Health 2050: The Realization of Personalized Medicine through Crowdsourcing, the Quantified Self, and the Participatory Biocitizen
Abstract
:1. Introduction
1.1. Contemporary Public Health Challenges
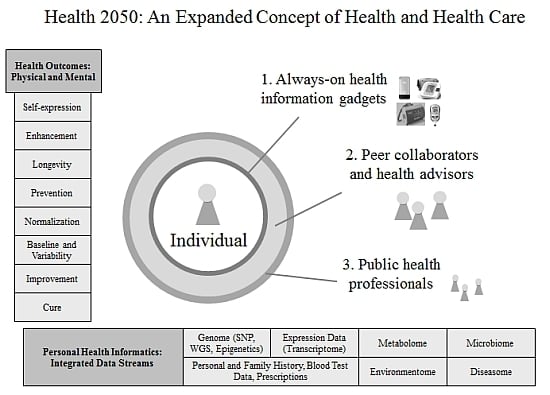
1.2. Health 2050
1.3. Preventive Medicine
2. Health 2050: Preventive Medicine

2.1. Greatly Expanded Range of Health Outcomes
2.2. Data Stream Integration Needed for Personal Health Informatics
2.3. Participant-Centric Action-taking
Mental Performance and Cognitive Acuity is the New Health Frontier
2.4. The 80% of a Condition’s Life Cycle While It Is still Pre-Clinical
2.4.1. Concept of Health, Service Providers, Remedy Providers, and Research Conduct
| Category | Pre-Clinical (80%) | Clinical (20%) |
|---|---|---|
| Concept of health | Wellness maintenance, prevention | Illness cure |
| Service providers | Wellness: Health advisors, wellness coaches, genomic counselors, prevention specialists | Medical: Public health system |
| Remedy providers | Health engagement platforms, health social networks, peer collaborators, supplementation treatments, medical tourism | Pharmaceutical companies |
| Research conduct | Crowdsourced studies, health social networks, CRO 2.0 a [18] | Academia |
| Financial models | HSA, b out of pocket | Professional payers, insurance |
| Privacy and security | Cloud, PHRs c | Physician office, paper files |
| Legislative influence | Patient Advocacy Groups | Medical professionals |
| Regulation and oversight | Portable consent [19], IRB 2.0 d | Institutional IRB |
2.4.2. Financial Models and Economics
2.4.3. Privacy and Security, Legislative Influence, and Regulation and Oversight
3. The Realization of Health 2050: Preventive Medicine
3.1. Personalized Typing

3.1.1. Genotyping and Haplotype Groups
3.1.2. Enterotyping the Microbiome
3.1.3. Endotyping Asthma
3.2. Participatory Health Efforts
| (Light) | Level of Participant Engagement | (Intensive) | |||
|---|---|---|---|---|---|
| Social Media | Mobile Phone Health Apps | Personal Health Records (PHRs) | Health Social Networks (HSNs) | Consumer Genomics | Crowdsourced Health Studies |
3.2.1. Social Media
3.2.2. Mobile Phone Health Apps
3.2.3. Personal Health Records (PHRs)
3.2.4. Health Social Networks (HSNs)
3.2.5. Consumer Genomics
3.2.6. Crowdsourced Health Studies
3.3. Era of Big Health Data
3.3.1. Search and Social Media Aggregation of Health Information
3.3.2. Using Big Health Data for Preventive Prediction
3.4. Change in Philosophical Mindset and Other Qualitative Shifts
3.4.1. Overview of Participatory Health Communities
3.4.2. Motivations of Crowdsourced Study Participants
3.4.3. Quantified Self Study: Are New Forms of Knowledge Being Generated?
3.4.4. Quantified Self Study Results
3.4.5. Participatory Health Pioneers Are Defining the Preventive Medicine Mindset
3.5. Limitations
4. Conclusion
Acknowledgements
Conflict of Interest
References
- Kaiser Family Foundation. Health care costs: A primer. 2012. Available online: http://www.kff.org/insurance/upload/7670-03.pdf (accessed on 25 July 2012).
- OECD. Health at a glance 2011: OECD indicators. 2011. Available online: http://www.oecd.org/dataoecd/12/16/49084355.pdf (accessed on 25 July 2012).
- Begley, S. Is healthy weight impossible for many Americans? 2012. Available online: http://today.msnbc.msn.com/id/47337275/ns/today-today_health/t/healthy-weight-impossible-many-americans/#.T-_d-fUkKSp (accessed on 25 July 2012).
- Voice of America. Populations are aging worldwide. 2009. Available online: http://www.voanews.com/content/a-13-2005-11-30-voa69/397115.html (accessed on 25 July 2012).
