Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links
Abstract
:1. Introduction
2. Methods
2.1. Study Selection
2.2. Qualitative Analysis
3. Results
3.1. Psychological Distress
3.2. Cognitive Impairment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sindhusake, D.; Mitchell, P.; Newall, P.; Golding, M.; Rochtchina, E.; Rubin, G. Prevalence and characteristics of tinnitus in older adults: The Blue Mountains Hearing Study: Prevalencia y características del acúfeno en adultos mayores: El Estudio de Audición Blue Mountains. Int. J. Audiol. 2003, 42, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Balla, M.P.; Greco, A.; Altissimi, G.; Ricci, P.; Turchetta, R.; De Virgilio, A.; De Vincentiis, M.; Ricci, S.; Cianfrone, G. Work-Related Noise Exposure in a Cohort of Patients with Chronic Tinnitus: Analysis of Demographic and Audiological Characteristics. Int. J. Environ. Res. Public Health 2017, 14, 1035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paciello, F.; Podda, M.V.; Rolesi, R.; Cocco, S.; Petrosini, L.; Troiani, D.; Fetoni, A.R.; Paludetti, G.; Grassi, C. Anodal transcranial direct current stimulation affects auditory cortex plasticity in normal-hearing and noise-exposed rats. Brain Stimul. 2018, 11, 1008–1023. [Google Scholar] [CrossRef] [PubMed]
- Skarzynski, P.H.; Dziendziel, B.; Gos, E.; Wlodarczyk, E.; Miaskiewicz, B.; Rajchel, J.J.; Skarzynski, H. Prevalence and Severity of Tinnitus in Otosclerosis: Preliminary Findings from Validated Questionnaires. J. Int. Adv. Otol. 2019, 15, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; Pyykkö, I.; Arroll, M.A.; Casselbrant, M.L.; Foster, C.A.; Manzoor, N.F.; Megerian, C.A.; Naganawa, S.; Young, Y.-H. Meniere’s disease. Nat. Rev. Dis. Prim. 2016, 2, 16028. [Google Scholar] [CrossRef] [PubMed]
- Cascella, V.; Giordano, P.; Hatzopoulos, S.; Petruccelli, J.; Prosser, S.; Simoni, E.; Astolfi, L.; Fetoni, A.R.; Skarżyński, H.; Martini, A. A new oral otoprotective agent. Part 1: Electrophysiology data from protection against noise-induced hearing loss. Med. Sci. Monit. 2012, 18, BR1–BR8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.-S.; Koo, M.; Chen, J.-C.; Hwang, J.-H. The association between tinnitus and the risk of ischemic cerebrovascular disease in young and middle-aged patients: A secondary case-control analysis of a nationwide, population-based health claims database. PLoS ONE 2017, 12, e0187474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shih, C.-P.; Lin, H.-C.; Chung, C.-H.; Hsiao, P.-J.; Wang, C.-H.; Lee, J.-C.; Chien, W.-C. Increased risk of tinnitus in patients with chronic kidney disease: A nationwide, population-based cohort study. PLoS ONE 2017, 12, e0183192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ralli, M.; Lobarinas, E.; Fetoni, A.R.; Stolzberg, D.; Paludetti, G.; Salvi, R. Comparison of Salicylate- and Quinine-Induced Tinnitus in Rats. Otol. Neurotol. 2010, 31, 823–831. [Google Scholar] [CrossRef] [Green Version]
- Hwang, J.-H.; Tsai, S.-J.; Liu, T.-C.; Chen, Y.-C.; Lai, J.-T. Association of Tinnitus and Other Cochlear Disorders with a History of Migraines. JAMA Otolaryngol. Neck Surg. 2018, 144, 712–717. [Google Scholar] [CrossRef]
- Knipper, M.; Van Dijk, P.; Nunes, I.; Rüttiger, L.; Zimmermann, U. Advances in the neurobiology of hearing disorders: Recent developments regarding the basis of tinnitus and hyperacusis. Prog. Neurobiol. 2013, 111, 17–33. [Google Scholar] [CrossRef]
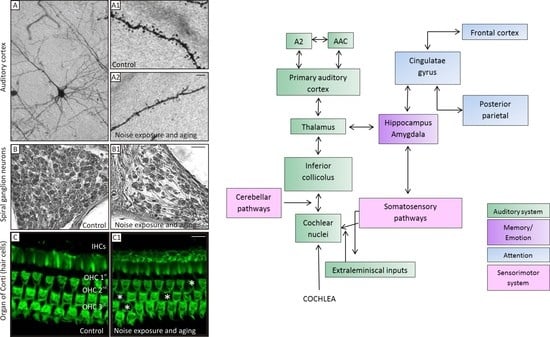
- Fetoni, A.R.; Etroiani, D.; Epetrosini, L.; Epaludetti, G. Cochlear Injury and Adaptive Plasticity of the Auditory Cortex. Front. Aging Neurosci. 2015, 7, 8. [Google Scholar] [CrossRef]
