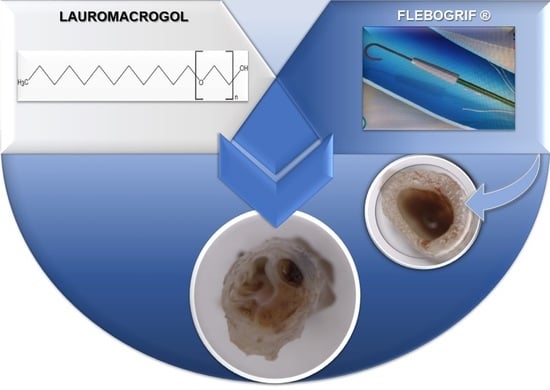
Study of Flebogrif®—A New Tool for Mechanical Sclerotherapy—Effectiveness Assessment Based on Animal Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Analysis of Physicochemical Properties of Lauromacrogol
2.2. The Course of the Experiment
2.3. Histological Evaluation
3. Results
3.1. The Analysis of Physicochemical Properties of Lauromacrogol
3.2. Histological Results
3.3. The Morphometrical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mitchel, P.; Goldman, J.-J. 7—Mechanism of Action of Sclerotherapy. In Sclerotherapy; Elsevier: Amsterdam, The Netherlands, 2017; Volume 6, pp. 173–199. [Google Scholar]
- Zimmet, S.E. Sclerotherapy Treatment of Telangiectasias and Varicose Veins. Tech. Vasc. Interv. Radiol. 2003, 6, 116–120. [Google Scholar] [CrossRef]
- Jensen, J.T.; Rodriguez, M.I.; Liechtenstein-Zábrák, J.; Zalanyi, S. Transcervical polidocanol as a nonsurgical method of female sterilization: A pilot study. Contraception 2004, 70, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Hawro, T.; Fluhr, J.W.; Mengeaud, V.; Redoulès, D.; Church, M.K.; Maurer, M.; Metz, M. Polidocanol inhibits cowhage—But not histamine-induced itch in humans. Exp. Dermatol. 2014, 23, 922–923. [Google Scholar] [CrossRef]
- Schweiger, D.; Baufeld, C.; Drescher, P.; Oltrogge, B.; Höpfner, S.; Mess, A.; Lüttke, J.; Rippke, F.; Filbry, A.; Max, H. Efficacy of a new tonic containing urea, lactate, polidocanol, and glycyrrhiza inflata root extract in the treatment of a dry, itchy, and subclinically inflamed scalp. Skin Pharmacol. Physiol. 2013, 26, 108–118. [Google Scholar] [CrossRef] [PubMed]
- Drake, L.A.; Dinehart, S.M.; Goltz, R.W.; Graham, G.F.; Hordinsky, M.K.; Lewis, C.W.; Pariser, D.M.; Skouge, J.W.; Webster, S.B.; Whitaker, D.C.; et al. Guidelines of care for sclerotherapy treatment of varicose and telangiectatic leg veins. J. Am. Acad. Dermatol. 1996, 34, 523–528. [Google Scholar]
- Hamel-Desnos, C.; Ouvry, P.; Benigni, J.P.; Boitelle, G.; Schadeck, M.; Desnos, P.; Allaert, F.A. Comparison of 1% and 3% Polidocanol Foam in Ultrasound Guided Sclerotherapy of the Great Saphenous Vein: A Randomised, Double-Blind Trial with 2 Year-Follow-up. “The 3/1 Study.”. Eur. J. Vasc. Endovasc. Surg. 2007, 34, 723–729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabe, E.; Pannier-Fischer, F.; Gerlach, H.; Breu, F.X.; Guggenbichler, S.; Zabel, M. Guidelines for sclerotherapy of varicose veins. Phlebologie 2003, 32, 101–106. [Google Scholar]
- Chen, C.H.; Chiu, C.S.; Yang, C.H. Ultrasound-guided foam sclerotherapy for treating incompetent great saphenous veins—Results of 5 years of analysis and morphologic evolvement study. Dermatol. Surg. 2012, 38, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, A.; Kakkos, S.; Baekgaard, N.; Comerota, A.; de Maeseneer, M.; Eklof, B.; Giannoukas, A.; Lugli, M.; Maleti, O.; Mansilha, A.; et al. Management of chronic venous disorders of the lower limbs. Guidelines According to Scientific Evidence. Part II. Int. Angiol. 2020, 39, 175–240. [Google Scholar] [CrossRef]
