Poisonous Plants of the Indian Himalaya: An Overview
Abstract
:1. Introduction
2. Methodology
3. Poisonous Plants of Indian Himalaya
3.1. Abrus precatorius Linn.
3.2. Aconitum ferox Wall. Ex Ser. (Syn Aconitum Atrox Walp)
3.3. Aconitum hookeri Stapf.
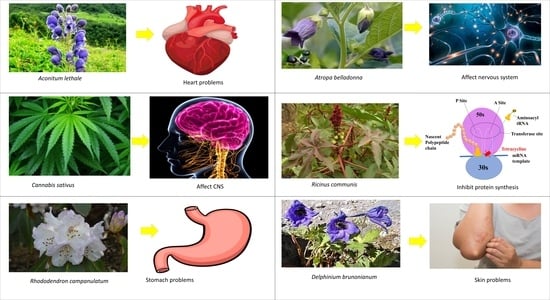
3.4. Aconitum lethale Griff. (Syn Aconitum Balfourii Stapf.)
3.5. Aconitum napellus Linn.
3.6. Aconitum spicatum (Brühl) Stapf.
3.7. Aquilegia pubiflora Wall. Ex Royle
3.8. Aesculus indica (Wall. Ex Camb.) Hoof. f.
3.9. Cannabis sativa Linn.
3.10. Convallaria majalis Linn.
3.11. Delphinium brunonianum Royle
3.12. Digitalis purpurea Linn.
3.13. Eupatorium adenophorum Spreng.
3.14. Heracleum canescens Lindl.
3.15. Hyoscyamus niger Linn.
3.16. Lantana camara Linn.
3.17. Melia azedarach Linn.
3.18. Rhododendron campanulatum D. Don
3.19. Ricinus communis Linn.
3.20. Solanum xanthocarpum Schrad. & H. Wendl.
3.21. Taxus baccata Linn.
3.22. Silybum marianum Gaertn.
| S. No. | Plant Species | Family | Toxic Compound | Symptoms | Reference |
|---|---|---|---|---|---|
| 1 | Abrus precatorius Linn. | Fabaceae | Abrin | In humans, it causes vomiting, nausea, difficulty in swallowing, throat pain, high fever, weakness irritation in eyes, severe diarrhoea and even death. After ingestion by livestock it causes nasal discharge, salivation, severe diarrhoea, abortion and eventual death in pregnant animals. | [14] |
| 2 | Aconitum chasmanthum Stapf ex Holmes | Ranunculaceae | Aconitine, diterpenoid alkaloid | Cardiotoxins and neurotoxins, skin contact cause numbness. | [27,106] |
| 3 | Aconitum ferox Wall. ex Ser. | Ranunculaceae | Pseudoaconitine and bikhaconitine | Cardio and neurotoxicity. | [38,39] |
| 4 | Aconitum lethale Griff. | Ranunculaceae | Pseudoaconitine and aconitine, balfourine | Cardio and neurotoxicity. | [43,44] |
| 5 | Aconitum laeve Royle | Ranunculaceae | 8-methyllycaconitine, 14-demethyllycaconitine, and N-deethyllycaconitine-N-aldehyde | Cardio and neurotoxicity. | [107,108] |
| 6 | Aesculus indica (Wall. Ex Camb.) Hoof. f. | Hippocastanaceae | Escin or aesculin | After consumption it causes gastro-intestinal problems, dizziness, nausea, vomiting, headache, fatigue and pruritus, while excessive consumption may cause paralysis and death. | [54] |
| 8 | Ageratum conyzoides Linn. | Asteraceae | Pyrrolizidine alkaloids | Due to contact with the plant, it causes skin problems such as as itching and rashes in susceptible individuals. Animals usually avoid browsing it, but accidental consumption causes very high fever, diarrhoea, anorexia and finally death within few hours. | [109] |
| 9 | Aloe vera (L.) Burm.f. | Xanthorrhoeaceae | Aloin or barbaloin an anthraquinone glycoside | Excessive consumption may cause nausea, abdominal pain, vomiting, hyperkalemia and cardiac dysrhythmias. | [17] |
| 10 | Anagallis arvensis Linn. | Primulaceae | Primin | Consumption of the plant causes an acute headache, nausea, unconsciousness, anorexia, body pains, general weakness, bloody diarrhoea, sudden drop in body temperature and eventually death. | [14,110] |
| 11 | Aquilegia pubiflora Wall. ex Royle | Ranunculaceae | Isovitexin, isoorientin, vitexin, chlorogenic acid, orientin, cumeric acid, sinapic acid, ferulic acid | Cardiogenic toxins cause gastroenteritis and heart palpitations. | [111] |
| 12 | Argemone Mexicana Linn. | Papaveraceae | Sanguinarine and dihydrosanguinarine alkaloids present in Argemone oil. | Seeds are toxic and cause nausea, intense headaches, vomiting, severe diarrhoea, oedema of legs and feet. | [14,112] |
| 13 | Arisaema tortuosum (Wall.) Schott | Juncaceae | Raphide (Calcium oxalate) | Intake of tubers causes irritation of the skin and mucous membrane, mouth and body pain, slow breathing and suffocation. | [113] |
| 14 | Arisaema triphyllum (L.) Schott | Araceae | Raphide (Calcium oxalate) | Irritation of the skin and the mucous membrane and body pain. | [113] |
| 15 | Artemisia nilagirica (C.B. Clarke) Pamp. | Asteraceae | Lactones | Ingestion of large doses by animals causes headaches, nausea, vomiting and abortion of pregnant animals as a result of contraction of the uterus. | [14,114] |
| 16 | Atropa belladonna Linn. | Solanaceae | Atropine and Scopolamine | Plant ingestion may cause vomiting, nausea, diarrhea and abdominal cramps. | [17] |
| 17 | Calotropis procera (Aiton) W.T.Aiton | Asclepiadaceae | Uscharin, Calotoxin, Calotropin, Calactin, and Calotropage | The milky latex of this plant act as the skin and mucous membranes irritant, that causes blisters in both humans and animals. Accidental exposure to latex can cause eye swelling and redness. Both the leaves and the latex cause diarrhea in livestock and abortion of pregnant animals. | [14,115] |
| 18 | Caltha palustris Linn. | Ranunculaceae | Protoaneminin | Poison severity of this plant is low but this plant can be toxic, and ingesting large amounts of the plant’s leaves can lead to burning of the throat, vomiting, bloody diarrhea and gastric illness. Poisonous to human beings in mature stages. | [116,117] |
| 19 | Cannabis sativa Linn. | Cannabaceae | Cannabidiol, 9-tetrahydrocannabinol (THC) | Skin allergy. | [27] |
| 20 | Capsicum chinense Jacq. | Solanaceae | Capsaicin | Consuming excessive amounts may cause stomach irritation. | [17] |
| 21 | Cassia occidentalis Linn. | Fabaceae | Achrosin, aloe-emodin, emodin | Accidental intake of pods causes nausea, vomiting, restlessness, high fever, purging and ataxia in adult humans, whereas the accidental intake of seeds in childhood causes severe brain disease. In animals it causes gastroenteritis. | [14,118,119] |
| 22 | Celtis australis Linn. | Ulmaceae | Not reported | Regular consumption of leaves causes weakness and increase in body temperature in animals. | [14] |
| 23 | Chelidonium majus Linn. | Papaveraceae | Chelidonine | Ingestion causes the severe irritation of oral mucosa. | [14] |