- Stolzberg, D.; Chen, G.-D.; Allman, B.; Salvi, R. Salicylate-induced peripheral auditory changes and tonotopic reorganization of auditory cortex. Neuroscience 2011, 180, 157–164. [Google Scholar] [CrossRef] [Green Version]
- Salvi, R.J.; Wang, J.; Ding, D. Auditory plasticity and hyperactivity following cochlear damage. Hear. Res. 2000, 147, 261–274. [Google Scholar] [CrossRef]
- Diesch, E.; Andermann, M.; Flor, H.; Rupp, A. Interaction among the components of multiple auditory steady-state responses: Enhancement in tinnitus patients, inhibition in controls. Neuroscience 2010, 167, 540–553. [Google Scholar] [CrossRef]
- Vanneste, S.; De Ridder, D. The auditory and non-auditory brain areas involved in tinnitus. An emergent property of multiple parallel overlapping subnetworks. Front. Syst. Neurosci. 2012, 6, 31. [Google Scholar] [CrossRef] [Green Version]
- Hébert, S.; Fournier, P.; Noreña, A. The Auditory Sensitivity is Increased in Tinnitus Ears. J. Neurosci. 2013, 33, 2356–2364. [Google Scholar] [CrossRef] [Green Version]
- Rauschecker, J.P.; Leaver, A.M.; Mühlau, M. Tuning Out the Noise: Limbic-Auditory Interactions in Tinnitus. Neuron 2010, 66, 819–826. [Google Scholar] [CrossRef] [Green Version]
- Araneda, R.; De Volder, A.G.; Deggouj, N.; Philippot, P.; Heeren, A.; Lacroix, E.; Decat, M.; Rombaux, P.; Renier, L. Altered top-down cognitive control and auditory processing in tinnitus: Evidences from auditory and visual spatial stroop. Restor. Neurol. Neurosci. 2015, 33, 67–80. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, J.-N.; Hu, W.; Li, J.-J.; Zhou, J.-X.; Shi, G.-F.; He, P.; Li, Z.-W.; Li, M. The characteristics of cognitive impairment in subjective chronic tinnitus. Brain Behav. 2018, 8, e00918. [Google Scholar] [CrossRef]
- De Corso, E.; Cantone, E.; Galli, J.; Seccia, V.; Lucidi, D.; Di Cesare, T.; Ottaviano, G.; Sergi, B.; Paludetti, G.; Fetoni, A.R. Otitis media in children: Which phenotypes are most linked to allergy? A systematic review. Pediatr. Allergy Immunol. 2021, 32, 524–534. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Fetoni, A.R.; Di Cesare, T.; Settimi, S.; Sergi, B.; Rossi, G.; Malesci, R.; Marra, C.; Paludetti, G.; De Corso, E. The evaluation of global cognitive and emotional status of older patients with chronic tinnitus. Brain Behav. 2021, in press. [Google Scholar]
- Aazh, H.; Lammaing, K.; Moore, B.C.J. Factors related to tinnitus and hyperacusis handicap in older people. Int. J. Audiol. 2017, 56, 677–684. [Google Scholar] [CrossRef]
- Park, S.Y.; Han, J.J.; Hwang, J.H.; Whang, E.S.; Yeo, S.W.; Park, S.N. Comparison of tinnitus and psychological aspects between the younger and older adult patients with tinnitus. Auris Nasus Larynx 2017, 44, 147–151. [Google Scholar] [CrossRef]
- Gopinath, B.; McMahon, C.M.; Rochtchina, E.; Karpa, M.J.; Mitchell, P. Risk factors and impacts of incident tinnitus in older adults. Ann. Epidemiol. 2010, 20, 129–135. [Google Scholar] [CrossRef]
- Lasisi, A.O.; Abiona, T.; Gureje, O. Tinnitus in the elderly: Profile, correlates, and impact in the Nigerian study of ageing. Otolaryngol. Head Neck Surg. 2010, 143, 510–515. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Maskalick, S.; Brown, K.; Gilham, B. Association between depression and tinnitus in a nationally representative sample of US older adults. Aging Ment. Health 2013, 17, 714–717. [Google Scholar] [CrossRef]
- Beukes, E.W.; Baguley, D.M.; Allen, P.M.; Manchaiah, V.; Andersson, G. Audiologist-Guided Internet-Based Cognitive Behavior Therapy for Adults With Tinnitus in the United Kingdom: A Randomized Controlled Trial. Ear Hear. 2018, 39, 423–433. [Google Scholar] [CrossRef] [Green Version]