- Gavura, S. What does a new drug cost? Sci. Based Med. 2011. Available online: http://www.sciencebasedmedicine.org/index.php/what-does-a-new-drug-cost/ (accessed on 25 July 2012).
- Himmelstein, D.U.; Thorne, D.; Warren, E.; Woolhandler, S. Medical bankruptcy in the United States, 2007: Results of a national study. Am. J. Med. 2009, 122, 741–746. [Google Scholar] [CrossRef]
- Hood, L. Lee Hood. Nat. Biotechnol. 2011, 29. [Google Scholar]
- National Cancer Institute. Personalized medicine. Dictionary of cancer terms. Available online: http://www.cancer.gov/dictionary?cdrid=561717 (accessed on 25 July 2012).
- Herper, M. Government unveils first map of all the germs in the human body. Forbes. 2012. Available online: http://www.forbes.com/sites/matthewherper/2012/06/13/government-unveils-first-map-of-all-the-germs-in-the-human-body/ (accessed on 25 July 2012).
- Voineagu, I.; Wang, X.; Johnston, P.; Lowe, J.K.; Tian, Y.; Horvath, S.; Mill, J.; Cantor, R.M.; Blencowe, B.J.; Geschwind, D.H. Transcriptomic analysis of autistic brain reveals convergent molecular pathology. Nature 2011, 474, 380–384. [Google Scholar]
- Hueber, W.; Kidd, B.A.; Tomooka, B.H.; Lee, B.J.; Bruce, B.; Fries, J.F.; Sønderstrup, G.; Monach, P.; Drijfhout, J.W.; van Venrooij, W.J.; et al. Antigen microarray profiling of autoantibodies in rheumatoid arthritis. Arthritis Rheum. 2005, 52, 2645–2655. [Google Scholar]
- Fox, S. Pew Research Center’s Internet and American Life Project. The social life of health information. 2011. Available online: http://www.pewInternet.org/Reports/2011/Social-Life-of-Health-Info.aspx (accessed on 25 July 2012).
- Leong, C. TedMed highlights: Here’s to the future of health and medicine. 2012. Massive Health Blog. Available online: http://blog.massivehealth.com/post/21793580940/tedmed-highlights-heres-to-the-future-of-health-and (accessed on 25 July 2012).
- Cattriona citing Medline Plus/National Library of Medicine. 20 million people in the United States. askville by Amazon. 2011. Available online: http://askville.amazon.com/percentage-people-USA-suffering-depression/AnswerViewer.do?requestId=7150700 (accessed on 25 July 2012).
- Foreman, A.C.; Hall, C.; Bone, K.; Cheng, J.; Kaplin, A. Just text me: Using SMS technology for collaborative patient mood charting. J. Participat. Med. 2011, 3, e45. [Google Scholar]
- Harrison, V.; Proudfoot, J.; Wee, P.P.; Parker, G.; Pavlovic, D.H.; Manicavasagar, V. Mobile mental health: Review of the emerging field and proof of concept study. J. Ment. Health 2011, 20, 509–524. [Google Scholar] [CrossRef]
- Trudeau, M. Mental health apps: Like a ‘Therapist In Your Pocket.’ 2010. NPR. Available online: http://www.npr.org/templates/story/story.php?storyId=127081326 (accessed on 25 July 2012).
- Swan, M. Scaling crowdsourced health studies: The emergence of a new form of contract research organization. Pers. Med. 2012, 9, 223–234. [Google Scholar] [CrossRef]
- Wilbanks, J. Portable legal consent and consent to research. 2012. TED Glob. Available online: http://weconsent.us/ (accessed on 25 July 2012).
- Rognlin, B. The easiest food journal you’ll ever keep: The eatery. Blisstree. 2012. Available online: http://blisstree.com/eat/nutrition/food-journal-app-the-eatery-weight-loss-733/ (accessed on 25 July 2012).
- Swan, M. Crowdsourced health research studies: An important emerging complement to clinical trials in the public health research ecosystem. J. Med. Internet Res. 2012, 14, e46. [Google Scholar] [CrossRef]
- Zeff, A. New BD Veritor™ System for Rapid Detection of Flu A+B Receives 510(k) Clearance and CLIA Waiver. 2012. Becton Dickinson Company. Available online: http://www.bd.com/contentmanager/b_article.asp?Item_ID=26567&ContentType_ID=1&BusinessCode=20001&d=BD+Worldwide&s=&dTitle=&dc=&dcTitle= (accessed on 25 July 2012).