| 24 | Colchicum luteum Baker | Liliaceae | Colchicine | Prolonged consumption may cause salivation with frothing in the mouth, colic, polydipsia, fetid diarrhea, dizziness and eventually death in a few cases. | [14] |
| 25 | Commelina benghalensis Linn. | Commelinaceae | n-octacosanol, n triacontanol, n-dotriacontanol | The plant is bitter in taste and after ingestion it causes stomach irritation in animals. | [14] |
| 26 | Convallaria majalis Linn. | Asparagaceae | Cardenolides | Neurotoxic, ingestion may cause cardiac dysrhythmia and hyperkalemia. | [27,60,120] |
| 27 | Cuscuta reflexa Roxb. | Cuscutaceae | Cuscutin, cuscutatin, beta-sitosterol, luteolin, bergenin and kaempferol | It causes vomiting, stomach ache, anorexia and purgation in animals, and its consumption can cause abortion in pregnant animals. | [14] |
| 28 | Daphne oleoides Schreb | Thymelaeaceae | Not reported | Berries and leaves consumption creates mouth sensation, nausea, vomiting, diarrhoea, restlessness, numbness and unconsciousness. | [14] |
| 29 | Datura innoxia Mill. | Solanaceae | Atropine | In humans the strong pungent smell of the leaves causes nausea and severe headaches. Contact with the leaves causes several skin problems. Unintentional consumption of the seeds by humans and animals causes dryness and sensation of the mouth and throat, stomach ache, numbness, anorexia, mydriasis, polydipsia and restlessness. | [14] |
| 30 | Datura stramonium Linn. | Solanaceae | Atropine | Accidental ingestion of the leaves or seeds by either humans or animals may cause drowsiness, dryness and sensation of the mouth and throat, bulging of the eyeballs, mydriasis, blurred vision, startling movements, convulsions, unconsciousness and finally death. | [14] |
| 31 | Delphinium brunonianum Royle | Ranunculaceae | Diterpenoid, alkaloids, Methyllycaco-ninite | Skin allergy. | [27] |
| 32 | Digitalis purpurea Linn. | Plantaginaceae | Digitoxin and Digoxin | Ingestion of the plant may cause nausea, vomiting, abdominal pain, excessive urination, abnormal heartbeats and finally death. | [17] |
| 33 | Ephedra sinica Stapf. | Ephedraceae | Ephedrine | Plant ingestion may cause nausea, vomiting, abdominal pain, hyperkalemia and cardiac dysrhythmias. | [17] |
| 34 | Eupatorium adenophorum Spreng. | Asteraceae | 2-deoxo-2-(acetyloxy)-9-oxoageraphorone, 9-oxo-10, 11-dehydroageraphorone, 10Hβ-9-oxoageraphorone, and 10Hα-9-oxo-ageraphorone | Ingestion of the plant may cause coughing, increased respiratory effort and weight loss in horses. | [69,70] |
| 35 | Gloriosa superba Linn. | Colchicaceae | Colchicine | Every part of this plant is poisonous, especially the tuberous rhizome, and after ingestion it may cause nausea, abdominal pain, vomiting, numbness, burning in the throat and bloody diarrhea, which leads to dehydration. | [121] |
| 36 | Heracleum canescens Lindl. | Apiaceae | Furanocoumarins | Skin contact with furanocoumarins caused sensitization when exposed to sunlight or UV light. Furanocoumarins enter to the nucleus and binds with DNA and causes cell death and inflammation. | [72] |
| 37 | Hedera nepalensis K.Koch | Araliaceae | Saponins | When the skin comes in contact with the leaves it causes skin problems such as rashes and severe swelling in susceptible individuals. Consumption of leaves is poisonous for animals, causing paralysis and finally death. | [14] |
| 38 | Hyoscyamus niger Linn. | Solanaceae | Tropane alkaloids | Ingestion causes dry mouth, dysphonia, tachycardia, dysphagia, mydriasis, headache, urinary retention and confusion. | [27] |
| 39 | Hypericum perforatum Linn. | Hypericaceae | Hypericin, pseudohypericin, and hyperforin | Plant intake during flowering phases causes itching, photosensitization and inflammation of affected areas of skin, dry cough, trembling of limbs, extreme body pains, cold sweat and intense fatigue are some other symptoms after ingestion. | [14] |
| 40 | Ichnocarpus frutescens (L.) W.T. Aiton | Apocynaceae | Not reported | Consumption of leaves by animals’ causes indigestion, sour belching, vomiting and stomach irritation. | [14] |
| 41 | Lantana camara Linn. | Verbenaceae | Lantadenes | Jaundice, diarrhea, weakness, lethargy, loss of appetite, photosensitivity and hepatotoxicity in grazing animals. | [77] |
| 42 | Melia azedarach Linn. | Meliaceae | Tetranortriterpenes (meliatoxins) | Neurotoxin, gastrointestinal. | [27,79] |
| 43 | Nerium indicum Mill. | Apocynaceae | Oleandrin | Consumption of this plant causes mild to severe symptoms such as increased blood pressure and heart rate, sweating and vomiting. Its excessive consumption leads to heart attack and sudden death. | [14] |
| 44 | Physalis minima Linn. | Solanaceae | Solanine | Consumption of unripe berries causes abortion in pregnant animals. | [14] |
| 45 | Prunus persica (L.) Batsch | Rosaceae | Cyanide | Excessive consumption of the newly developed leaves affects brains and causes severe symptoms, i.e., seizures, loss of consciousness, abdominal pain, convulsions, choking, and finally death within a few hours in animals. | [14] |
| 46 | Ranunculus arvensis Linn. | Ranunculaceae | Protoanemonin | This plant may cause skin inflammation and injury of mucous membranes. The fresh leaf juice causes cracks, itching and sores in the skin of humans and animals. | [14,122] |
| 47 | Ranunculus sceleratus Linn. | Ranunculaceae | Protoanemonin | When the skin or mucosa comes in contact with the injured part of the plant, it causes itching and skin rashes and blisters. Poison ingestion may cause dizziness, nausea, vomiting, acute hepatitis, jaundice and finally paralysis. | [123,124] |
| 48 | Rhamnus triquetra Wall. | Rhamnaceae | Rhamnetin, quercitin and rhamnazin | Fruits and leaves of this species are highly toxic for livestock and excessive consumption affects the working ability of their brain resulting in loss of mental balance. | [14] |
| 49 | Rhododendron campanulatum D.Don | Ericaceae | Andromedotoxin | After ingestion of flowering buds and leaves by livestock it causes salivation, diarrhea, loss of energy and finally death. | [84,85] |