- Ciostek, P.; Kowalski, M.; Woźniak, W.; Miłek, T.; Myrcha, P.; Migda, B. Phlebogriffe—A new device for mechanochemical ablation of incompetent saphenous veins: A pilot study. Phlebol. Rev. 2015, 3, 72–77. [Google Scholar] [CrossRef] [Green Version]
- Elias, S.; Lam, Y.L.; Wittens, C.H.A. Mechanochemical ablation: Status and results. Phlebology 2013, 28, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Ouvry, P.; Allaert, F.A.; Desnos, P.; Hamel-Desnos, C. Efficacy of Polidocanol Foam versus Liquid in Sclerotherapy of the Great Saphenous Vein: A Multicentre Randomised Controlled Trial with a 2-year Follow-up. Eur. J. Vasc. Endovasc. Surg. 2008, 36, 366–370. [Google Scholar] [CrossRef] [Green Version]
- Rabe, E.; Otto, J.; Schliephake, D.; Pannier, F. Efficacy and Safety of Great Saphenous Vein Sclerotherapy Using Standardised Polidocanol Foam (ESAF): A Randomised Controlled Multicentre Clinical Trial. Eur. J. Vasc. Endovasc. Surg. 2008, 35, 238–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rasmussen, L.H.; Lawaetz, M.; Bjoern, L.; Vennits, B.; Blemings, A.; Eklof, B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br. J. Surg. 2011, 98, 1079–1087. [Google Scholar] [CrossRef]
- Bishawi, M.; Bernstein, R.; Boter, M.; Draughn, D.; Gould, C.F.; Hamilton, C.; Koziarski, J. Mechanochemical ablation in patients with chronic venous disease: A prospective multicenter report. Phlebology 2014, 29, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Andrzej, P.; Zbigniew, R. Hybrid strategy in the treatment of difficult to heal venous leg ulcers. Phlebol. Rev. 2016, 24, 66–70. [Google Scholar] [CrossRef] [Green Version]
- Vun, S.V.; Rashid, S.T.; Blest, N.C.; Spark, J.I. Lower pain and faster treatment with mechanico-chemical endovenous ablation using ClariVein®. Phlebology 2014, 30, 688–692. [Google Scholar] [CrossRef]
- Ammollo, R.P.; Petrone, A.; Giribono, A.M.; Ferrante, L.; Del Guercio, L.; Bracale, U.M. Early Results of Mechanochemical Ablation with Flebogrif® in great Saphenous Vein Insufficiency: Does Polidocanol Concentration Affect Outcome? Transl. Med. @ UniSa 2020, 21, 47–51. [Google Scholar]
- Orsini, C.; Brotto, M. Immediate pathologic effects on the vein wall of foam sclerotherapy. Dermatol. Surg. 2007, 33, 1250–1254. [Google Scholar]
- Ikponmwosa, A.; Abbott, C.; Graham, A.; Homer-Vanniasinkam, S.; Gough, M.J. The Impact of Different Concentrations of Sodium Tetradecyl Sulphate and Initial Balloon Denudation on Endothelial Cell Loss and Tunica Media Injury in a Model of Foam Sclerotherapy. Eur. J. Vasc. Endovasc. Surg. 2010, 39, 366–371. [Google Scholar] [CrossRef] [Green Version]
- Smarandache, A.; Staicu, A.; Nastasa, V.; Moreno-Moraga, J.; De La Torre, J.R.; Trelles, M.; Pirvulescu, R.; Pascu, M.L. Physical properties of laser irradiated sclerosing foams. Rom. Rep. Phys. 2015, 67, 1480–1490. [Google Scholar]