- Heianza, Y.; Arase, Y.; Fujihara, K.; Tsuji, H.; Saito, K.; Hsieh, S.; Kodama, S.; Shimano, H.; Yamada, N.; Hara, S.; et al. High normal HbA(1c) levels were associated with impaired insulin secretion without escalating insulin resistance in Japanese individuals: The Toranomon Hospital Health Management Center Study 8 (TOPICS 8). Diabet. Med. 2012. [Google Scholar]
- Manolio, T.A.; Collins, F.S.; Cox, N.J.; Goldstein, D.B.; Hindorff, L.A.; Hunter, D.J.; McCarthy, M.I.; Ramos, E.M.; Cardon, L.R.; Chakravarti, A.; et al. Finding the missing heritability of complex diseases. Nature 2009, 461, 747–753. [Google Scholar] [CrossRef]
- González, A.M.; Maceira, B.M.; Pérez, E.; Cabrera, V.M.; López, A.J.; Larruga, J.M. Genetics, environment, and diabetes-related end-stage renal disease in the Canary Island. Genet. Test. Mol. Bioma. 2012, 16, 859–886. [Google Scholar] [CrossRef]
- Santos, J.L.; de la Cruz, R.; Holst, C.; Grau, K.; Naranjo, C.; Maiz, A.; Astrup, A.; Saris, W.H.; MacDonald, I.; Oppert, J.M.; et al. Allelic variants of melanocortin 3 receptor gene (MC3R) and weight loss in obesity: a randomised trial of hypo-energetic high- versus low-fat diets. PLoS One 2011, 6, e19934. [Google Scholar]
- Sun, B.; Chamarthi, B.; Williams, J.S.; Krug, A.W.; Lasky-Su, J.; Raby, B.A.; Hopkins, P.N.; Jeunemaitre, X.; Ferri, C.; Williams, G.H. Different polymorphisms of the mineralocorticoid receptor gene are associated with either glucocorticoid or mineralocorticoid levels in hypertension. J. Clin. Endocr. Metab. 2012. [Google Scholar]
- Vandiedonck, C.; Taylor, M.S.; Lockstone, H.E.; Plant, K.; Taylor, J.M.; Durrant, C.; Broxholme, J.; Fairfax, B.P.; Knight, J.C. Pervasive haplotypic variation in the spliceo-transcriptome of the human major histocompatibility complex. Genome Res. 2011, 21, 1042–1054. [Google Scholar] [CrossRef]
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; et al. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180. [Google Scholar]
- Willingham, E. Which of the three gut types are you? 2011. EarthSky. Available online: http://earthsky.org/human-world/which-of-the-three-gut-types-are-you/ (accessed on 25 July 2012).
- NewTime. Microbiome—Beings who live in us, controlling our lives. Finding the World. Available online: http://www.findingtheworld.com/microbiome-beings-who-live-in-us-controlling-our-lives/ (accessed on 25 July 2012).
- Poon, A.H.; Hamid, Q. Personalized medicine for asthma: Are we there yet? Ann. Thorac. Med. 2012, 7, 55–56. [Google Scholar] [CrossRef]
- Lötvall, J.; Akdis, C.A.; Bacharier, L.B.; Bjermer, L.; Casale, T.B.; Custovic, A.; Lemanske, R.F., Jr.; Wardlaw, A.J.; Wenzel, S.E.; Greenberger, P.A. Asthma endotypes: A new approach to classification of disease entities within the asthma syndrome. J. Allergy Clin. Immunol. 2011, 127, 355–360. [Google Scholar]
- Kaye, J.; Curren, L.; Anderson, N.; Edwards, K.; Fullerton, S.M.; Kanellopoulou, N.; Lund, D.; MacArthur, D.G.; Mascalzoni, D.; Shepherd, J.; et al. From patients to partners: Participant-centric initiatives in biomedical research. Nat. Rev. Genet. 2012, 13, 371–376. [Google Scholar] [CrossRef]
- Hughes, B.; Joshi, I.; Wareham, J. Health 2.0 and medicine 2.0: Tensions and controversies in the field. J. Med. Internet Res. 2008, 10, e23. [Google Scholar] [CrossRef]
- Frydman, G. A Patient-Centric Definition of Participatory Medicine. 2010. e-patients.net. Available online: http://e-patients.net/archives/2010/04/a-patient-centric-definition-of-participatory-medicine.html (accessed on 25 July 2012).
- Swan, M. The future of health: An overview of participant-driven research and medicine. Presented at Interpharma 37th Health Seminar, Lausanne, Switzerland, November 10, 2012; Available online: http://www.slideshare.net/lablogga/participant-drivenhealth (accessed on 25 July 2012).