| 50 | Ricinus communis Linn. | Euphorbiaceae | Ricin | In humans, it causes mild to severe symptoms after ingestion, i.e., pain in throat, inflammation in eyes, high fever, profuse cold sweat, difficulty in swallowing, vomiting, diarrhoea, nausea, weakness, trembling of hands, inability to stand and finally death. | [17] |
| 51 | Solanum xanthocarpum Schrad. & H. Wendl. | Solanaceae | Solasonine and solamargine | After ingestion it causes headaches, nausea, vomiting, diarrhea, stomach ache, burning of the throat, itching, eczema, thyroid problems and pain and inflammation in the joints. | [96] |
| 52 | Taxus baccata Linn. | Taxaceae | Taxanes or Taxines, Taxol | Seeds and leaves are highly toxic, causing nausea, vomiting, abdominal pain bradycardia and respiratory muscle paralysis. | [125] |
4. Role of Poisonous Plants to Cure Several Diseases
5. Conclusions and Future Prospective
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Husaini, D.C.; Bush, C.J.; Coc, I.; Guerra, E.; Perez, A.W.; Wu, C.-Y. Poisonous plants of Belize: A mini toxicological review. Adv. Tradit. Med. 2020, 1–11. [Google Scholar] [CrossRef]
- Benzeid, H.; Gouaz, F.; Touré, A.H.; Bouatia, M.; Idrissi, M.O.B.; Draoui, M. Inventory of toxic plants in Morocco: An overview of the botanical, biogeography, and phytochemistry studies. J. Toxicol. 2018, 2018, 4563735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.S.A.; Ahmad, I. Chapter 1—Herbal medicine: Current trends and future prospects. In New Look to Phytomedicine; Academic Press: Cambridge, MA, USA, 2019; pp. 3–13. [Google Scholar]
- Painuli, S.; Quispe, C.; Herrera-Bravo, J.; Semwal, P.; Martorell, M.; Almarhoon, Z.M.; Seilkhan, A.; Ydyrys, A.; Rad, J.S.; Alshehri, M.M. Nutraceutical Profiling, Bioactive Composition, and Biological Applications of Lepidium sativum L. Oxidative Med. Cell. Longev. 2022, 2022, 2910411. [Google Scholar] [CrossRef] [PubMed]
- Tewari, D.N. Report of the task force on conservation and sustainable use of medicinal plants. In Bulletin of Planning Commission; Government of India: New Delhi, India, 2000. [Google Scholar]
- Neupane, P.; Lamichhane, J. Estimation of total phenolic content, total flavonoid content and antioxidant capacities of five medicinal plants from Nepal. Vegetos 2020, 33, 360–366. [Google Scholar] [CrossRef]
- Semwal, P.; Painuli, S. Antioxidant, antimicrobial, and GC-MS profiling of Saussurea obvallata (Brahma Kamal) from Uttarakhand Himalaya. Clin. Phytosci. 2019, 5, 12. [Google Scholar] [CrossRef] [Green Version]
- Alonso-Amelot, M.E.; Oliveros, A.; Calcagno-Pisarelli, M.P. Phenolics and condensed tannins in relation to altitude in neotropical Pteridium spp.: A field study in the Venezuelan Andes. Biochem. Syst. Ecol. 2004, 32, 969–981. [Google Scholar] [CrossRef] [Green Version]
- Semwal, P.; Painuli, S.; Tewari, D.; Bussmann, R.W.; Palni, L.M.S.; Thapliyal, A. Assesment of non-timber Brahma Kamal (Saussurea obvallata (DC.) Edgew.), an important Himalayan. Ethnobot. Res. Appl. 2020, 19, 1–15. [Google Scholar]
- Zlatić, N.M.; Stanković, M.S. Variability of secondary metabolites of the species Cichorium intybus L. from different habitats. Plants 2017, 6, 38. [Google Scholar] [CrossRef] [Green Version]
- Semwal, P.; Painuli, S.; Painuli, K.M.; Antika, G.; Tumer, T.B.; Thapliyal, A.; Setzer, W.N.; Martorell, M.; Alshehri, M.M.; Taheri, Y. Diplazium esculentum (Retz.) Sw.: Ethnomedicinal, Phytochemical, and Pharmacological Overview of the Himalayan Ferns. Oxidative Med. Cell. Longev. 2021, 2021, 1917890. [Google Scholar] [CrossRef]
- Jamloki, A.; Bhattacharyya, M.; Nautiyal, M.; Patni, B. Elucidating the relevance of high temperature and elevated CO2 in plant secondary metabolites (PSMs) production. Heliyon 2021, 7, e07709. [Google Scholar] [CrossRef]
- Al-Qura’n, S. Ethnobotanical survey of folk toxic plants in southern part of Jordan. Toxicon 2005, 46, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, H.; Manhas, R.; Kumar, K.; Magotra, R. Traditional knowledge on poisonous plants of Udhampur district of Jammu and Kashmir, India. J. Ethnopharmacol. 2014, 152, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Mendieta, M.d.C.; Souza, A.D.Z.d.; Ceolin, S.; Vargas, N.R.C.; Ceolin, T.; Heck, R.M. Toxic plants: Importance of knowledge for realization of health education. J. Nurs. UFPE/Rev. Enferm. 2014, 8. [Google Scholar]
- Tamilselvan, N.; Thirumalai, T.; Shyamala, P.; David, E. A review on some poisonous plants and their medicinal values. J. Acute Dis. 2014, 3, 85–89. [Google Scholar] [CrossRef] [Green Version]
- Banasik, M.; Stedeford, T. Plants, Poisonous (Humans). In Encyclopedia of Toxicology, 3rd ed.; Wexler, P., Ed.; Academic Press: Oxford, UK, 2014; pp. 970–978. [Google Scholar] [CrossRef]
- Serrano, R. Toxic plants: Knowledge, medicinal uses and potential human health risks. Environ. Ecol. Res. 2018, 6, 487–492. [Google Scholar] [CrossRef] [Green Version]
- Habermehl, G.G. Highlights on Plant Toxins in Toxicon; Elsevier: Amsterdam, The Netherlands, 2004; Volume 44, pp. 341–344. [Google Scholar]
- Harvey, A.; Bradley, K.; Cochran, S.; Rowan, E.; Pratt, J.; Quillfeldt, J.; Jerusalinsky, D. What can toxins tell us for drug discovery? Toxicon 1998, 36, 1635–1640. [Google Scholar] [CrossRef]
- Katewa, S.; Galav, P.; Nag, A.; Jain, A. Poisonous plants of the southern Aravalli hills of Rajasthan. Indian J. Tradit. Knowl. 2008, 7, 269–272. [Google Scholar]
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014, 4, 177. [Google Scholar] [CrossRef] [Green Version]
- Petrovska, B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Coleman, J.J.; Ferner, R.E.; Evans, S.J.W. Monitoring for adverse drug reactions. Br. J. Clin. Pharmacol. 2006, 61, 371–378. [Google Scholar] [CrossRef]
- Casarett, L.J.; Klaassen, C.D.; Watkins, J.B. Casarett and Doull’s Essentials of Toxicology; McGraw-Hill/Medical Pub. Div.: New York, NY, USA, 2003. [Google Scholar]
