The Effect of Medical Cooperation in the CKD Patients: 10-Year Multicenter Cohort Study
Abstract
:1. Introduction
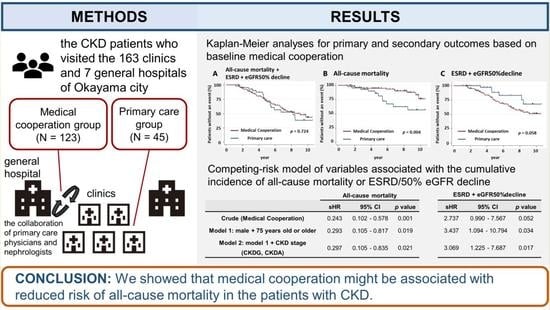
2. Materials and Methods
2.1. Study Subjects
2.2. Variables and Data Sources
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics of the Participants
3.2. Outcomes
3.3. The Effect of Medical Cooperation on the Blood Pressure Control
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Couser, W.G.; Remuzzi, G.; Mendis, S.; Tonelli, M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011, 80, 1258–1270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bello, A.K.; Levin, A.; Tonelli, M.; Okpechi, I.G.; Feehally, J.; Harris, D.; Jindal, K.; Salako, B.L.; Rateb, A.; Osman, M.A.; et al. Assessment of Global Kidney Health Care Status. JAMA 2017, 317, 1864–1881. [Google Scholar] [CrossRef]
- Naito, T.; Ohtani, H.; Kobayashi, K.; Miyazaki, M.; Yamada, K.; Sugawara, M.; Naka, Y.; Saruta, T. Current status of and regional differences in CKD management and medical cooperation in Japan: From the results of a nationwide questionnaire survey for primary care physicians. Jpn. J. Nephrol. 2013, 55, 1391–1400. (In Japanese) [Google Scholar]
- Nagai, K.; Asahi, K.; Iseki, K.; Yamagata, K. Estimating the prevalence of definitive chronic kidney disease in the Japanese general population. Clin. Exp. Nephrol. 2021, 25, 885–892. [Google Scholar] [CrossRef]
- Yamagata, K.; Takahashi, H.; Suzuki, S.; Mase, K.; Hagiwara, M.; Shimizu, Y.; Hirayama, K.; Kobayashi, M.; Narita, M.; Koyama, A. Age distribution and yearly changes in the incidence of ESRD in Japan. Am. J. Kidney Dis. 2004, 43, 433–443. [Google Scholar] [CrossRef]
- Cortes-Sanabria, L.; Cabrera-Pivaral, C.E.; Cueto-Manzano, A.M.; Rojas-Campos, E.; Barragan, G.; Hernandez-Anaya, M.; Martinez-Ramirez, H.R. Improving care of patients with diabetes and CKD: A pilot study for a cluster-randomized trial. Am. J. Kidney Dis. 2008, 51, 777–788. [Google Scholar] [CrossRef]
- Jafar, T.H.; Allen, J.C.; Jehan, I.; Hameed, A.; Saffari, S.E.; Ebrahim, S.; Poulter, N.; Chaturvedi, N. Health Education and General Practitioner Training in Hypertension Management: Long-Term Effects on Kidney Function. Clin. J. Am. Soc. Nephrol. 2016, 11, 1044–1053. [Google Scholar] [CrossRef] [Green Version]
- Jha, V.; Arici, M.; Collins, A.J.; Garcia-Garcia, G.; Hemmelgarn, B.R.; Jafar, T.H.; Pecoits-Filho, R.; Sola, L.; Swanepoel, C.R.; Tchokhonelidze, I.; et al. Understanding kidney care needs and implementation strategies in low- and middle-income countries: Conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2016, 90, 1164–1174. [Google Scholar] [CrossRef] [Green Version]
- Yamagata, K. 5. Effect of Medical Cooperation on Prevention of CKD Aggravation. J. Jpn. Soc. Intern. Med. 2015, 104, 556–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamagata, K.; Makino, H.; Iseki, K.; Ito, S.; Kimura, K.; Kusano, E.; Shibata, T.; Tomita, K.; Narita, I.; Nishino, T.; et al. Effect of Behavior Modification on Outcome in Early- to Moderate-Stage Chronic Kidney Disease: A Cluster-Randomized Trial. PLoS ONE 2016, 11, e0151422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uchida, H.A.; Maeshima, Y.; Sugiyama, H.; Wada, J.; Makino, H. Medical cooperation system for chronic kidney disease. Jpn. J. Nephrol. 2019, 61, 81–85. (In Japanese) [Google Scholar]