- Park, H.-M.; Jung, J.; Kim, J.-K.; Lee, Y.-J. Tinnitus and Its Association with Mental Health and Health-Related Quality of Life in an Older Population: A Nationwide Cross-Sectional Study. J. Appl. Gerontol. 2020, 733464820966512. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Kim, H.; Lee, J.Y.; Kim, J.H.; Lee, D.Y.; Mook-Jung, I.; Kim, Y.H.; Kim, Y.K. Effects of Chronic Tinnitus on Metabolic and Structural Changes in Subjects With Mild Cognitive Impairment. Front. Aging Neurosci. 2020, 12, 594282. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Lee, J.Y.; Han, S.-Y.; Seo, Y.; Shim, Y.J.; Kim, Y.H. Neurocognition of Aged Patients with Chronic Tinnitus: Focus on Mild Cognitive Impairment. Clin. Exp. Otorhinolaryngol. 2020, 13, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.; Lee, S.-Y.; Choi, W.H.; Park, J.-C.; Lee, D.H.; Kim, Y.K.; Lee, J.H.; Lee, J.-Y.; Lee, M.J.; Kim, Y.H. Proteasome Activity in the Plasma as a Novel Biomarker in Mild Cognitive Impairment with Chronic Tinnitus. J. Alzheimer’s Dis. 2020, 78, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Q.; Chen, J.; Zhang, R.; Zhang, W.; Ruan, J.; Zhang, M.; Han, C.; Yu, Z. Heterogeneous Influence of Frailty Phenotypes in Age-Related Hearing Loss and Tinnitus in Chinese Older Adults: An Explorative Study. Front. Psychol. 2021, 11, 617610. [Google Scholar] [CrossRef]
- Fetoni, A.R.; Lucidi, D.; De Corso, E.; Fiorita, A.; Conti, G.; Paludetti, G. Relationship between Subjective Tinnitus Perception and Psychiatric Discomfort. Int. Tinnitus J. 2016, 20, 76–82. [Google Scholar] [CrossRef] [Green Version]
- Panza, F.; Solfrizzi, V.; Logroscino, G. Age-related hearing impairment—A risk factor and frailty marker for dementia and AD. Nat. Rev. Neurol. 2015, 11, 166–175. [Google Scholar] [CrossRef]
- Pattyn, T.; Eede, F.V.D.; Vanneste, S.; Cassiers, L.; Veltman, D.; Van De Heyning, P.; Sabbe, B. Tinnitus and anxiety disorders: A review. Hear. Res. 2016, 333, 255–265. [Google Scholar] [CrossRef]
- Taljaard, D.S.; Olaithe, M.; Brennan-Jones, C.G.; Eikelboom, R.H.; Bucks, R.S. The relationship between hearing impairment and cognitive function: A meta-analysis in adults. Clin. Otolaryngol. 2016, 41, 718–729. [Google Scholar] [CrossRef] [Green Version]
- Trevis, K.J.; McLachlan, N.M.; Wilson, S.J. Cognitive Mechanisms in Chronic Tinnitus: Psychological Markers of a Failure to Switch Attention. Front. Psychol. 2016, 7, 1262. [Google Scholar] [CrossRef] [Green Version]
- Mohamad, N.; Hoare, D.J.; Hall, D.A. The consequences of tinnitus and tinnitus severity on cognition: A review of the behavioural evidence. Hear. Res. 2016, 332, 199–209. [Google Scholar] [CrossRef] [Green Version]
- De Ridder, D.; Schlee, W.; Vanneste, S.; Londero, A.; Weisz, N.; Kleinjung, T.; Shekhawat, G.S.; Elgoyhen, A.B.; Song, J.-J.; Andersson, G.; et al. Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). Neuroendocrinol. Pathol. Situa. Dis. 2021, 260, 1–25. [Google Scholar] [CrossRef]
- Fortunato, S.; Forli, F.; Guglielmi, V.; De Corso, E.; Paludetti, G.; Berrettini, S.; FetonI, A. Ipoacusia e declino cognitivo: Revisione della letteratura. Acta Otorhinolaryngol. Ital. 2016, 36, 155–166. [Google Scholar] [CrossRef]
- Wingfield, A.; Grossman, M. Language and the Aging Brain: Patterns of Neural Compensation Revealed by Functional Brain Imaging. J. Neurophysiol. 2006, 96, 2830–2839. [Google Scholar] [CrossRef] [Green Version]
- Peelle, J.E.; Wingfield, A. The Neural Consequences of Age-Related Hearing Loss. Trends Neurosci. 2016, 39, 486–497. [Google Scholar] [CrossRef] [Green Version]
- Tangalos, E.G.; Petersen, R.C. Mild Cognitive Impairment in Geriatrics. Clin. Geriatr. Med. 2018, 34, 563–589. [Google Scholar] [CrossRef]