- Huai, H.; Xu, J. Indigenous knowledge: An inexhaustible “information bank” for toxin research. Toxicon Off. J. Int. Soc. Toxinol. 2000, 38, 745–746. [Google Scholar] [CrossRef]
- Gupta, S.M.; Manikyaprabhu, K.; Dwibedi, S. Himalayan toxic plants of defense importance. Acta Sci. Med. Sci. 2018, 2, 44–48. [Google Scholar]
- Maharani, B.; Vijayakumari, N. Profile of poisoning cases in a Tertiary care Hospital, Tamil Nadu, India. J. Appl. Pharm. Sci. 2013, 3, 91. [Google Scholar] [CrossRef] [Green Version]
- Unnikrishnan, B.; Singh, B.; Rajeev, A. Trends of acute poisoning in south Karnataka. Kathmandu Univ. Med. J. (KUMJ) 2005, 3, 149–154. [Google Scholar]
- Haritha, C.; Khan, S.; Manjusha, K.; Banu, A. Toxicological aspects of common plant poisoning in ruminants. Indian Farmer 2019, 6, 812–822. [Google Scholar]
- Gupta, V.K.; Singh, G.D.; Singh, S.; Kaul, A. Medicinal Plants: Phytochemistry, Pharmacology and Therapeutics; Daya Publishing House: New Delhi, India, 2010; Volume 1. [Google Scholar]
- Bhatia, M.; Siddiqui, N.; Gupta, S. Abrus precatorius (L.): An evaluation of traditional herb. J. Pharm. Res. 2013, 3, 3296–3315. [Google Scholar]
- Narayanan, S.; Surendranath, K.; Bora, N.; Surolia, A.; Karande, A.A. Ribosome inactivating proteins and apoptosis. FEBS Lett. 2005, 579, 1324–1331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karthikeyan, A.; Amalnath, S.D. Abrus precatorius poisoning: A retrospective study of 112 patients. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2017, 21, 224. [Google Scholar] [CrossRef]
- Polunin, O.; Stainton, A. Flowers of the Himalaya; Oxford University Press: Oxford, UK, 1984. [Google Scholar]
- Ghimire, S.K.; Sapkota, I.; Oli, B.; Parajuli, R. Non-Timber Forest Products of Nepal Himalaya: Database of Some Important Species Found in the Mountain Protected Areas and Surrounding Regions; WWF Nepal; WWF: Gland, Switzerland, 2008; ISBN 978-99946-837-9-6. [Google Scholar]
- Agnihotri, P.; Husain, D.; Katiyar, P.; Husain, T. Notes on the typification of four Himalayan aconites. Kew Bull. 2016, 71, 1–7. [Google Scholar] [CrossRef]
- Hanuman, J.B.; Katz, A. Isolation and identification of four norditerpenoid alkaloids from processed and unprocessed root tubers of Aconitum ferox. J. Nat. Prod. 1993, 56, 801–809. [Google Scholar] [CrossRef]
- Hanuman, J.B.; Katz, A. Isolation of quinolinones from ayurvedic processed root tubers of Aconitum ferox. Nat. Prod. Lett. 1993, 3, 227–231. [Google Scholar] [CrossRef]
- Rokaya, M.B.; Münzbergová, Z.; Timsina, B. Ethnobotanical study of medicinal plants from the Humla district of western Nepal. J. Ethnopharmacol. 2010, 130, 485–504. [Google Scholar] [CrossRef] [PubMed]
- Regmi, P.; Ravikrishna, S.; Bhat, S.; Hebbar, C. Ethno-botanical and Toxicological comparison on varieties of Vatsanabha (Aconitum ferox Wall.) available in Nepal. Int. J. Ayurveda Tradit. Med. 2020, 2, 3–9. [Google Scholar]
- Kalita, B.C.; Gogoi, B.J.; Hui, P.K. Diversity and Traditional Uses of Some Poisonous Plants of Arunachal Pradesh. Int. J. Adv. Res. Innov. Ideas Educ. 2017, 3, 57–64. [Google Scholar]
- Sharma, E.; Gaur, A. Aconitum balfourii Stapf: A rare medicinal herb from Himalayan Alpine. J. Med. Plants Res. 2012, 6, 3810–3817. [Google Scholar] [CrossRef]
- Khetwal, K.; Joshi, B.; Desai, H.; William Pelletier, S. Alkaloids of Aconitum balfourii Stapf. Heterocycles 1992, 34, 441–444. [Google Scholar]
- Khetwal, K.; Pande, S. Constitutens of high altitude himalayan herbs part XV: A new norditerpenoid alkaloid from the roots of Aconitum balfourii. Nat. Prod. Res. 2004, 18, 129–133. [Google Scholar] [CrossRef]
- Khetwal, K.S.; Desai, H.; Joshi, B.S.; Pelletier, S.W. Norditerpenoid alkaloids from the aerial parts of Aconitum balfourii Stapf. Heterocycles 1994, 38, 833–842. [Google Scholar]
- Sher, H.; Jan, H.A.; Ur Rahman, I.; Hussain, W.; Kunwar, R.M.; Bussmann, R.W.; Paniagua-Zambrana, N.Y. Aconitum balfourii Stapf. Aconitum ferox Wall. ex. Ser. Aconitum heterophyllum Wall. ex Royle Aconitum laeve Royle Aconitum naviculare (Brühl) Stapf. Aconitum spicatum Stapf. Aconitum violaceum Jacq. ex Stapf var. violaceum Ranunculaceae. In Ethnobotany of the Himalayas; Kunwar, R.M., Sher, H., Bussmann, R.W., Eds.; Springer International Publishing: Cham, Switerland, 2021; pp. 139–154. [Google Scholar]
- Agnihotri, P.; Husain, D.; Husain, T. Assessment of diversity, endemism and distribution of the genus Aconitum Linnaeus (Ranunculaceae) in India. Pleione 2015, 9, 95–102. [Google Scholar]
- Gao, L.M.; Wei, X.M.; Yang, L.; Gao, L. Two new norditerpenoid alkaloids from Aconitum spicatum Stapf. Chin. Chem. Lett. 2005, 16, 475–478. [Google Scholar]
- Manandhar, N. Ethnobotany of Jumla District, Nepal. Int. J. Crude Drug Res. 1986, 24, 81–89. [Google Scholar] [CrossRef]
- Aziz, N.; Khan, M.N.; Ul Haq, F.; Ahmed, F.; Ali, A.; El-Seedi, H.R.; Musharraf, S.G. Erythroid induction activity of Aquilegia fragrans and Aquilegia pubiflora and identification of compounds using liquid chromatography-tandem mass spectrometry. J. King Saud Univ. Sci. 2021, 33, 101227. [Google Scholar] [CrossRef]
- Jan, H.; Usman, H.; Shah, M.; Zaman, G.; Mushtaq, S.; Drouet, S.; Hano, C.; Abbasi, B.H. Phytochemical analysis and versatile in vitro evaluation of antimicrobial, cytotoxic and enzyme inhibition potential of different extracts of traditionally used Aquilegia pubiflora Wall. Ex Royle. BMC Complement. Med. Ther. 2021, 21, 1–19. [Google Scholar] [CrossRef]
- Kaur, L.; Joseph, L.; George, M. Phytochemical analysis of leaf extract of Aesculus indica. Int. J. Pharm. Pharm. Sci. 2011, 3, 232–234. [Google Scholar]
- Yadav, N.; Singh, A.P.; Rana, A.C.; Kumar, S.; Kaur, P.; Singh, J.; Jangra, A.; Kumar, D. Aesculus indica: An updated review on its pharmacognosy, phytochemistry and pharmacological profile. Egypt. J. Basic Appl. Sci. 2022, 9, 125–135. [Google Scholar] [CrossRef]
- Plants of the World Online, w.p.o. Available online: www.plantoftheworldonline.org (accessed on 22 May 2022).