- Jiamjariyapon, T.; Ingsathit, A.; Pongpirul, K.; Vipattawat, K.; Kanchanakorn, S.; Saetie, A.; Kanistanon, D.; Wongprompitak, P.; Leesmidt, V.; Watcharasaksilp, W.; et al. Effectiveness of Integrated Care on Delaying Progression of stage 3–4 Chronic Kidney Disease in Rural Communities of Thailand (ESCORT study): A cluster randomized controlled trial. BMC Nephrol. 2017, 18, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.H.; Chiu, Y.W.; Hwang, S.J.; Tsai, J.C.; Shi, H.Y.; Lin, M.Y. Effect of nephrology referrals and multidisciplinary care programs on renal replacement and medical costs on patients with advanced chronic kidney disease: A retrospective cohort study. Medicine 2019, 98, e16808. [Google Scholar] [CrossRef]
- Imamura, Y.; Takahashi, Y.; Hayashi, T.; Iwamoto, M.; Nakamura, R.; Goto, M.; Takeba, K.; Shinohara, M.; Kubo, S.; Joki, N. Usefulness of multidisciplinary care to prevent worsening renal function in chronic kidney disease. Clin. Exp. Nephrol. 2019, 23, 484–492. [Google Scholar] [CrossRef]
- Imasawa, T.; Saito, C.; Kai, H.; Iseki, K.; Kazama, J.J.; Shibagaki, Y.; Sugiyama, H.; Nagata, D.; Narita, I.; Nishino, T.; et al. Long-term Effectiveness of a Primary Care Practice Facilitation Program for Chronic Kidney Disease Management: An Extended Follow-up of a Cluster-Randomized FROM-J Study. Nephrol. Dial. Transplant. 2022, 38, 158–166. [Google Scholar] [CrossRef]
- Uchida, H.A. Growing kidney disease education with involvement of the community healthcare cooperation office. Jpn. J. Nephrol. 2015, 57, 828–832. (In Japanese) [Google Scholar]
- National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39 (Suppl. S1), S1–S266. [Google Scholar]
- Japanese Society of Nephrology. Essential points from Evidence-based Clinical Practice Guidelines for Chronic Kidney Disease 2018. Clin. Exp. Nephrol. 2019, 23, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.E.; Levin, A.; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and Management of Chronic Kidney Disease: Synopsis of the Kidney Disease: Improving Global Outcomes 2012 Clinical Practice Guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukui, A.; Yokoo, T.; Nangaku, M.; Kashihara, N. New measures against chronic kidney diseases in Japan since 2018. Clin. Exp. Nephrol. 2019, 23, 1263–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fine, J.P.; Gray, R.J. A Proportional Hazards Model for the Subdistribution of a Competing Risk. J. Am. Stat. Assoc. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Ito, T.; Kamei, F.; Sonoda, H.; Oba, M.; Kawanishi, M.; Yoshimura, R.; Fukunaga, S.; Egawa, M. Effectiveness of CKD Exacerbation Countermeasures in Izumo City. J. Pers. Med. 2021, 11, 1104. [Google Scholar] [CrossRef]
- Fukui, A.; Takeshita, K.; Nakashima, A.; Maruyama, Y.; Yokoo, T. Chronic Kidney Disease Patients Visiting Various Hospital Departments: An Analysis in a Hospital in Central Tokyo, Japan. J. Pers. Med. 2022, 12, 39. [Google Scholar] [CrossRef]
- Umebayashi, R.; Uchida, H.A.; Matsuoka-Uchiyama, N.; Sugiyama, H.; Wada, J. Prevalence of Chronic Kidney Disease and Variation of Its Risk Factors by the Regions in Okayama Prefecture. J. Pers. Med. 2022, 12, 97. [Google Scholar] [CrossRef]
