. Minor. Health 2011, 13, 732–741. [Google Scholar] [CrossRef]
- Abdullah, N.F.; Fauzi, R.M.; Harith, S. Coping with Stress: Evaluation on Metabolic Syndrome Patients in Hospital Universiti Sains Malaysia. Int. Med. J. 2017, 24, 27–30. [Google Scholar]
- Alwerdt, J.; Tian, Y.; Patterson, A.D.; Sliwinski, M. High Rumination and Low Amino Acids are Associated with an Increased Risk of Metabolic Syndrome. Innov. Aging 2019, 3 (Suppl. 1), S955. [Google Scholar] [CrossRef]
- Casagrande, M.; Boncompagni, I.; Mingarelli, A.; Favieri, F.; Forte, G.; Germanò, R.; Germanò, G.; Guarino, A. Coping Styles in Individuals with Hypertension of Varying Severity. Stress Health 2019, 35, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Anders, I.; Esterbauer, E.; Fink, A.; Ladurner, G.; Huemer, M.; Wranek, U. [Blood lipids and adaptation to stress as risk factors for stroke prevention]. Wien. Med. Wochenschr. 2000, 150, 25–31. [Google Scholar] [PubMed]
- Łukasiewicz, A.; Kiejna, A.; Cichoń, E.; Jodko-Modlińska, A.; Obrębski, M.; Kokoszka, A. Relations of Well-Being, Coping Styles, Perception of Self-Influence on the Diabetes Course and Sociodemographic Characteristics with HbA1c and BMI Among People with Advanced Type 2 Diabetes Mellitus. Diabetes Metab. Syndr. Obes. 2022, 15, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Dilling, H. Internationale Klassifikation Psychischer Störungen; Hogrefe AG: Bern, Switzerland, 2015. [Google Scholar]
- Kühner, C.; Bürger, C.; Keller, F.; Hautzinger, M. Reliabilität und Validität des revidierten Beck-Depressionsinventars (BDI-II): Befunde aus deutschsprachigen Stichproben. Nervenarzt 2007, 78, 651–656. [Google Scholar] [CrossRef]
- Finch, H. Comparison of the Performance of Nonparametric and Parametric MANOVA Test Statistics When Assumptions Are Violated. Methodology 2005, 1, 27–38. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Torres, S.J.; Nowson, C.A. Relationship between Stress, Eating Behavior, and Obesity. Nutrition 2007, 23, 887–894. [Google Scholar] [CrossRef]
- Bonnet, F.; Irving, K.; Terra, J.-L.; Nony, P.; Berthezène, F.; Moulin, P. Depressive Symptoms Are Associated with Unhealthy Lifestyles in Hypertensive Patients with the Metabolic Syndrome. J. Hypertens. 2005, 23, 611–617. [Google Scholar] [CrossRef]
- Yancura, L.A.; Aldwin, C.M.; Levenson, M.R.; Spiro, A. Coping, Affect, and the Metabolic Syndrome in Older Men: How Does Coping Get Under the Skin? J. Gerontol. Ser. B 2006, 61, P295–P303. [Google Scholar] [CrossRef]
- Bakan, G.; Inci, F.H. Predictor of Self-efficacy in Individuals with Chronic Disease: Stress-coping Strategies. J. Clin. Nurs. 2021, 30, 874–881. [Google Scholar] [CrossRef]
- Kwarta, P.; Pietrzak, J.; Miśkowiec, D.; Stelmach, I.; Górski, P.; Kuna, P.; Antczak, A.; Pietras, T. Personality Traits and Styles of Coping with Stress in Physicians. Pol. Merkur Lek. 2016, 40, 301–307. [Google Scholar]
- Schlatter, S.; Louisy, S.; Canada, B.; Thérond, C.; Duclos, A.; Blakeley, C.; Lehot, J.-J.; Rimmelé, T.; Guillot, A.; Lilot, M.; et al. Personality Traits Affect Anticipatory Stress Vulnerability and Coping Effectiveness in Occupational Critical Care Situations. Sci. Rep. 2022, 12, 20965. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.C.; Suchday, S.; Wylie-Rosett, J. Perceived Social Support, Coping Styles, and Chinese Immigrants’ Cardiovascular Responses to Stress. Int. J. Behav. Med. 2012, 19, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Puglisi-Allegra, S.; Andolina, D. Serotonin and Stress Coping. Behav. Brain Res. 2015, 277, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Nagase, Y.; Uchiyama, M.; Kaneita, Y.; Li, L.; Kaji, T.; Takahashi, S.; Konno, M.; Mishima, K.; Nishikawa, T.; Ohida, T. Coping Strategies and Their Correlates with Depression in the Japanese General Population. Psychiatry Res. 2009, 168, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Baidog, A.; Herman, G.V. The Influence of Sports and Physical Activity on the Metabolic Syndrome: A Systematic Review. Anal. Univ. Oradea Fasc. Educ. Fizică Sport 2018, 28, 39–45. [Google Scholar]
- Baik, I.; Shin, C. Prospective Study of Alcohol Consumption and Metabolic Syndrome. Am. J. Clin. Nutr. 2008, 87, 1455–1463. [Google Scholar] [CrossRef]
- Slagter, S.N.; van Vliet-Ostaptchouk, J.V.; Vonk, J.M.; Boezen, H.M.; Dullaart, R.P.; Kobold, A.C.M.; Feskens, E.J.; van Beek, A.P.; van derKlauw, M.M.; Wolffenbuttel, B.H. Associations between Smoking, Components of Metabolic Syndrome and Lipoprotein Particle Size. BMC Med. 2013, 11, 195. [Google Scholar] [CrossRef]
- Zellner, D.A.; Loaiza, S.; Gonzalez, Z.; Pita, J.; Morales, J.; Pecora, D.; Wolf, A. Food Selection Changes under Stress. Physiol. Behav. 2006, 87, 789–793. [Google Scholar] [CrossRef]
- Meléndez, J.C.; Mayordomo, T.; Sancho, P.; Tomás, J.M. Coping Strategies: Gender Differences and Development throughout Life Span. Span. J. Psychol. 2012, 15, 1089–1098. [Google Scholar] [CrossRef]
- Imaizumi, T.; Toda, T.; Maekawa, M.; Sakurai, D.; Hagiwara, Y.; Yoshida, Y.; Ando, M.; Maruyama, S. Identifying High-Risk Population of Depression: Association between Metabolic Syndrome and Depression Using a Health Checkup and Claims Database. Sci. Rep. 2022, 12, 18577. [Google Scholar] [CrossRef] [PubMed]
- Eaton, R.J.; Bradley, G. The Role of Gender and Negative Affectivity in Stressor Appraisal and Coping Selection. Int. J. Stress Manag. 2008, 15, 94–115. [Google Scholar] [CrossRef]
| Positive strategies | Pos 1: | Re- and devaluation strategies | Under-evaluation | Attribute lower stress to oneself compared to others |
| Guilt and denial | Emphasize lack of personal responsibility | |||
| Pos 2: | Distraction strategies | Distraction | Distract yourself from stress-related activities and situations | |
| Alternative satisfaction | Turn to positive activities | |||
| Pos 3: | Control strategies | Situation control | Analyze the situation, plan and execute problem solving | |
| Response control | Get your own reaction under control | |||
| Positive self-instruction | Assure oneself of competence and ability to control the situation | |||
| Negative strategies | Escape | Tendency to escape a stressful situation | ||
| Thought continuation | Rumination/cannot detach yourself mentally | |||
| Resignation | Giving up with feelings of hopelessness and helplessness | |||
| Self-blame | Attribute the burdens to their own wrong actions | |||
| Neutral strategies | Need for social support | Seek social support and help | ||
| Active avoidance | Decide to prevent or avoid stress |
| With MetS | Without MetS | Differences between | Differences between | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Mets (with vs. without) | Sex (Female vs. Male) | |||||
| (N = 57) | (N = 60) | (N = 147) | (N = 99) | t/χ2 | df | p | t/χ2 | df | p | |
| Anamnestic data | ||||||||||