- Zhang, Q.; Chen, X.; Guo, H.; Trindade, L.M.; Salentijn, E.M.J.; Guo, R.; Guo, M.; Xu, Y.; Yang, M. Latitudinal Adaptation and Genetic Insights Into the Origins of Cannabis sativa L. Front. Plant Sci. 2018, 9, 1876. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breijyeh, Z.; Jubeh, B.; Bufo, S.A.; Karaman, R.; Scrano, L. Cannabis: A toxin-producing plant with potential therapeutic uses. Toxins 2021, 13, 117. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, K.J.; Fine, D.M.; Evans, T.J.; Khan, S. Suspected lily-of-the-valley (Convallaria majalis) toxicosis in a dog. J. Vet. Emerg. Crit. Care 2008, 18, 399–403. [Google Scholar] [CrossRef]
- Cortinovis, C.; Caloni, F. Epidemiology of intoxication of domestic animals by plants in Europe. Vet. J. 2013, 197, 163–168. [Google Scholar] [CrossRef]
- Knight, A. A Guide to Poisonous House and Garden Plants; CRC Press: Boca Raton, FL, USA, 2007. [Google Scholar]
- Fenton, J.J. Toxicology: A Case-Oriented Approach; CRC Press: Boca Raton, FL, USA, 2001. [Google Scholar]
- Khare, C.P. Delphinium brunonianum Royle. In Indian Medicinal Plants: An Illustrated Dictionary; Khare, C.P., Ed.; Springer: New York, NY, USA, 2007. [Google Scholar]
- Zoltani, C.K. Chapter 14—Cardiovascular Toxicity. In Veterinary Toxicology, 3rd ed.; Gupta, R.C., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 227–238. [Google Scholar]
- Zoltani, C.K. Cardiovascular toxicity. In Veterinary Toxicology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 227–238. [Google Scholar]
- Chen, H.; Zhou, B.; Yang, J.; Ma, X.; Deng, S.; Huang, Y.; Wen, Y.; Yuan, J.; Yang, X. Essential oil derived from Eupatorium adenophorum spreng. Mediates anticancer effect by inhibiting stat3 and akt activation to induce apoptosis in hepatocellular carcinoma. Front. Pharmacol. 2018, 9, 483. [Google Scholar] [CrossRef]
- O’sullivan, B. Investigations into Crofton weed (Eupatorium adenophorum) toxicity in horses. Aust. Vet. J. 1985, 62, 30–32. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Mukhopadhayay, S.; Tolenkhomba, T.; Shah, A. Short-term toxicity studies of Eupatorium adenophorum in Swiss albino mice. Int. J. Res. Phytochem. Pharmacol. 2011, 1, 165–171. [Google Scholar]
- Liu, B.; Cao, L.; Zhang, L.; Yuan, X.; Zhao, B. Hepatotoxicity of Eupatorium adenophorum extracts and the identification of major hepatotoxic components. Nat. Prod. Res. 2017, 31, 2788–2792. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Singh, A.; Sharma, O.P.; Dawra, R.K.; Kurade, N.P.; Mahato, S.B. Hepatotoxicity and cholestasis in rats induced by the sesquiterpene, 9-oxo-10, 11-dehydroageraphorone, isolated from Eupatorium adenophorum. J. Biochem. Mol. Toxicol. 2001, 15, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Oelrichs, P.B.; Calanasan, C.A.; Macleod, J.K.; Seawright, A.A.; Ng, J.C. Isolation of a compound from Eupatorium adenophorum (Spreng.) [Ageratina adenophora (Spreng.)] causing hepatotoxicity in mice. Nat. Toxins 1995, 3, 350–354. [Google Scholar] [CrossRef]
- Ouyang, C.B.; Liu, X.M.; Liu, Q.; Bai, J.; Li, H.Y.; Li, Y.; Wang, Q.X.; Yan, D.D.; Mao, L.G.; Cao, A. Toxicity assessment of cadinene sesquiterpenes from Eupatorium adenophorum in mice. Nat. Prod. Bioprospecting 2015, 5, 29–36. [Google Scholar] [CrossRef] [Green Version]
- Del Río, J.A.; Díaz, L.; García-Bernal, D.; Blanquer, M.; Ortuno, A.; Correal, E.; Moraleda, J.M. Furanocoumarins: Biomolecules of therapeutic interest. Stud. Nat. Prod. Chem. 2014, 43, 145–195. [Google Scholar]
- Al-Snafi, A.E. Therapeutic importance of Hyoscyamus species grown in Iraq (Hyoscyamus albus, Hyoscyamus niger and Hyoscyamus reticulates)—A review. IOSR J. Pharm. 2018, 8, 18–32. [Google Scholar]
- Bock, J.; Norris, D. Introduction to Forensic Plant Science; Academic Press: London, UK, 2016; Volume 2016, pp. 1–22. [Google Scholar]
- Nayar, M. Changing patterns of the Indian flora. Nelumbo-Bull. Bot. Surv. India 1977, 19, 145–155. [Google Scholar]
- Kohli, R.K.; Batish, D.R.; Singh, H.; Dogra, K.S. Status, invasiveness and environmental threats of three tropical American invasive weeds (Parthenium hysterophorus L., Ageratum conyzoides L., Lantana camara L.) in India. Biol. Invasions 2006, 8, 1501–1510. [Google Scholar] [CrossRef]
- Negi, G.; Sharma, S.; Vishvakarma, S.C.; Samant, S.S.; Maikhuri, R.K.; Prasad, R.C.; Palni, L. Ecology and use of Lantana camara in India. Bot. Rev. 2019, 85, 109–130. [Google Scholar] [CrossRef] [Green Version]
- Parimoo, H.A.; Sharma, R.; Patil, R.D.; Patial, V. Sub-acute toxicity of lantadenes isolated from Lantana camara leaves in Guinea pig animal model. Comp. Clin. Pathol. 2015, 24, 1541–1552. [Google Scholar] [CrossRef]
- Oelrichs, P.B.; Hill, M.W.; Vallely, P.J.; MacLeod, J.K.; Molinski, T.F. Toxic tetranortriterpenes of the fruit of Melia azedarach. Phytochemistry 1983, 22, 531–534. [Google Scholar] [CrossRef]
- Carmen Méndez, M.d.; Aragão, M.; Fabiana, E.; Riet-Correa, F.; Juan Gimeno, E. Experimental intoxication by the leaves of Melia azedarach (Meliaceae) in cattle. Pesqui. Veterinária Bras. 2002, 22, 19–24. [Google Scholar] [CrossRef]
- Plumlee, K.H. Chapter 25—Plants. In Clinical Veterinary Toxicology; Plumlee, K.H., Ed.; Mosby: Saint Louis, MI, USA, 2004; pp. 337–442. [Google Scholar] [CrossRef]
- Phua, D.H.; Tsai, W.J.; Ger, J.; Deng, J.F.; Yang, C.C. Human Melia azedarach poisoning. Clin. Toxicol. 2008, 46, 1067–1070. [Google Scholar] [CrossRef]
- Poudel, R.C.; Kunwar, R.M.; Jan, H.A.; Sher, H.; Ur Rahman, I.; Hussain, W.; Bussmann, R.W.; Paniagua-Zambrana, N.Y. Rhododendron afghanicum Aitch. & Hemsl. Rhododendron anthopogon D. Don Rhododendron arboreum Sm. Rhododendron campanulatum D. Don Rhododendron collettianum Aitch. & Hemsl. Ericaceae. In Ethnobotany of the Himalayas; Kunwar, R.M., Sher, H., Bussmann, R.W., Eds.; Springer International Publishing: Cham, Switerland, 2020; pp. 1–18. [Google Scholar]
- Rai, I.D.; Singh, G.; Rawat, G. Plants of Kedarnath Wildlife Sanctuary, Western Himalaya: A Field Guide; Bishen Singh Mahendra Pal Singh: Dehradun, India, 2017. [Google Scholar]
- Bhattacharyya, D. Rhododendron species and their uses with special reference to Himalayas—A review. Assam Univ. J. Sci. Technol. 2011, 7, 161–167. [Google Scholar]
- Kerkvliet, J. Analysis of a toxic rhododendron honey. J. Apic. Res. 1981, 20, 249–253. [Google Scholar] [CrossRef]
- Hikino, H.; Ohta, T.; Ogura, M.; Ohizumi, Y.; Konno, C.; Takemoto, T. Structure-activity relationship of ericaceous. Toxins on acute toxicity in mice. Toxicol. Appl. Pharmacol. 1976, 35, 303–310. [Google Scholar] [CrossRef]
- Smith, M. Japanese pieris poisoning in the goat. J. Am. Vet. Med. Assoc. 1978, 173, 78–79. [Google Scholar]
- Krochmal, C. Poison honeys. Am. Bee J. 1994, 134, 549–550. [Google Scholar]
- Zarai, Z.; Chobba, I.B.; Mansour, R.B.; Békir, A.; Gharsallah, N.; Kadri, A. Essential oil of the leaves of Ricinus communis L.: In vitro cytotoxicity and antimicrobial properties. Lipids Health Dis. 2012, 11, 102. [Google Scholar] [CrossRef] [Green Version]
- Phillips, R.R. Annuals and Biennials: The Garden Plants; Macmillan: London, UK, 1999. [Google Scholar]
- Buzzz, G. Nine Most Toxic Plants for Humans. Available online: http://greenbuzzznet/environment/ninemost-toxic-plants-for-humans/ (accessed on 20 May 2022).
