Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns
Abstract
:1. Introduction
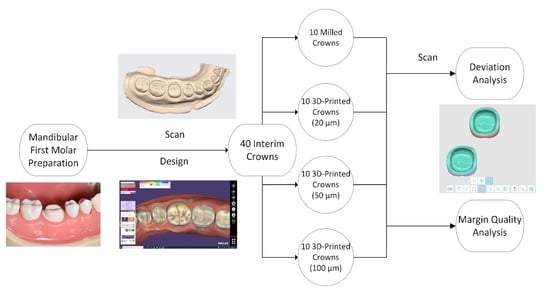
2. Materials and Methods
2.1. Model and Crown Data Acquisition
2.2. Crown Fabrication
2.3. Crown Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, Y.; Ye, H.; Wang, Y.; Zhao, Y.; Sun, Y.; Zhou, Y. Three-dimensional analysis of internal adaptations of crowns cast from resin patterns fabricated using computer-aided design/computer-assisted manufacturing technologies. Int. J. Prosthodont. 2018, 31, 386–393. [Google Scholar] [CrossRef] [Green Version]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry-state of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Muta, S.; Ikeda, M.; Nikaido, T.; Sayed, M.; Sadr, A.; Suzuki, T.; Tagami, J. Chairside fabrication of provisional crowns on FDM 3D-printed PVA model. J. Prosthodont. Res. 2020, 64, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [Green Version]
- Salmi, M.; Paloheimo, K.S.; Tuomi, J.; Ingman, T.; Mäkitie, A. A digital process for additive manufacturing of occlusal splints: A clinical pilot study. J. R. Soc. Interface. 2013, 10, 20130203. [Google Scholar] [CrossRef]
- Zeng, L.; Zhang, Y.; Liu, Z.; Wei, B. Effects of repeated firing on the marginal accuracy of Co-Cr copings fabricated by selective laser melting. J. Prosthet. Dent. 2015, 113, 135–139. [Google Scholar] [CrossRef]
- Salmi, M.; Paloheimo, K.S.; Tuomi, J.; Wolff, J.; Mäkitie, A. Accuracy of medical models made by additive manufacturing (rapid manufacturing). J. Craniomaxillofac. Surg. 2013, 41, 603–609. [Google Scholar] [CrossRef]
- Reyes, A.; Turkyilmaz, I.; Prihoda, T.J. Accuracy of surgical guides made from conventional and a combination of digital scanning and rapid prototyping techniques. J. Prosthet. Dent. 2015, 113, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Wismeijer, D.; Osman, R.B. Additive manufacturing techniques in prosthodontics: Where do we currently stand? A critical review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Bai, W.; Cheng, X.; Tian, J.; Wei, D.; Sun, Y.; Di, P. Effects of printing layer thickness on mechanical properties of 3D-printed custom trays. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef]
- Lerner, H.; Nagy, K.; Pranno, N.; Zarone, F.; Admakin, O.; Mangano, F. Trueness and precision of 3D-printed versus milled monolithic zirconia crowns: An in vitro study. J. Dent. 2021, 103792. [Google Scholar] [CrossRef]
- Zhang, Z.C.; Li, P.L.; Chu, F.T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Son, K.; Lee, J.H.; Lee, K.B. Comparison of intaglio surface trueness of interim dental crowns fabricated with SLA 3D printing, DLP 3D printing, and milling technologies. Healthcare 2021, 9, 983. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Peng, C.C.; Chung, K.H.; Ramos, V., Jr. Assessment of the adaptation of interim crowns using different measurement techniques. J. Prosthodont. 2020, 29, 87–93. [Google Scholar] [CrossRef]
- Peng, C.C.; Chung, K.H.; Yau, H.T.; Ramos, V., Jr. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Simoneti, D.M.; Pereira-Cenci, T.; Dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Mai, H.N.; Lee, K.B.; Lee, D.H. Fit of interim crowns fabricated using photopolymer-jetting 3D printing. J. Prosthet. Dent. 2017, 118, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Jung, B.Y.; Han, S.S.; Woo, C.W. Accuracy evaluation of 3D printed interim prosthesis fabrication using a CBCT scanning based digital model. PLoS ONE 2020, 15, e0240508. [Google Scholar] [CrossRef]
