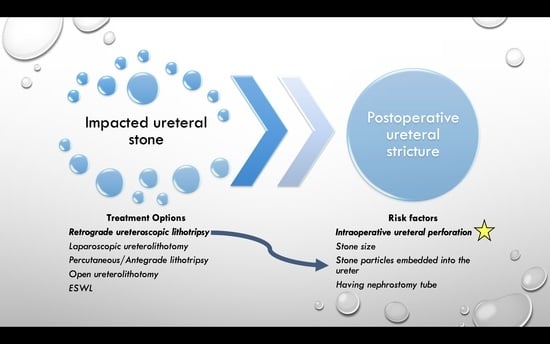
Predictors of Ureteral Strictures after Retrograde Ureteroscopic Treatment of Impacted Ureteral Stones: A Systematic Literature Review
Abstract
:1. Introduction
2. Material and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Extraction
2.3. Primary Outcomes
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xiong, M.; Zhu, X.; Chen, D.; Hossain, M.A.; Xie, Y.; Gou, X.; Deng, Y. Post ureteroscopic stone surgery ureteral strictures management: A retrospective study. Int. Urol. Nephrol. 2020, 52, 841–849. [Google Scholar] [CrossRef]
- Schuster, T.G.; Hollenbeck, B.K.; Faerber, G.J.; Wolf, J.S., Jr. Complications of ureteroscopy: Analysis of predictive factors. J. Urol. 2001, 166, 538–540. [Google Scholar] [CrossRef]
- Jung, H.D.; Hong, Y.; Lee, J.Y.; Lee, S.H. A Systematic Review on Comparative Analyses between Ureteroscopic Lithotripsy and Shock-Wave Lithotripsy for Ureter Stone According to Stone Size. Medicina 2021, 57, 1369. [Google Scholar] [CrossRef]
- Roberts, W.W.; Cadeddu, J.A.; Micali, S.; Kavoussi, L.R.; Moore, R.G. Ureteral stricture formation after removal of impacted calculi. J. Urol. 1998, 159, 723–726. [Google Scholar] [CrossRef]
- Ulvik, O.; Harneshaug, J.R.; Gjengsto, P. Ureteral Strictures Following Ureteroscopic Stone Treatment. J. Endourol. 2021, 35, 985–990. [Google Scholar] [CrossRef]
- Fam, X.I.; Singam, P.; Ho, C.C.K.; Sridharan, R.; Hod, R.; Bahadzor, B.; Goh, E.H.; Tan, G.H.; Zainuddin, Z. Ureteral stricture formation after ureteroscope treatment of impacted calculi: A prospective study. Korean J. Urol. 2015, 56, 63–67. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Brito, A.H.; Mitre, A.I.; Srougi, M. Ureteroscopic pneumatic lithotripsy of impacted ureteral calculi. Int. Braz. J. Urol. 2006, 32, 295–299. [Google Scholar] [CrossRef]
- Bayar, G.; Tanrıverdi, O.; Horasanlı, K.; Dalkılıç, A. Ureteroscopy Outcomes, Complications and Management of Perforations in Impacted Ureter Stones. J. Urol. Surg. 2016, 3, 133–137. [Google Scholar] [CrossRef]
- Alazaby, H.; Mohey, A.; Omar, R.; Sebaey, A.; Gharib, T. Impacted ≥ 10-mm pelvic ureteric stone treatment: Laser lithotripsy alone or in combination with pneumatic lithotripsy—A prospective, comparative study. Afr. J. Urol. 2020, 26, 16. [Google Scholar] [CrossRef]
- Al-Nabulsi, Z.; Phan, Y.C.; Abdalla, O.; Austin, T.; Tanasescu, G.; Osborn, P.; Auer, A.; Rowbotham, C.; Ismail, M. Surgical and radiological predictive factors for ureteric stricture formation in patients treated with ureteroscopy for ureteric stones. Scand. J. Urol. 2021, 55, 394–398. [Google Scholar] [CrossRef]
- Delvecchio, F.C.; Auge, B.K.; Brizuela, R.M.; Weizer, A.Z.; Silverstein, A.D.; Lallas, C.D.; Pietrow, P.K.; Albala, D.M.; Preminger, G.M. Assessment of stricture formation with the ureteral access sheath. Urology 2003, 61, 518–522; discussion 522. [Google Scholar] [CrossRef]
- Tran, H.; Arsovska, O.; Paterson, R.F.; Chew, B.H. Evaluation of risk factors and treatment options in patients with ureteral stricture disease at a single institution. Can. Urol. Assoc. J. 2015, 9, 921–924. [Google Scholar] [CrossRef]