- Kobert, R. der Intoxikationen; Ferdinand Enke: Stuttgart, Germany, 1906. [Google Scholar]
- Stillmark, H. Ueber Ricin, ein Giftiges Fragment aus den Samen von Ricinus comm. L. und Einigen Anderen Euphorbiaceen; Kaiserliche Universität zu Dorpat: Tartu, Estonia, 1888. [Google Scholar]
- Smallshaw, J.E.; Firan, A.; Fulmer, J.R.; Ruback, S.L.; Ghetie, V.; Vitetta, E.S. A novel recombinant vaccine which protects mice against ricin intoxication. Vaccine 2002, 20, 3422–3427. [Google Scholar] [CrossRef]
- Siddiqui, B.; Siddiqui, S.; Faizi, S. Studies in the Chemical Constituents of the Fresh Berries of Solanum xanthocarpum Schrad. and Wendle. J. Chem. Soc. Pak. 2011, 5, 99. [Google Scholar]
- Al Sinani, S.; Eltayeb, E. The steroidal glycoalkaloids solamargine and solasonine in Solanum plants. S. Afr. J. Bot. 2017, 112, 253–269. [Google Scholar] [CrossRef]
- Al Chami, L.; Méndez, R.; Chataing, B.; O’Callaghan, J.; Usubillaga, A.; LaCruz, L. Toxicological effects of alpha-solamargine in experimental animals. Phytother. Res. 2003, 17, 254–258. [Google Scholar] [CrossRef]
- Wilson, C.R.; Sauer, J.; Hooser, S.B. Taxines: A review of the mechanism and toxicity of yew (Taxus spp.) alkaloids. Toxicon 2001, 39, 175–185. [Google Scholar] [CrossRef]
- Tiwary, A.K.; Puschner, B.; Kinde, H.; Tor, E.R. Diagnosis of Taxus (yew) poisoning in a horse. J. Vet. Diagn. Investig. 2005, 17, 252–255. [Google Scholar] [CrossRef] [Green Version]
- Tekol, Y. Acute toxicity of taxine in mice and rats. Vet. Hum. Toxicol 1991, 33, 337–338. [Google Scholar]
- Alden, C.L.; Fosnaugh, C.J.; Smith, J.B.; Mohan, R. Japanese yew poisoning of large domestic animals in the Midwest. J. Am. Vet. Med. Assoc. 1977, 170, 314–316. [Google Scholar]
- Bahmani, M.; Shirzad, H.; Rafieian, S.; Rafieian-Kopaei, M. Silybum marianum: Beyond Hepatoprotection. J. Evid.-Based Complement. Altern. Med. 2015, 20, 292–301. [Google Scholar] [CrossRef] [Green Version]
- Sewell, R.D.; Rafieian-Kopaei, M. The history and ups and downs of herbal medicines usage. J. HerbMed Pharmacol. 2014, 3, 1–3. [Google Scholar]
- Tucker, J.; Cordy, D.; Berry, L.; Harvey, W.; Fuller, T. Nitrate Poisoning in Livestock; Nitrate Poisoning Livest California Agricultural Experiment Station Circular: Berkeley, CA, USA, 1961. [Google Scholar]
- Ameri, A. The effects of Aconitum alkaloids on the central nervous system. Prog. Neurobiol. 1998, 56, 211–235. [Google Scholar] [CrossRef]
- Shaheen, F.; Ahmad, M.; Khan, M.T.H.; Jalil, S.; Ejaz, A.; Sultankhodjaev, M.N.; Arfan, M.; Choudhary, M.I. Alkaloids of Aconitum laeve and their anti-inflammatory, antioxidant and tyrosinase inhibition activities. Phytochemistry 2005, 66, 935–940. [Google Scholar] [CrossRef]
- Ulubelen, A.; Mericli, A.; Mericli, F.; Kolak, U.; Arfan, M.; Ahmad, M.; Ahmad, H. Norditerpenoid alkaloids from the roots of Aconitum leave Royle. Pharmazie 2002, 57, 427–429. [Google Scholar]
- Diallo, A.; Eklu-Gadegbeku, K.; Amegbor, K.; Agbonon, A.; Aklikokou, K.; Creppy, E.; Gbeassor, M. In vivo and in vitro toxicological evaluation of the hydroalcoholic leaf extract of Ageratum conyzoides L. (Asteraceae). J. Ethnopharmacol. 2014, 155, 1214–1218. [Google Scholar] [CrossRef]
- Kotb, F.T. Medicinal Plants in Libya; Arab Encyclopedia House: Beirut, Lebanon, 1985; p. 830. [Google Scholar]
- Tilford, G.L. Edible and Medicinal Plants of the West; Mountain Press Publishing: Missoula, MT, USA, 1997. [Google Scholar]
- Shelar, M.; Bafna, A.; Wahile, A.; Tupkari, S. Evaluation of edible oils for Argemone mexicana seed oil adulteration. Res. J. Pharm. Biol. Chem. Sci. 2011, 2, 927–936. [Google Scholar]
- Ali, H.; Yaqoob, U. Traditional uses, phytochemistry, pharmacology and toxicity of Arisaema (Areaceae): A review. Bull. Natl. Res. Cent. 2021, 45, 1–19. [Google Scholar] [CrossRef]
- da Silva, J.A.T. Mining the essential oils of the Anthemideae. Afr. J. Biotechnol. 2004, 3, 706–720. [Google Scholar]
- Iyadurai, R.; Gunasekaran, K.; Jose, A.; Pitchaimuthu, K. Calotropis poisoning with severe cardiac toxicity—A case report. J. Fam. Med. Prim. Care 2020, 9, 4444. [Google Scholar] [CrossRef]
- Plants, N. Plant Database. Agalinis purpurea, A. setacea, A. strictifolia, A. heterophylla, Perideridia americana, Osmorhiza longistylis, Taenidia integerrima. 2014. Available online: https://www.wildflower.org/plants/result.php?id_plant=SOSE3 (accessed on 22 May 2022).