- Anzivino, R.; Conti, G.; Di Nardo, W.; Fetoni, A.R.; Picciotti, P.M.; Marra, C.; Guglielmi, V.; Fortunato, S.; Forli, F.; Paludetti, G.; et al. Prospective Evaluation of Cognitive Functions after Rehabilitation with Cochlear Implant or Hearing Aids: Preliminary Results of a Multicentric Study on Elderly Patients. Am. J. Audiol. 2019, 28, 762–774. [Google Scholar] [CrossRef]
- Guglielmi, V.; Marra, C.; Picciotti, P.M.; Iacobucci, G.M.; Giovannini, S.; Quaranta, D.; Anzivino, R.; Paludetti, G.; Conti, G. Does Hearing Loss in the Elderly Individuals Conform to Impairment of Specific Cognitive Domains? J. Geriatr. Psychiatry Neurol. 2019, 33, 231–240. [Google Scholar] [CrossRef]
- Savastano, M. Tinnitus with or without hearing loss: Are its characteristics different? Eur. Arch. Otorhinolaryngol. 2008, 265, 1295–1300. [Google Scholar] [CrossRef]
- Mazurek, B.; Olze, H.; Haupt, H.; Szczepek, A.J. The More the Worse: The Grade of Noise-Induced Hearing Loss Associates with the Severity of Tinnitus. Int. J. Environ. Res. Public Health 2010, 7, 3071–3079. [Google Scholar] [CrossRef] [Green Version]
- Deary, I.J.; Corley, J.; Gow, A.J.; Harris, S.E.; Houlihan, L.M.; Marioni, R.E.; Penke, L.; Rafnsson, S.B.; Starr, J.M. Age-associated cognitive decline. Br. Med Bull. 2009, 92, 135–152. [Google Scholar] [CrossRef]
- Harada, C.N.; Love, M.C.N.; Triebel, K.L. Normal Cognitive Aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [Green Version]
- Shahidipour, Z.; Geshani, A.; Jafari, Z.; Jalaie, S.; Khosravifard, E. Auditory memory deficit in elderly people with hearing loss. Iran J. Otorhinolaryngol. 2013, 25, 169–176. [Google Scholar]
- Aghamolaei, M.; Jafari, Z.; Grimm, S.; Zarnowiec, K.; Najafi-Koopaie, M.; Escera, C. The effects of aging on early stages of the auditory deviance detection system. Clin. Neurophysiol. 2018, 129, 2252–2258. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef] [Green Version]
- Loughrey, D.G.; Kelly, M.E.; Kelley, G.A.; Brennan, S.; Lawlor, B.A. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia. JAMA Otolaryngol. Neck Surg. 2018, 144, 115–126. [Google Scholar] [CrossRef] [PubMed]

| Author, Year [Ref] | Inclusion Criteria | Exclusion Criteria | N° of Cases, Age | Type of Study | Objective | Methods (Outcome Evaluation) | Results | Level of Evidence | Evidence of Association |
|---|---|---|---|---|---|---|---|---|---|
| Fetoni AR, 2021 [23] | -Chronic tinnitus -Age ≥ 55 y -With or without HL | -History of neurological diseases -Psychiatric disorders -Otologic diseases-Antipsychotic drugs use | 102 patients ≥55 y; 70.4 ± 9.6 y (range 55–94 y | Prospective cross-sectional study | To assess the value of self-administered screening tests in comparing severity of tinnitus perception with emotional disorders and cognitive status | THI, HADS, MMSE (questionnaires) | THI score related to HADS-A score, HADS-D score, there was no relationship between tinnitus severity and MMSE | II | Yes |
| Aazh H, 2017 [24] | -Age ≥ 60 y -Tinnitus sufferers with/without hyperacusis -With/without HL | History of neurologic and psychiatric diseases, or sleep disorders | 184 patients ≥60 y; mean age of 69 y | Retrospective cross-sectional study | To assess issues associated with tinnitus and hyperacusis handicap | HADS, HQ, ISI, THI, VAS (questionnaires) | THI was significant in predicting tinnitus annoyance. Hyperacusis handicap and insomnia were both predicted by level of depression | III | Yes |
| Park SY, 2017 [25] | -Age < and ≥ 65 y -With/without HL | History of psychiatric or neurologic diseases | 76 patients ≥65 y | Retrospective cohort study | To assess differences between tinnitus-related features and psychological aspects between younger and older tinnitus sufferers | THI, BDI, and BEPSI (questionnaires) | No differences in tinnitus severity, depression, and stress between younger and older subjects | III | Yes/No |