- Nastasa, V.; Boni, M.; Alexandru, S.; Dinache, A. Laser Optofluidics in Fighting Multiple Drug Resistance. In Lasers in Foams and Emulsions Studies; Betham Books: Sharjah, UAE, 2017; p. 293. [Google Scholar]
- Smarandache, A. Laser beams interaction with polidocanol foam: Molecular background. Photomed. Laser Surg. 2012, 30, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Lin-Vien, D.; Colthup, N.; Fateley, W.; Grasselli, J. The Handbook of Infrared and Raman Characteristic Frequencies of Organic Molecules, 1st ed.; Elsevier: Amsterdam, The Netherlands, 1991. [Google Scholar]
- Hamel-Desnos, C.; Allaert, F.A. Liquid versus foam sclerotherapy. Phlebology 2009, 24, 240–246. [Google Scholar] [CrossRef] [PubMed]
- König, H.E.; Liebich, H.-G. Veterinary Anatomy of Domestic Mammals: Textbook and Colour Atlas, 6th ed.; Schattauer: Stuttgart, Germany, 2013; ISBN 3-7945-2101-3. [Google Scholar]
- Iłżecki, M.; Terlecki, P.; Przywara, S.; Iłżecka, J.; Dave, S.; Zubilewicz, T. The novel minimally invasive mechano-chemical technique of the saphenous vein ablation. Our center experience: Results of 24 months follow-up. Acta Angiol. 2019, 25, 127–132. [Google Scholar]










| V-1 | V-2 | V-3 | V-4 | V-Average | |
|---|---|---|---|---|---|
| Mann–Whitney U | 25.000 | 32.000 | 13.000 | 4.000 | 0.000 |
| Wilcoxon W | 61.000 | 68.000 | 49.000 | 40.000 | 36.000 |
| Z | −1.333 | −0.711 | −2.399 | −3.199 | −3.554 |
| p | 0.183 | 0.477 | 0.016 | 0.001 | 0.000 |
| V-1 | V-2 | V-3 | V-4 | V-Average | |
|---|---|---|---|---|---|
| Mann–Whitney U | 8.000 | 4.000 | 0.000 | 2.000 | 0.000 |
| Wilcoxon W | 53.000 | 49.000 | 45.000 | 47.000 | 45.000 |
| Z | −3.021 | −3.348 | −3.674 | −3.511 | −3.674 |
| p | 0.003 | 0.001 | 0.000 | 0.000 | 0.000 |
| V-1 | V-2 | V-3 | V-4 | V-Average | |
|---|---|---|---|---|---|
| Mann–Whitney U | 11.000 | 7.000 | 0.000 | 18.000 | 0.000 |
| Wilcoxon W | 56.000 | 52.000 | 45.000 | 63.000 | 45.000 |
| Z | −2.406 | −2.791 | −3.464 | −1.732 | −3.464 |
| p | 0.016 | 0.005 | 0.001 | 0.083 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rybak, Z.; Janeczek, M.; Dobrzynski, M.; Wujczyk, M.; Czerski, A.; Kuropka, P.; Noszczyk-Nowak, A.; Szymonowicz, M.; Sender-Janeczek, A.; Wiglusz, K.; et al. Study of Flebogrif®—A New Tool for Mechanical Sclerotherapy—Effectiveness Assessment Based on Animal Model. Nanomaterials 2021, 11, 544. https://doi.org/10.3390/nano11020544
Rybak Z, Janeczek M, Dobrzynski M, Wujczyk M, Czerski A, Kuropka P, Noszczyk-Nowak A, Szymonowicz M, Sender-Janeczek A, Wiglusz K, et al. Study of Flebogrif®—A New Tool for Mechanical Sclerotherapy—Effectiveness Assessment Based on Animal Model. Nanomaterials. 2021; 11(2):544. https://doi.org/10.3390/nano11020544
Chicago/Turabian StyleRybak, Zbigniew, Maciej Janeczek, Maciej Dobrzynski, Marta Wujczyk, Albert Czerski, Piotr Kuropka, Agnieszka Noszczyk-Nowak, Maria Szymonowicz, Aleksandra Sender-Janeczek, Katarzyna Wiglusz, and et al. 2021. "Study of Flebogrif®—A New Tool for Mechanical Sclerotherapy—Effectiveness Assessment Based on Animal Model" Nanomaterials 11, no. 2: 544. https://doi.org/10.3390/nano11020544