- Liakh, V.; Konechna, R.; Mylyanych, A.; Zhurakhivska, L.; Hubytska, I.; Novikov, V. Caltha palustris. Analytical overview. Sci. Pharm. Sci. 2020, 2020, 51–56. [Google Scholar] [CrossRef]
- Alves, A. Pharmacological study of the root of Cassia occidentalis. Anals Fac Farm. Porto 1965, 24, 65–119. [Google Scholar]
- Vashishtha, V.; Nayak, N.; Jacob John, T.; Kumar, A. Recurrent annual outbreaks of a hepato-myo-encephalopathy syndrome in children in western Uttar Pradesh, India. Indian J. Med. Res. 2007, 125, 523–533. [Google Scholar] [PubMed]
- Moxley, R.; Schneider, N.; Steinegger, D.; Carlson, M. Apparent toxicosis associated with lily-of-the-valley (Convallaria majalis) ingestion in a dog. J. Am. Vet. Med. Assoc. 1989, 195, 485–487. [Google Scholar]
- George, P. Death related to herbal therapy for joint pains–A rare case of Gloriosa superba poisoning. J. Clin. Diagn. Res. 2011, 5, 379–380. [Google Scholar]
- Sedivy, C.; Piskorski, R.; Müller, A.; Dorn, S. Too low to kill: Concentration of the secondary metabolite ranunculin in buttercup pollen does not affect bee larval survival. J. Chem. Ecol. 2012, 38, 996–1002. [Google Scholar] [CrossRef] [Green Version]
- Lewis, R.A. Lewis’ Dictionary of Toxicology; CRC Press: Boca Raton, FL, USA, 1998. [Google Scholar]
- Yilmaz, B.; Yilmaz, B.; Aktaş, B.; Unlu, O.; Roach, E.C. Lesser celandine (pilewort) induced acute toxic liver injury: The first case report worldwide. World J. Hepatol. 2015, 7, 285. [Google Scholar] [CrossRef]
- Willaert, W.; Claessens, P.; Vankelecom, B.; Vanderheyden, M. Intoxication with Taxus baccata: Cardiac arrhythmias following yew leaves ingestion. Pacing Clin. Electrophysiol. 2002, 25, 511–512. [Google Scholar] [CrossRef] [PubMed]
- Tekuri, S.K.; Pasupuleti, S.K.; Konidala, K.K.; Amuru, S.R.; Bassaiahgari, P.; Pabbaraju, N. Phytochemical and pharmacological activities of Solanum surattense Burm. f.-A review. J. Appl. Pharm. Sci. 2019, 9, 126–136. [Google Scholar]
- Botha, C.; Penrith, M.L. Poisonous plants of veterinary and human importance in southern Africa. J. Ethnopharmacol. 2008, 119, 549–558. [Google Scholar] [CrossRef]
- Bisht, V.; Negi, J.; Bh, A.; Sundriyal, R. Traditional use of medicinal plants in district Chamoli, Uttarakhand, India. J. Med. Plants Res. 2013, 7, 918–929. [Google Scholar]
- Joshi, R. Traditional healthcare practices among the villages of Khirshu, Pauri, Uttarakhand, India. Soc. Sci. Rev. 2016, 2, 105–116. [Google Scholar]
- Kumar, A.; Mitra, M.; Adhikari, B.; Rawat, G. Depleting indigenous knowledge of medicinal plants in cold-arid region of Nanda Devi Biosphere Reserve, Western Himalaya. Med. Aromat. Plants 2015, 4, 2167–2178. [Google Scholar] [CrossRef]
- Phondani, P.; Maikhuri, R.; Kala, C. Ethnoveterinary uses of medicinal plants among traditional herbal healers in Alaknanda catchment of Uttarakhand, India. Afr. J. Tradit. Complement. Altern. Med. 2010, 7, 195–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rawat, G.S. Alpine Meadows of Uttaranchal: Ecology, Land Use and Status of Medicinal and Aromatic Plants; Bishen Pal Singh Mahendra Pal Singh: Dehradun, India, 2005; p. 219. [Google Scholar]
- Uniyal, B. Utilization of Medicinal Plants by the Rural women of Kullu, Himachal Pradesh. NIScPR 2003, 2, 366–370. [Google Scholar]
- Gairola, S.; Sharma, J.; Bedi, Y.S. A cross-cultural analysis of Jammu, Kashmir and Ladakh (India) medicinal plant use. J. Ethnopharmacol. 2014, 155, 925–986. [Google Scholar] [CrossRef] [PubMed]
- Kayani, S.; Ahmad, M.; Sultana, S.; Shinwari, Z.K.; Zafar, M.; Yaseen, G.; Hussain, M.; Bibi, T. Ethnobotany of medicinal plants among the communities of Alpine and Sub-alpine regions of Pakistan. J. Ethnopharmacol. 2015, 164, 186–202. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Lama, Y.; Tripathi, G.; Schmitt, S.; Aumeeruddy-Thomas, Y. Conservation of Plant Resources, Community Development and Training in Applied Ethnobotany at Shey-Phoksundo National Park and Its Buffer Zone, Dolpa; WWF Report Series Nepal Program, Kathmandu, Nepal; WWF: Gland, Switzerland, 2001; p. 41. [Google Scholar]
- Kunwar, R.M.; Adhikari, N. Ethnomedicine of Dolpa district, Nepal: The plants, their vernacular names and uses. Lyonia 2005, 8, 43–49. [Google Scholar]
- Tiwari, U.L.; Kotia, A.; Rawat, G.S. Medico-ethnobotany of the Monpas in Tawang and West Kameng districts of Arunachal Pradesh, India. Pleione 2009, 3, 1–8. [Google Scholar]
- Tsering, J.; Tag, H. High altitude ethnomedicinal plants of Western Arunachal Himalayan landscape. Pleione 2015, 9, 18–25. [Google Scholar]
- Singh, H.B.; Sundriyal, R. Composition, economic use, and nutrient contents of alpine vegetation in the Khangchendzonga Biosphere Reserve, Sikkim Himalaya, India. Arct. Antarct. Alp. Res. 2005, 37, 591–601. [Google Scholar] [CrossRef] [Green Version]
- Quattrocchi, U. CRC World Dictionary of Medicinal and Poisonous Plants: Common Names, Scientific Names, Eponyms, Synonyms, and Etymology (5 Volume Set); CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Srivastava, N.; Sharma, V.; Kamal, B.; Dobriyal, A.; Jadon, V.S. Advancement in research on Aconitum sp.(Ranunculaceae) under different area: A review. Biotechnology 2010, 9, 411–427. [Google Scholar] [CrossRef] [Green Version]
- Hussain, I.; Bano, A.; Ullah, F. Traditional drug therapies from various medicinal plants of central karakoram national park, Gilgit-Baltistan Pakistan. Pak. J. Bot. 2011, 43, 79–84. [Google Scholar]
- Jamil Ahmed, M.; Murtaza, G. A study of medicinal plants used as ethnoveterinary: Harnessing potential phytotherapy in Bheri, District Muzaffarabad (Pakistan). J. Ethnopharmacol. 2015, 159, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Thatoi, P.; Kerry, R.G.; Gouda, S.; Das, G.; Pramanik, K.; Thatoi, H.; Patra, J.K. Photo-mediated green synthesis of silver and zinc oxide nanoparticles using aqueous extracts of two mangrove plant species, Heritiera fomes and Sonneratia apetala and investigation of their biomedical applications. J. Photochem. Photobiol. B Biol. 2016, 163, 311–318. [Google Scholar] [CrossRef]
- Gangwar, K.; Deepali, G.R.; Gangwar, R. Ethnomedicinal plant diversity in Kumaun himalaya of Uttarakhand, India. Nat. Sci. 2010, 8, 66–78. [Google Scholar]
- Hussain, F.; Badshah, L.; Dastagir, G. Folk medicinal uses of some plants of South Waziristan, Pakistan. Pak. J. Plant Sci. 2006, 12, 27–39. [Google Scholar]
- Jain, A.; Katewa, S.; Galav, P. Some phytotherapeutic claims by tribals of southern Rajasthan. Indian J. Tradit. Knowl. 2005, 4, 291–297. [Google Scholar]