| Age M ± SD | 54 ± 6.56 | 52 ± 7.24 | 54 ± 7.00 | 51 ± 7.52 | −0.595 | 361 | 0.55 | 2.680 | 361 | <0.01 |
| BDI-II M ± SD | 20.95 ± 10.15 | 19.80 ± 11.03 | 20.52 ± 9.71 | 19.12 ± 10.80 | −0.345 | 361 | 0.73 | 1.163 | 361 | 0.25 |
| BMI M ± SD | 31.4 ± 5.41 | 31.4 ± 4.63 | 24.8 ± 4.99 | 25.7 ± 3.30 | −11.493 | 204.267 | <0.001 | −2.195 | 360.604 | <0.05 |
| Obesity | ||||||||||
| Yes N (%) | 57 (48.7%) | 60 (51.3%) | 66 (70.2%) | 28 (29.8%) | 124.371 | 1 | <0.001 | 0.899 | 1 | 0.34 |
| No N (%) | 0 | 0 | 81 (53.3 %) | 71 (46.7%) | ||||||
| Education | ||||||||||
| Low education N (%) | 25 (6.89) | 29 (7.99) | 48 (13.22) | 54 (14.88) | 0.712 | 1 | 0.40 | 9.827 | 1 | <0.01 |
| High education N (%) | 32 (8.82) | 31 (8.54) | 99 (27.27) | 45 (12.40) | ||||||
| ICD−10 Diagnosis | ||||||||||
| F32 N (%) | 16 (4.41) | 28 (7.71) | 54 (14.88) | 48 (13.22) | 0.490 | 1 | 0.48 | 6.758 | 1 | < 0.01 |
| F33 N (%) | 41 (11.29) | 32 (8.82) | 93 (25.62) | 51 (14.05) | ||||||
| Stress coping scales M ± SD | ||||||||||
| Re- and devaluation (Pos 1) | 8.64 ± 3.23 | 9.40 ± 3.98 | 8.01 ± 3.34 | 8.80 ± 3.32 | −1.826 | 361 | 0.07 | −2.324 | 361 | <0.05 |
| Distraction (Pos 2) | 12.02 ± 3.58 | 9.81 ± 3.63 | 10.14 ± 3.89 | 9.43 ± 3.58 | −2.436 | 361 | <0.05 | 2.745 | 361 | <0.01 |
| Control (Pos 3) | 14.78 ± 2.74 | 13.81 ± 3.68 | 14.18 ± 3.20 | 14.18 ± 3.49 | −0.277 | 361 | 0.39 | 0.869 | 361 | 0.40 |
| Negative | 15.54 ± 4.29 | 12.79 ± 5.10 | 15.20 ± 3.72 | 13.66 ± 4.46 | 0.865 | 195.527 | 0.39 | 4.231 | 302.783 | <0.001 |
| F | p | ηp2 | |
|---|---|---|---|
| Main effect MetS | 2.496 | <0.05 | 0.028 |
| Main effect sex | 8.875 | <0.001 | 0.091 |
| Interaction MetS by sex | 1.845 | 0.12 | 0.020 |
| Age | 1.993 | 0.10 | 0.022 |
| Education | 0.910 | 0.46 | 0.010 |
| BDI-II score | 43.982 | <0.001 | 0.333 |
| Main Effect | Main Effect | Interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MetS | Sex | MetS by Sex | |||||||
| F | p | ηp2 | F | p | ηp2 | F | p | ηp2 | |
| Stress Coping Strategies | |||||||||
| Re- and devaluation (Pos 1) | 2.764 | 0.10 | 0.008 | 3.912 | <0.05 | 0.011 | 0.000 | 0.99 | 0.000 |
| Distraction (Pos 2) | 7.634 | <0.01 | 0.021 | 12.260 | <0.001 | 0.033 | 3.317 | 0.07 | 0.009 |
| Control (Pos 3) | 0.173 | 0.68 | 0.000 | 1.823 | 0.18 | 0.005 | 1.976 | 0.16 | 0.006 |
| Negative | 0.792 | 0.37 | 0.002 | 21.190 | <0.001 | 0.056 | 2.600 | 0.11 | 0.007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puchner, E.; Platzer, M.; Dalkner, N.; Schwalsberger, K.; Lenger, M.; Fellendorf, F.T.; Unterrainer, H.-F.; Schwerdtfeger, A.; Reininghaus, B.; Reininghaus, E.Z. Effects of Metabolic Syndrome and Sex on Stress Coping Strategies in Individuals with Depressive Disorder. Metabolites 2023, 13, 652. https://doi.org/10.3390/metabo13050652
Puchner E, Platzer M, Dalkner N, Schwalsberger K, Lenger M, Fellendorf FT, Unterrainer H-F, Schwerdtfeger A, Reininghaus B, Reininghaus EZ. Effects of Metabolic Syndrome and Sex on Stress Coping Strategies in Individuals with Depressive Disorder. Metabolites. 2023; 13(5):652. https://doi.org/10.3390/metabo13050652
Chicago/Turabian StylePuchner, Eva, Martina Platzer, Nina Dalkner, Karin Schwalsberger, Melanie Lenger, Frederike T. Fellendorf, Human-Friedrich Unterrainer, Andreas Schwerdtfeger, Bernd Reininghaus, and Eva Z. Reininghaus. 2023. "Effects of Metabolic Syndrome and Sex on Stress Coping Strategies in Individuals with Depressive Disorder" Metabolites 13, no. 5: 652. https://doi.org/10.3390/metabo13050652