- Wagner, E.H. The role of patient care teams in chronic disease management. BMJ 2000, 320, 569–572. [Google Scholar] [CrossRef] [Green Version]
- Blumenthal, J.A.; Hinderliter, A.L.; Smith, P.J.; Mabe, S.; Watkins, L.L.; Craighead, L.; Ingle, K.; Tyson, C.; Lin, P.H.; Kraus, W.E.; et al. Effects of Lifestyle Modification on Patients With Resistant Hypertension: Results of the TRIUMPH Randomized Clinical Trial. Circulation 2021, 144, 1212–1226. [Google Scholar] [CrossRef]
- Gaede, P.; Lund-Andersen, H.; Parving, H.H.; Pedersen, O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N. Engl. J. Med. 2008, 358, 580–591. [Google Scholar] [CrossRef] [Green Version]
- Shikata, K.; Haneda, M.; Ninomiya, T.; Koya, D.; Suzuki, Y.; Suzuki, D.; Ishida, H.; Akai, H.; Tomino, Y.; Uzu, T.; et al. Randomized trial of an intensified, multifactorial intervention in patients with advanced-stage diabetic kidney disease: Diabetic Nephropathy Remission and Regression Team Trial in Japan (DNETT-Japan). J. Diabetes Investig. 2021, 12, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Hemmelgarn, B.R.; Manns, B.J.; Zhang, J.; Tonelli, M.; Klarenbach, S.; Walsh, M.; Culleton, B.F. Association between multidisciplinary care and survival for elderly patients with chronic kidney disease. J. Am. Soc. Nephrol. 2007, 18, 993–999. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Y.; Xiong, J.; Chen, Y.; Deng, J.; Peng, H.; Zhao, J.; He, J. The effectiveness of multidisciplinary care models for patients with chronic kidney disease: A systematic review and meta-analysis. Int. Urol. Nephrol. 2018, 50, 301–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wavamunno, M.D.; Harris, D.C. The need for early nephrology referral. Kidney Int. Suppl. 2005, 67, S128–S132. [Google Scholar] [CrossRef] [Green Version]
- Smart, N.A.; Dieberg, G.; Ladhani, M.; Titus, T. Early referral to specialist nephrology services for preventing the progression to end-stage kidney disease. Cochrane Database Syst. Rev. 2014, 6, CD007333. [Google Scholar] [CrossRef]
- Bayliss, E.A.; Bhardwaja, B.; Ross, C.; Beck, A.; Lanese, D.M. Multidisciplinary team care may slow the rate of decline in renal function. Clin. J. Am. Soc. Nephrol. 2011, 6, 704–710. [Google Scholar] [CrossRef] [Green Version]
- Barrett, B.J.; Garg, A.X.; Goeree, R.; Levin, A.; Molzahn, A.; Rigatto, C.; Singer, J.; Soltys, G.; Soroka, S.; Ayers, D.; et al. A nurse-coordinated model of care versus usual care for stage 3/4 chronic kidney disease in the community: A randomized controlled trial. Clin. J. Am. Soc. Nephrol. 2011, 6, 1241–1247. [Google Scholar] [CrossRef] [Green Version]
- Schor, A.; Bergovoy-Yellin, L.; Landsberger, D.; Kolobov, T.; Baron-Epel, O. Multidisciplinary work promotes preventive medicine and health education in primary care: A cross-sectional survey. Isr. J. Health Policy Res. 2019, 8, 50. [Google Scholar] [CrossRef] [Green Version]
- Savica, V.; Bellinghieri, G.; Monardo, P.; Muraca, U.; Santoro, D. An update on calcium metabolism alterations and cardiovascular risk in patients with chronic kidney disease: Questions, myths and facts. J. Nephrol. 2013, 26, 456–464. [Google Scholar] [CrossRef]
- Savica, V.; Calo, L.A.; Monardo, P.; Caldarera, R.; Cavaleri, A.; Santoro, D.; Muraca, U.; Mallamace, A.; Bellinghieri, G. High phosphate content beverages in dialysis patients: Relevance for hyperphosphatemia and cardiovascular risk. Nutr. Metab. Cardiovasc. Dis. 2008, 18, e39–e40. [Google Scholar] [CrossRef]