- Suresh, K.; Kottaimuthu, R.; Norman, T.S.J.; Kumuthakalavalli, R.; Simon, S.M. Ethnobotanical study of medicinal plants used by Malayali tribals in Kolli Hills of Tamil Nadu, India. Int. J. Res. Ayurveda Pharm. 2011, 2, 502–508. [Google Scholar]
- Verma, H.; Lal, V.; Pant, K.; Soni, N. A Ethno medicinal Review on Arisaema tortuosum. Int. J. Adv. Pharm. Biol. Chem. 2012, 1, 176–179. [Google Scholar]
- Schultes, R.E.; Hofmann, A. Plants of the Gods: Origins of Hallucinogenic Use; Alfred van der Marck Editions: New York, NY, USA, 1979. [Google Scholar]
- Tombs, S.; Silverman, I. Pupillometry: A sexual selection approach. Evol. Hum. Behav. 2004, 25, 221–228. [Google Scholar] [CrossRef]
- Alsasua del Valle, A. Implication of cannabinoids in neurological diseases. Cell Mol. Neurobiol. 2006, 26, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Levendal, R.A.; Frost, C. In vivo effects of Cannabis sativa L. extract on blood coagulation, fat and glucose metabolism in normal and streptozocin-induced diabetic rats. Afr. J. Tradit. Complement. Altern. Med. 2006, 3, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Swift, W.; Gates, P.; Dillon, P. Survey of Australians using cannabis for medical purposes. Harm Reduct. J. 2005, 2, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stansbury, J.; Saunders, P.; Winston, D.; Zampieron, E. The Use of Convallaria and Crataegus in the Treatment of Cardiac Dysfunction. J. Restor. Med. 2012, 1, 107–111. [Google Scholar] [CrossRef] [Green Version]
- Tripathee, H.P.; Sharma, R.P.; Timilsina, Y.P.; Pathak, R.; Devkota, K.P. An assessment of ethnomedicinal use, chemical constituents analysis and bioactivity evaluation on high altitude medicinal plant Delphinium brunonianum of Manang district. Nepal J. Sci. Technol. 2011, 12, 111–118. [Google Scholar] [CrossRef] [Green Version]
- Gilani, A.H.; Khan, A.u.; Raoof, M.; Ghayur, M.N.; Siddiqui, B.S.; Vohra, W.; Begum, S. Gastrointestinal, selective airways and urinary bladder relaxant effects of Hyoscyamus niger are mediated through dual blockade of muscarinic receptors and Ca2+ channels. Fundam. Clin. Pharmacol. 2008, 22, 87–99. [Google Scholar] [CrossRef]
- Ghorbanpour, M.; Ghafarzadegan, R.; Khavazi, K.; Hatami, M. Two main tropane alkaloids variations of black henbane (Hyoscyamus niger) under PGPRs inoculation and water deficit stress induction at flowering stage. J. Med. Plants 2013, 12, 29–42. [Google Scholar]
- Dharani, N.; Rukunga, G.; Yenesew, A.; Mbora, A.; Mwaura, L.; Dawson, I.; Jamnadass, R. Common antimalarial trees and shrubs of East Africa. A Descr. Species A Guide Cultiv. Conserv. Use 2010, 73–76. [Google Scholar]
- Rahmatullah, M.; Khatun, M.A.; Morshed, N.; Neogi, P.K.; Khan, S.U.A.; Hossan, M.S.; Mahal, M.J.; Jahan, R. A randomized survey of medicinal plants used by folk medicinal healers of Sylhet Division, Bangladesh. Adv. Nat. Appl. Sci. 2010, 4, 52–62. [Google Scholar]
- Post-White, J.; Ladas, E.J.; Kelly, K.M. Advances in the use of milk thistle (Silybum marianum). Integr. Cancer Ther. 2007, 6, 104–109. [Google Scholar] [CrossRef]
- Malik, S.; Cusidó, R.M.; Mirjalili, M.H.; Moyano, E.; Palazón, J.; Bonfill, M. Production of the anticancer drug taxol in Taxus baccata suspension cultures: A review. Process Biochem. 2011, 46, 23–34. [Google Scholar] [CrossRef]




| S. No. | Poisonous Plants | Medicinal Properties | References |
|---|---|---|---|
| 1 | Abrus precatorius Linn. | Traditionally used to treat tetanus and to prevent rabies. | [32] |
| 2 | Aconitum lethale Griff. | Used to cure leprosy and arthritis, fever, rheumatism and boils. | [128,129,130,131,132,133] |
| 3 | Aconitum chasmanthum Stapf ex Holmes | Used in neuralgia, beurological rheumatism, as anthelminthic and as body tonic. | [134,135] |
| 4 | Aconitum ferox Wall. ex Ser. | Fever, digestive problems, leprosy, cholera inflammation and cuts, after detoxification of dried tubers by boiling in alcohol and used for fever, throat pain, tonsillitis, stomach ache and cheilitis. | [136,137,138,139] |
| 5 | Aconitum hookeri Stapf | Dried roots are used in diabetes and jaundice. | [140] |
| 6 | Aconitum laeve Royle | Used in kidney problems such as kidney stones, cold, cough, vomiting and diarrhea. | [141,142] |
| 7 | Aquilegia pubiflora Wall. ex Royle | Traditionally used in hepatitis, jaundice, wound healing, skin burns, circulatory and cardiovascular diseases. | [143,144,145] |
| 8 | Arisaema triphyllum (L.) Schott | Used in stomach ache and rheumatism, piles, dysentery. Tubers’ powder are used for the treatment of wound healing. | [146,147,148,149,150] |
| 9 | Atropa belladonna Linn. | Used to dilate the pupil of the eye, headache, peptic ulcer, menstrual symptoms, inflammation and motion sicknesss. | [151,152] |
| 10 | Cannabis sativa Linn. | Used for the treatment of various diseases, i.e., nausea, vomiting, diabetes, glaucoma, snake-bite, chronic pain, arthritis, bronchial asthma and cancer. | [153,154,155] |
| 11 | Convallaria majalis Linn. | Used in congestive heart failure and cardiomyopath | [156] |
| 12 | Delphinium brunonianum Royle | The dry and powdered rhizome is used in fever, headache stomach-ache, and cough. | [157] |
| 13 | Hyoscyamus niger Linn. | Used for the treatment for pupil dilating, urinary bladder relaxant, antisecretory, bronchodilating, anti-diarrheal properties, and as a spasmolytic, hypnotic hallucinogenic and sedative. | [158,159] |
| 14 | Melia azedarach Linn. | Stem and bark are used in gonorrhea, malaria and to expel parasitic worms, leaves are used for skin diseases such as scabies and for brushing teeth. | [160,161] |
| 15 | Silybum marianum (L.) Gaertn. | Used to treat liver and biliary disorders. | [162] |
| 16 | Taxus baccata Linn. | The taxol has high anticancer properties and used for cancer treatment. | [163] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jamloki, A.; Trivedi, V.L.; Nautiyal, M.C.; Semwal, P.; Cruz-Martins, N. Poisonous Plants of the Indian Himalaya: An Overview. Metabolites 2022, 12, 540. https://doi.org/10.3390/metabo12060540
Jamloki A, Trivedi VL, Nautiyal MC, Semwal P, Cruz-Martins N. Poisonous Plants of the Indian Himalaya: An Overview. Metabolites. 2022; 12(6):540. https://doi.org/10.3390/metabo12060540
Chicago/Turabian StyleJamloki, Abhishek, Vijay Laxmi Trivedi, M. C. Nautiyal, Prabhakar Semwal, and Natália Cruz-Martins. 2022. "Poisonous Plants of the Indian Himalaya: An Overview" Metabolites 12, no. 6: 540. https://doi.org/10.3390/metabo12060540