- Davis, S.; O’Connell, B. The provisional crown. J. Ir. Dent. Assoc. 2004, 50, 167–172. [Google Scholar] [PubMed]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3d-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, S.Y.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Kim, J.G. Dimensional accuracy of dental models for three-unit prostheses fabricated by various 3D printing technologies. Materials 2021, 14, 1550. [Google Scholar] [CrossRef]
- Çakmak, G.; Yilmaz, H.; Treviño, A.; Kökat, A.M.; Yilmaz, B. The effect of scanner type and scan body position on the accuracy of complete-arch digital implant scans. Clin. Implant. Dent. Relat. Res. 2020, 22, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.Y.; Son, K.; Lee, K.B. Evaluation of intaglio surface trueness and margin quality of interim crowns in accordance with the build angle of stereolithography apparatus 3-dimensional printing. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- You, S.M.; You, S.G.; Kang, S.Y.; Bae, S.Y.; Kim, J.H. Evaluation of the accuracy (trueness and precision) of a maxillary trial denture according to the layer thickness: An in vitro study. J. Prosthet. Dent. 2021, 125, 139–145. [Google Scholar] [CrossRef]
- Park, G.S.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Seo, D.G. Effects of Printing Parameters on the fit of implant-supported 3D printing resin prosthetics. Materials 2019, 12, 2533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaefer, O.; Watts, D.C.; Sigusch, B.W.; Kuepper, H.; Guentsch, A. Marginal and internal fit of pressed lithium disilicate partial crowns in vitro: A three-dimensional analysis of accuracy and reproducibility. Dent. Mater. 2012, 28, 320–326. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Standardization. ISO-5725-2. Accuracy (Trueness and Precision) of Measurement Methods and Results-Part 2: Basic Method for the Determination of Repeatability and Reproducibility of a Standard Measurement Method; ISO: Geneva, Switzerland, 1994; Available online: http://www.iso.org/iso/store.htm (accessed on 22 December 1994).
- Wang, W.; Yu, H.; Liu, Y.; Jiang, X.; Gao, B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J. Prosthet. Dent. 2019, 121, 285–291. [Google Scholar] [CrossRef]
- Baumgartner, S.; Gmeiner, R.; Schönherr, J.A.; Stampfl, J. Stereolithography-based additive manufacturing of lithium disilicate glass ceramic for dental applications. Mater. Sci. Eng. C. Mater. Biol. Appl. 2020, 116, 111180. [Google Scholar] [CrossRef]
- Vilela Teixeira, A.B.; Dos Reis, A.C. Influence of parameters and characteristics of complete denture bases fabricated by 3D printing on evaluated properties: A scoping review. Int. J. Prosthodont. 2021. [Google Scholar] [CrossRef]
- Dias Resende, C.C.; Quirino Barbosa, T.A.; Moura, G.F.; Piola Rizzante, F.A.; Mendonça, G.; Zancopé, K.; Domingues das Neves, F. Cost and effectiveness of 3-dimensionally printed model using three different printing layer parameters and two resins. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef] [PubMed]
- Haddadi, Y.; Ranjkesh, B.; Isidor, F.; Bahrami, G. Marginal and internal fit of crowns based on additive or subtractive manufacturing. Biomater. Investig. Dent. 2021, 8, 87–91. [Google Scholar] [CrossRef]