- Joshi, H.N.; Singh, A.K.; Koirala, N.P.; Karmacharya, R.M. Outcome of Uretero Renoscopic Lithotripsy (URSL) with Holmium LASER Vs Pneumatic Lithotripter for Lower Ureteric Stones, Experience from University Hospital of Nepal. Kathmandu Univ. Med. J. 2020, 18, 49–53. [Google Scholar] [CrossRef]
- Degirmenci, T.; Gunlusoy, B.; Kozacioglu, Z.; Arslan, M.; Koras, O.; Arslan, B.; Minareci, S. Comparison of Ho:YAG laser and pneumatic lithotripsy in the treatment of impacted ureteral stones: An analysis of risk factors. Kaohsiung J. Med. Sci. 2014, 30, 153–158. [Google Scholar] [CrossRef]
- Binbay, M.; Tepeler, A.; Singh, A.; Akman, T.; Tekinaslan, E.; Sarilar, O.; Baykal, M.; Muslumanoglu, A.Y. Evaluation of pneumatic versus holmium:YAG laser lithotripsy for impacted ureteral stones. Int. Urol. Nephrol. 2011, 43, 989–995. [Google Scholar] [CrossRef]
- Li, L.; Pan, Y.; Weng, Z.; Bao, W.; Yu, Z.; Wang, F. A Prospective Randomized Trial Comparing Pneumatic Lithotripsy and Holmium Laser for Management of Middle and Distal Ureteral Calculi. J. Endourol. 2015, 29, 883–887. [Google Scholar] [CrossRef]
- Kassem, A.; ElFayoumy, H.; ElSaied, W.; ElGammal, M.; Bedair, A. Laser and Pneumatic Lithotripsy in the Endoscopic Management of Large Ureteric Stones: A Comparative Study. Urol. Int. 2012, 88, 311–315. [Google Scholar] [CrossRef]
- Güler, Y.; Erbin, A. Comparative evaluation of retrograde intrarenal surgery, antegrade ureterorenoscopy and laparoscopic ureterolithotomy in the treatment of impacted proximal ureteral stones larger than 1.5 cm. Cent. Eur. J. Urol. 2021, 74, 57–63. [Google Scholar] [CrossRef]
- Hu, H.; Xu, L.; Wang, S.; Yu, X.; Yang, H.; Peng, E.; Cui, L.; Li, C. Ureteral stricture formation after removal of proximal ureteral stone: Retroperitoneal laparoscopic ureterolithotomy versus ureteroscopy with holmium: YAG laser lithotripsy. PeerJ 2017, 5, e3483. [Google Scholar] [CrossRef]
- Shao, Y.; Wang, D.-W.; Lu, G.-L.; Shen, Z.-J. Retroperitoneal laparoscopic ureterolithotomy in comparison with ureteroscopic lithotripsy in the management of impacted upper ureteral stones larger than 12 mm. World J. Urol. 2015, 33, 1841–1845. [Google Scholar] [CrossRef]
- Elashry, O.M.; Elgamasy, A.K.; Sabaa, M.A.; Abo-Elenien, M.; Omar, M.A.; Eltatawy, H.H.; El-Abd, S.A. Ureteroscopic management of lower ureteric calculi: A 15-year single-centre experience. BJU Int. 2008, 102, 1010–1017. [Google Scholar] [CrossRef]
- Morgentaler, A.; Bridge, S.S.; Dretler, S.P. Management of the impacted ureteral calculus. J. Urol. 1990, 143, 263–266. [Google Scholar] [CrossRef]
- May, P.C.; Hsi, R.S.; Tran, H.; Stoller, M.L.; Chew, B.H.; Chi, T.; Usawachintachit, M.; Duty, B.D.; Gore, J.L.; Harper, J.D. The Morbidity of Ureteral Strictures in Patients with Prior Ureteroscopic Stone Surgery: Multi-Institutional Outcomes. J. Endourol. 2018, 32, 309–314. [Google Scholar] [CrossRef]
- Xi, Q.; Wang, S.; Ye, Z.; Liu, J. Combined removal of stones with resection of concurrent pathologic ureter may be a preferred treatment for impacted ureteral stones with stricture lesions. J. Endourol. 2009, 23, 243–247. [Google Scholar] [CrossRef]