| Gopinath B, 2010 [26] | -Age ≥ 50 y -With/without tinnitus -With/without HL | History of psychiatric diseases | 1214 participants (602 with tinnitus) ≥50 y | Longitudinal cohort study | To evaluate the risk factors and effects of tinnitus (depression) | SF-36; MHI for depression and/or CES-D (questionnaires) | Lessened quality of life and wellbeing in patients with tinnitus | II | Yes |
| Lasisi AO, 2010 [27] | -Age ≥ 65 y -With/without tinnitus; -With/without HL | History of neuropsychologic diseases | 184 patients ≥65 y; mean age of 77.3 y | Longitudinal cohort study | To establish the prevalence of tinnitus in the elderly and its influence on their life quality | WHOQOL (questionnaire) | Tinnitus sufferers had a lower perception of their overall health and a worse life quality; twofold likelihood to suffer activities impairment in daily living | II | Yes |
| Loprinzi PD, 2013 [28] | -Age ≥ 70 y -With/without tinnitus -With/without HL | Age < 70 years old | 696 patients 76 ± 0.2 y (range 70–85 y) | Prospective cross-sectional study | To evaluate the association between tinnitus and depression | Patient Health Questionnaire-9 (questionnaire) | Positive association between tinnitus (at least a moderate) and depression; patients bothered by tinnitus before going to bed were nearly 3 times more likely to be depressed | II | Yes, in moderate/severe tinnitus |
| Beukes EW, 2018 [29] | -Age< and > 60 y -Chronic tinnitus -With/without HL who completed therapy | History of neuropsychiatric diseases | 146 patientsstratified for age (> 60 y) | A randomized, delayed intervention efficacy trial | To establish if an internet-based cognitive behavioral therapy is useful in reducing tinnitus severity and associated comorbidities | ISI, Generalized Anxiety Disorder-7, Patient Health Questionnaire-9, Hearing Handicap Inventory for adults, HQ, Cognitive Failures Questionnaire, Satisfaction with Life Scales (questionnaires | Significant reduction in tinnitus and comorbidities (insomnia, depression, hyperacusis, cognitive failures) and improving of life quality | I | Yes |
| Park HM, 2020 [30] | -Age ≥ 60 y -With/without tinnitus -With/without HL | History of neurologic or psychiatric diseases | 5129 patients ≥60 y (range 60–79 y) | Retrospective cross-sectional study | To find a possible association of tinnitus, mental health, and health-related quality of life | Stress was tested asking: “How much stress do you usually feel in your daily life?”; depression was tested using CIDI-SF; suicide ideation with the question: “Have you ever thought about committing suicide within 12 months?” (questionnaires) | The annoying tinnitus patients had more depression, psychological stress, and suicidal ideation if compared to control group | III | Yes |
| Author, Year [Ref] | Inclusion Criteria | Exclusion Criteria | N° of Cases, Age | Type of Study | Objective | Methods (Outcome Evaluation) | Results | Level of Evidence | Evidence of Association |
|---|---|---|---|---|---|---|---|---|---|
| Lee SY, 2020 [31] | -Age > 60 y -Diagnosed for MCI -With/without tinnitus | -Moderate or severe hearing loss -Otologic diseases -History of psychiatric or neurologic disorders | 23 patients (12 with tinnitus) 74.0 ± 6.1 y (range 63–83 y) | Retrospective cohort study | To examine the glucose metabolism and gray matter volume in patients with MCI and tinnitus | MCI with or without tinnitus: FDG-PET and magnetic resonance imaging were performed (imaging) | Specific brain regions are associated with cognitive decline and increased tinnitus severity | III | Yes |