- Li, R.; Chen, H.; Wang, Y.; Sun, Y. Performance of stereolithography and milling in fabricating monolithic zirconia crowns with different finish line designs. J. Mech. Behav. Biomed. Mater. 2021, 115, 104255. [Google Scholar] [CrossRef]
- Pan, Y.; Tsoi, J.K.H.; Lam, W.Y.H.; Pow, E.H.N. Implant framework misfit: A systematic review on assessment methods and clinical complications. Clin. Implant. Dent. Relat. Res. 2021, 23, 244–258. [Google Scholar] [CrossRef]
- Zimmermann, M.; Ender, A.; Mehl, A. Local accuracy of actual intraoral scanning systems for single-tooth preparations in vitro. J. Am. Dent. Assoc. 2020, 151, 127–135. [Google Scholar] [CrossRef]
- O’Toole, S.; Osnes, C.; Bartlett, D.; Keeling, A. Investigation into the accuracy and measurement methods of sequential 3D dental scan alignment. Dent. Mater. 2019, 35, 495–500. [Google Scholar] [CrossRef]
- Pellitteri, F.; Brucculeri, L.; Spedicato, G.A.; Siciliani, G.; Lombardo, L. Comparison of the accuracy of digital face scans obtained by two different scanners. Angle Orthod. 2021, 91, 641–649. [Google Scholar] [CrossRef]
- Peroz, S.; Spies, B.C.; Adali, U.; Beuer, F.; Wesemann, C. Measured accuracy of intraoral scanners is highly dependent on methodical factors. J. Prosthodont. Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Lee, W.S.; Lee, K.B. Effect of different software programs on the accuracy of dental scanner using three-dimensional analysis. Int. J. Environ. Res. Public Health 2021, 18, 8449. [Google Scholar] [CrossRef]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Day, S.J.; Altman, D.G. Statistics notes: Blinding in clinical trials and other studies. BMJ 2000, 321, 504. [Google Scholar] [CrossRef] [PubMed] [Green Version]








| Layer Thickness | Overall RMS (µm) | External RMS (µm) | Intaglio RMS (µm) | Marginal RMS (µm) | Intaglio Occlusal RMS (µm) |
|---|---|---|---|---|---|
| Control (Milled) | 64.5 ±10.94 a | 54 ±21.29 a | 32.6 ±15.01 a | 11.3 ±14.36 a | 31.5 ±6.92 a |
| 20 µm | 56.1 ±10.7 a | 59.4 ±10.7 a | 49.9 ±12.13 ab | 14.9 ±9.57 a | 33.4 ± 2.22 ab |
| 50 µm | 53.3 ±9.3 a | 48.5 ±13.67 a | 45.4 ±15.75 ab | 9.1 ±8.02 a | 34.7 ±1.83 ab |
| 100 µm | 61.3 ±15.31 a | 62.4 ±18.21 a | 52.8 ±17.32 b | 14.6 ±9.94 a | 41.5 ±12.55 b |
| p values | 0.145 | 0.263 | 0.026 | 0.576 | 0.024 |
| Locations | ||||||
|---|---|---|---|---|---|---|
| Layer Thickness | Buccal-Lingual | Buccal-Mesial | Buccal-Distal | Lingual-Mesial | Lingual-Distal | Mesial-Distal |
| Control (Milled) | 0.005 | 0.03 | 0.005 | 0.885 | >0.05 | 0.885 |
| 20 µm | 0.121 | 0.762 | 0.988 | 0.566 | 0.223 | 0.914 |
| 50 µm | 0.765 | 0.765 | 0.988 | >0.05 | 0.915 | 0.915 |
| 100 µm | <0.001 | 0.831 | 0.831 | <0.001 | <0.001 | >0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Çakmak, G.; Cuellar, A.R.; Donmez, M.B.; Schimmel, M.; Abou-Ayash, S.; Lu, W.-E.; Yilmaz, B. Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns. Appl. Sci. 2021, 11, 9246. https://doi.org/10.3390/app11199246
Çakmak G, Cuellar AR, Donmez MB, Schimmel M, Abou-Ayash S, Lu W-E, Yilmaz B. Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns. Applied Sciences. 2021; 11(19):9246. https://doi.org/10.3390/app11199246
Chicago/Turabian StyleÇakmak, Gülce, Alfonso Rodriguez Cuellar, Mustafa Borga Donmez, Martin Schimmel, Samir Abou-Ayash, Wei-En Lu, and Burak Yilmaz. 2021. "Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns" Applied Sciences 11, no. 19: 9246. https://doi.org/10.3390/app11199246