- Nitta, K.; Hanafusa, N.; Akiyama, K.; Kawaguchi, Y.; Tsuchiya, K. Chronic Kidney Disease—Mineral and Bone Disorder (CKD-MBD), from Bench to Bedside. Kidney Dial. 2023, 3, 46–55. [Google Scholar] [CrossRef]
- Gansevoort, R.T.; Correa-Rotter, R.; Hemmelgarn, B.R.; Jafar, T.H.; Heerspink, H.J.L.; Mann, J.F.; Matsushita, K.; Wen, C.P. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 2013, 382, 339–352. [Google Scholar] [CrossRef] [PubMed]




| Medical Cooperation Group (N = 123) | Primary Care Group (N = 45) | p Value | |||
|---|---|---|---|---|---|
| Follow-up, months | 69.9 ± 33.8 | 62.7 ± 34.2 | 0.223 | ||
| Age, years | 61.7 ± 17.3 | 76.0 ± 9.6 | <0.001 | ||
| Male, n (%) | 74 | (60.2) | 17 | (37.8) | 0.010 |
| Hypertension, n (%) | 88 | (71.5) | 35 | (77.8) | 0.419 |
| Diabetes mellitus, n (%) | 34 | (27.6) | 11 | (24.4) | 0.679 |
| Systolic blood pressure, mmHg | 130.8 ± 21.1 | 127.6 ± 15.2 | 0.648 | ||
| Diastolic blood pressure, mmHg | 74.6 ± 13.8 | 69.4 ± 11.3 | 0.031 | ||
| Serum creatinine, mg/dL | 1.27 (0.92–1.71) | 1.28 (1.06–1.56) | 0.742 | ||
| eGFR, mL/min/1.73 m2 | 41.6 (27.7–61.8) | 33.0 (26.9–42.6) | 0.024 | ||
| Qualitative proteinuria, −/±/1+/2+/3+/4+ | 52/16/26/20/7/2 | 21/6/11/4/3/0 | 0.799 | ||
| Urinary protein excretion, g/gCr | 0.25 (0.09–1.01) | 0.56 (0.11–0.94) | 0.870 | ||
| Total cholesterol, mg/dL | 193 (164–221) | 208 (199–217) | 0.506 | ||
| Triglyceride, mg/dL | 143 (93–203) | 118 (70–165) | 0.516 | ||
| HDL-C, mg/dL | 54 (44–70) | 73 (58–88) | 0.240 | ||
| LDL-C, mg/dL | 110 (92–136) | 115 (94–135) | 0.977 | ||
| Uric acid, mg/dL | 6.7 (5.5–7.4) | 4.3 (3.5–5.0) | 0.054 | ||
| Hemoglobin, g/dL | 12.8 (10.9–14.0) | 11.6 (10.7–13.4) | 0.107 | ||
| All-Cause Mortality | ESRD + eGFR50% Decline | |||||
|---|---|---|---|---|---|---|
| Subhazard Ratio | 95% CI | p Value | Subhazard Ratio | 95% CI | p Value | |
| Crude (Medical Cooperation) | 0.243 | 0.102–0.578 | 0.001 | 2.737 | 0.990–7.567 | 0.052 |
| Model 1: male + 75 years old or older | 0.293 | 0.105–0.817 | 0.019 | 3.437 | 1.094–10.794 | 0.034 |
| Model 2: model 1 + CKD stage (CKDG, CKDA) | 0.297 | 0.105–0.835 | 0.021 | 3.069 | 1.225–7.687 | 0.017 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onishi, Y.; Uchida, H.A.; Maeshima, Y.; Okuyama, Y.; Otaka, N.; Ujike, H.; Tanaka, K.; Takeuchi, H.; Tsuji, K.; Kitagawa, M.; et al. The Effect of Medical Cooperation in the CKD Patients: 10-Year Multicenter Cohort Study. J. Pers. Med. 2023, 13, 582. https://doi.org/10.3390/jpm13040582
Onishi Y, Uchida HA, Maeshima Y, Okuyama Y, Otaka N, Ujike H, Tanaka K, Takeuchi H, Tsuji K, Kitagawa M, et al. The Effect of Medical Cooperation in the CKD Patients: 10-Year Multicenter Cohort Study. Journal of Personalized Medicine. 2023; 13(4):582. https://doi.org/10.3390/jpm13040582
Chicago/Turabian StyleOnishi, Yasuhiro, Haruhito A. Uchida, Yohei Maeshima, Yuka Okuyama, Nozomu Otaka, Haruyo Ujike, Keiko Tanaka, Hidemi Takeuchi, Kenji Tsuji, Masashi Kitagawa, and et al. 2023. "The Effect of Medical Cooperation in the CKD Patients: 10-Year Multicenter Cohort Study" Journal of Personalized Medicine 13, no. 4: 582. https://doi.org/10.3390/jpm13040582