- Dufau, S.; Duñabeitia, J.A.; Moret-Tatay, C.; McGonigal, A.; Peeters, D.; Alario, F.X.; Balota, D.A.; Brysbaert, M.; Carreiras, M.; Ferrand, L.; et al. Smart phone, smart science: How the use of smartphones can revolutionize research in cognitive science. PLoS One 2011, 6, e24974. [Google Scholar]
- Boulos, M.N.; Wheeler, S.; Tavares, C.; Jones, R. How smartphones are changing the face of mobile and participatory healthcare: An overview, with example from eCAALYX. Biomed. Eng. Online 2011, 10. [Google Scholar]
- Kiser, K. 25 ways to use your smartphone. Physicians share their favorite uses and apps. Minn. Med. 2011. Available online: http://www.minnesotamedicine.com/Default.aspx?tabid=3724 (accessed on 25 July 2012).
- Emily. US Physicians Adopt iPad in Record Numbers. 2012. PadGadget. Available online: http://www.padgadget.com/2012/05/14/us-physicians-adopt-ipad-in-record-numbers/ (accessed on 25 July 2012).
- Etherington, D. HealthTap Debuts Paid Private Medical Consultations Via Mobile Device. 2012. Available online: http://betakit.com/2012/06/28/healthtap-debuts-paid-private-medical-consultations-via-mobile-device (accessed on 25 July 2012).
- Practice Central. Reimbursement for Telehealth Services. 2011. Available online: http://www.apapracticecentral.org/update/2011/03-31/reimbursement.aspx (accessed on 25 July 2012).
- Harper, J. Pros and Cons of Telemedicine for Today’s Workers. 2012. U.S. News. Available online: http://health.usnews.com/health-news/articles/2012/07/24/pros-and-cons-of-telemedicine-for-todays-workers/ (accessed on 25 July 2012).
- Dolan, P.L. Nearly all U.S. Doctors are now on social media. 2011. amednews.com. Available online: http://www.ama-assn.org/amednews/2011/09/26/bil20926.htm/ (accessed on 25 July 2012).
- Tanner, L. Doctors increasingly becoming savvy with technology, social media. 2012. Available online: http://www.huffingtonpost.com/2012/06/11/doctors-technology-social-media-twitter-facebook-health_n_1586624.html/ (accessed on 25 July 2012).
- More than 1.5 million users are proving aetna’s personal health record is a building block to better health. Aetna. 2011. Available online: http://www.aetna.com/news/newsReleases/2011/0906-PHR.html (accessed on 25 July 2012).
- Swan, M. Emerging patient-driven health care models: An examination of health social networks, consumer personalized medicine and quantified self-tracking. Int. J. Environ. Res. Public Health 2009, 2, 492–525. [Google Scholar] [CrossRef]
- Raven, K. 23andMe’s Face in the Crowdsourced Health Research Industry Gets Bigger. Nature. 2012. Available online: http://blogs.nature.com/spoonful/2012/07/23andmes-face-in-the-crowdsourced-health-research-industry-gets-bigger.html (accessed on 25 July 2012).
- Swan, M. Multigenic condition risk assessment in direct-to-consumer genomic services. Genet. Med. 2010, 12, 279–288. [Google Scholar] [CrossRef]
- Marcus, A.D. Citizen scientists: Ordinary people are taking control of their health data, making their DNA public and running their own experiments. Their big question: Why should science be limited to professionals? Wall Street J. 2011. Available online: online.wsj.com/article/SB10001424052970204621904577014330551132036.html (accessed on 25 July 2012).
- U.S. Food and Drug Administration. Table of Pharmacogenomic Biomarkers in Drug Labels. 2012. Available online: http://www.fda.gov/Drugs/ScienceResearch/ResearchAreas/Pharmacogenetics/ucm083378.htm/ (accessed on 25 July 2012).
- Lohr, S. The Age of Big Data. New York Times. 2012. Available online: http://www.nytimes.com/2012/02/12/sunday-review/big-datas-impact-in-the-world.html?pagewanted=all (accessed on 25 July 2012).
- Lehmann, J.; Lalmas, M.; Yom-Tov, E.; Dupret, G. Models of user engagement. In Proceedings of the 20th International Conference on User Modeling, Adaptation and Personalization (UMAP 2012), Montreal, Canada, 16–20 July 2012.
- ScienceDaily. Google flu trends estimates off, study finds. 2010. Available online: http://www.sciencedaily.com/releases/2010/05/100517101714.htm (accessed on 25 July 2012).