| Lee SY, 2020 [32] | -Age ≥ 65 y -With/without HL | History of psychiatric or neurologic disorders | 58 patients68.1 ± 5.1 y (range 65–82 y) | Prospective cohort study | To examine the cognitive domains and the association between tinnitus severity and cognitive functions | K-PHQ-9, K-IADL, MoCA-K (questionnaires) | THI score in the MCI group was higher than in the non-MCI | II | Yes |
| Yun Y, 2020 [33] | -Age > 50 y -Chronic tinnitus | -History of Alzheimer’s disease or neurologic diseases -Hearing loss or otologic diseases | 55 patients > 50 y | Cross-sectional study | To examine plasma c-proteasome activity in association with cognitive functions in chronic tinnitus patients | Plasma c-proteasome activity was achieved with fluorogenic reporter substrate; MoCA (cut-off score of 22/23) to assess MCI (markers and questionnaires) | Circulating proteasomes were lower in patients with chronic tinnitus and MCI | III | Yes |
| Fetoni AR, 2021 [23] | -Chronic tinnitus -Age ≥ 55 y -With/without HL | -History of neurological diseases -Psychiatric disorders -Otologic diseases-Antipsychotic drugs use | 102 patients ≥ 55 y | Prospective cross-sectional study | To evaluate the use of self-administered screening tests to correlate the severity of tinnitus with emotional disorders and the overall cognitive status | THI, HADS, MMSE (questionnaires) | THI score was directly related to HADS score, there was no relationship between tinnitus severity and MMSE | II | No |
| Beukes EW, 2018 [29] | -Age < and > 60 y -Chronic tinnitus-With/without HL -Who completed therapy | History of neuropsychiatric diseases | 146 patients stratified for age (>60 y) | Randomized delayed intervention efficacy trial | To establish if an internet-based cognitive behavioral therapy is useful to lessen tinnitus severity and associated comorbidities | ISI, Generalized Anxiety Disorder, Patient Health Questionnaire, Hearing Handicap Inventory for Adults Screening version, HQ, Cognitive Failures Questionnaire, Satisfaction with Life Scales (questionnaires) | Significant reduction in tinnitus and comorbidities (insomnia, depression, hyperacusis, cognitive failures) and a significant rise in life quality | I | Yes |
| Ruan Q, 2021 [34] | -Age ≥ 58 y -With/without frailty -With/without HL -With/without tinnitus | No history of disability, cophosis, and vision loss | 429 patients ≥58 y | Longitudinal cohort study | To study whether cognitive frailty is associated with HL and tinnitus | To assess MCI: with executive and attention domain (TMT A and B); language domain (BNT and animal list generation); memory domain (HVLT-R) (questionnaires) | Cognitive frailty patients had higher risks of severe HL and tinnitus. Cognitive impairment in tinnitus patients involved executive, memory, and attention domains; altered processing speed | II | Yes/No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malesci, R.; Brigato, F.; Di Cesare, T.; Del Vecchio, V.; Laria, C.; De Corso, E.; Fetoni, A.R. Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links. J. Clin. Med. 2021, 10, 1881. https://doi.org/10.3390/jcm10091881
Malesci R, Brigato F, Di Cesare T, Del Vecchio V, Laria C, De Corso E, Fetoni AR. Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links. Journal of Clinical Medicine. 2021; 10(9):1881. https://doi.org/10.3390/jcm10091881
Chicago/Turabian StyleMalesci, Rita, Francesca Brigato, Tiziana Di Cesare, Valeria Del Vecchio, Carla Laria, Eugenio De Corso, and Anna Rita Fetoni. 2021. "Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links" Journal of Clinical Medicine 10, no. 9: 1881. https://doi.org/10.3390/jcm10091881