- O’Sullivan, D.C.; Lemberger, R.J.; Bishop, M.C.; Bates, C.P.; Dunn, M. Ureteric stricture formation following ureteric instrumentation in patients with a nephrostomy drain in place. Br. J. Urol. 1994, 74, 165–169. [Google Scholar] [CrossRef]

| Author and Year | Study Design | Patient/Procedure Number | Mean Patient Age | Stone Size | Stone Location | Treatment | Stricture Rate | Suggested Risk Factors | Follow-Up | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Proximal Ureter | Mid Ureter | Distal Ureter | |||||||||
| Fam et al., 2015 [6] | Prospective | 64 | Up to 20 mm | 21 (32.8%) | 15 (23.4%) | 28 (43.7%) | Retrograde Ureteroscopic laser lithotripsy | 5 (7.8%) | None among intraoperative or stone-related factors | 6 months | |
| Al-Nabulsi et al., 2021 [9] | Retrospective | 297 | 52 (20–86) | Retrograde Ureteroscopic laser lithotripsy | 10 (3.3%) | Stone size, degree of hydronephrosis, Nephrostomy insertion, mucosal injury, ureteric perforation, residual stone fragments, embedded stone fragments * | 3 months | ||||
| Stricture Group | 10 | 58 | 11.5 | 5 (50%) | 3 (30%) | 2 (20%) | |||||
| Without stricture Group | 287 | 53 | 7.6 | 119 (41.5%) | 43 (15%) | 125 (43.5%) | |||||
| Alazaby et al., 2020 [10] | Prospective comparative | 90 | Laser alone, combined (laser + pneumatic) | 2 (2.2%) | Ureter mucosa laceration and embedded stone particles | Na | |||||
| Laser Group | 45 | 51 ± 9.7 | 12.8 ± 1.1 | 2 (4.4%) | |||||||
| Combined Group (Laser + Pneumatic) | 45 | 49 ± 11.4 | 13.1 ± 1.4 | 0 | |||||||
| Brito et al., 2006 [11] | Retrospective | 42 | 23–72 | 5–20 mm | 9 | 11 | 22 | Retrograde Ureteroscopic pneumatic lithotripsy | 14.2% | Ureteral perforation (treatment of proximal ureteric impacted stone has high risk of perforation) | Na |
| Bayar et al., 2016 [12] | Retrospective | 81 | 39 ± 16 | 11.5 ± 5.2 | 31 (38%) | 16 (20%) | 34 (42%) | Retrograde Ureteroscopic stone removal (laser/pneumatic) | 5.6% (4/71 in non-perforated) 80% in perforated | Perforation | 3–86 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tonyali, S.; Yilmaz, M.; Tzelves, L.; Emiliani, E.; De Coninck, V.; Keller, E.X.; Miernik, A. Predictors of Ureteral Strictures after Retrograde Ureteroscopic Treatment of Impacted Ureteral Stones: A Systematic Literature Review. J. Clin. Med. 2023, 12, 3603. https://doi.org/10.3390/jcm12103603
Tonyali S, Yilmaz M, Tzelves L, Emiliani E, De Coninck V, Keller EX, Miernik A. Predictors of Ureteral Strictures after Retrograde Ureteroscopic Treatment of Impacted Ureteral Stones: A Systematic Literature Review. Journal of Clinical Medicine. 2023; 12(10):3603. https://doi.org/10.3390/jcm12103603
Chicago/Turabian StyleTonyali, Senol, Mehmet Yilmaz, Lazaros Tzelves, Esteban Emiliani, Vincent De Coninck, Etienne Xavier Keller, and Arkadiusz Miernik. 2023. "Predictors of Ureteral Strictures after Retrograde Ureteroscopic Treatment of Impacted Ureteral Stones: A Systematic Literature Review" Journal of Clinical Medicine 12, no. 10: 3603. https://doi.org/10.3390/jcm12103603