- Chunara, R.; Andrews, J.R.; Brownstein, J.S. Social and news media enable estimation of epidemiological patterns early in the 2010 Haitian cholera outbreak. Am. J. Trop. Med. Hyg. 2012, 86, 39–45. [Google Scholar] [CrossRef]
- Boulos, M.N.; Resch, B.; Crowley, D.N.; Breslin, J.G.; Sohn, G.; Burtner, R.; Pike, W.A.; Jezierski, E.; Chuang, K.Y. Crowdsourcing, citizen sensing and sensor web technologies for public and environmental health surveillance and crisis management: Trends, OGC standards and application examples. Int. J. Health Geogr. 2011. [Google Scholar]
- Keeso, A. Technlogy helping people to track and manage illness and disease. 2012. Available online: http://betakit.com/2012/06/23/technology-helping-people-to-track-and-manage-illness-and-diseaseand http://www.nowtrendingchallenge.com (accessed on 25 July 2012).
- Stomp, W. Foldit success story: Monkey virus retroviral protease structure solved within days. MedGadget. 2011. Available online: http://medgadget.com/2011/09/foldit-success-story-monkey-virus-retroviral-protease-structure-solved-within-days.html (accessed on 25 July 2012).
- Stomp, W. Another Success for Foldit: Gamers Increase Enzyme Activity by a Factor of 18. MedGadget. 2012. Available online: http://medgadget.com/2012/01/another-success-for-foldit-gamers-increase-enzyme-activity-by-a-factor-of-18.html (accessed on 25 July 2012).
- Freifeld, C.C.; Chunara, R.; Mekaru, S.R.; Chan, E.H.; Kass-Hout, T.; Ayala Iacucci, A.; Brownstein, J.S. Participatory epidemiology: Use of mobile phones for community-based health reporting. PLoS Med. 2010, 7, e1000376. [Google Scholar] [CrossRef]
- Biggers, G. Engagement from the Trenches & Benches, Individuals and participation in research: Sharing, controlling, collaborating. Testimony for the Presidential Commission for the Study of Bioethical Issues. Available online: http://www.tvworldwide.com/events/bioethics/120517/globe_show/default_go_archive.cfm?gsid=2049&type=flv&test=0&live=0and http://blog.bioethics.gov/2012/05/17/quotes-a-discussion-on-whole-genome-sequencing/ (accessed on 25 July 2012).
- Swan, M.; Hathaway, K.; Hogg, C.; McCauley, R.; Vollrath, A. Citizen science genomics as a model for crowdsourced preventive medicine research. J. Participat. Med. 2010, 2 Supplementary Material Item 6. Personal statements from study participants, p. e20. Available online: http://www.jopm.org/citizen-science-genomics-as-a-model-for-crowd-sourced-preventive-medicine-research-supplementary-material/ (accessed on 25 July 2012).
- Taleb, N.N. The Black Swan: The Impact of the Highly Improbable, 1st ed.; Random House: New York, NY, USA, 2007; pp. 1–25. [Google Scholar]
- Dolan, B. Safeway: Healthier employees pay less. MobiHealthNews. 2009. Available online: http://mobihealthnews.com/4808/insurance-discounts-for-healthy-safeway-employees/ (accessed on 25 July 2012).
- Susman, T. New York Mayor Bloomberg takes aim at giant-sized sugary sodas. Los Angeles Times. 2012. Available online: http://articles.latimes.com/2012/may/31/nation/la-na-nn-bloomberg-sugary-drinks-20120531 (accessed on 25 July 2012).
- Associated Press. Anti-obesity pill Belvig gets FDA OK. Cleveland.com. 2012. Available online: http://www.cleveland.com/healthfit/index.ssf/2012/06/anti-obesity_pill_belvig_gets.html (accessed on 25 July 2012).
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Swan, M. Health 2050: The Realization of Personalized Medicine through Crowdsourcing, the Quantified Self, and the Participatory Biocitizen. J. Pers. Med. 2012, 2, 93-118. https://doi.org/10.3390/jpm2030093
Swan M. Health 2050: The Realization of Personalized Medicine through Crowdsourcing, the Quantified Self, and the Participatory Biocitizen. Journal of Personalized Medicine. 2012; 2(3):93-118. https://doi.org/10.3390/jpm2030093
Chicago/Turabian StyleSwan, Melanie. 2012. "Health 2050: The Realization of Personalized Medicine through Crowdsourcing, the Quantified Self, and the Participatory Biocitizen" Journal of Personalized Medicine 2, no. 3: 93-118. https://doi.org/10.3390/jpm2030093