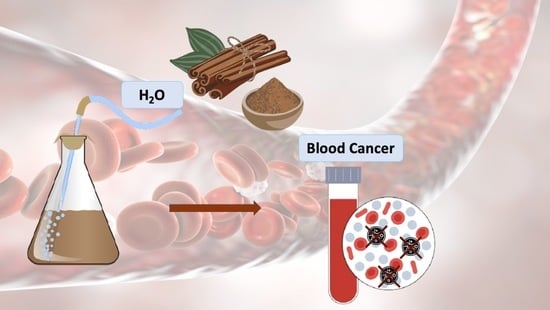
The Anti-Cancer Effect of Cinnamon Aqueous Extract: A Focus on Hematological Malignancies
Abstract
:1. Introduction
2. Cinnamon and Cancer: Pathways and Mechanisms of Action
2.1. Inhibition of NF-KB and AP-1
2.2. Activation of Cytotoxic CD8+ T Cells
2.3. Inhibition of COX-2 and Inflammatory Cells
2.4. Inhibition of PI3K/Akt/mTOR, MAPK-P38alfa and DHFR
2.5. Inhibition of Angiogenesis
3. Cinnamon and Hematological Malignancies
3.1. Acute Myeloid Leukemia
3.1.1. Acute Promyelocytic Leukemia
3.1.2. Acute Erythroblastic Leukemia
3.2. Lymphoma
4. Clinical Trials
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kwon, H.-K.; Hwang, J.-S.; So, J.-S.; Lee, C.-G.; Sahoo, A.; Ryu, J.-H.; Jeon, W.K.; Ko, B.S.; Im, C.-R.; Lee, S.H.; et al. Cinnamon extract induces tumor cell death through inhibition of NFκB and AP1. BMC Cancer 2010, 10, 392. [Google Scholar] [CrossRef]
- Assadollahi, V.; Gholami, M.; Zendedel, A.C. Zeylanicum aqueous extract induced apoptosis in the human myelocytic leukemia cell line (THP-1). Bratisl. Med. J. 2015, 116, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Abeysekera, W.P.K.M.; Premakumara, G.A.S.; Ratnasooriya, W.D. Anti-inflammatory, cytotoxicity and antilipidemic properties: Novel bioactivities of true cinnamon (Cinnamomum zeylanicum Blume) leaf. BMC Complement. Med. Ther. 2022, 22, 259. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Safdar, M.; Khan, M.M.A.; Khattak, K.N.; Anderson, R.A. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care 2003, 26, 3215–3218. [Google Scholar] [CrossRef] [PubMed]
- Youn, H.S.; Lee, J.K.; Choi, Y.J.; Saitoh, S.I.; Miyake, K.; Hwang, D.H.; Lee, J.Y. Cinnamaldehyde suppresses toll-like receptor 4 activation mediated through the inhibition of receptor oligomerization. Biochem. Pharmacol. 2008, 75, 494–502. [Google Scholar] [CrossRef]
- Aggarwal, S.; Bhadana, K.; Singh, B.; Rawat, M.; Mohammad, T.; Al-Keridis, L.A.; Alshammari, N.; Hassan, I.; Das, S.N. Cinnamomum zeylanicum extract and its bioactive component cinnamaldehyde show anti-tumor effects via inhibition of multiple cellular pathways. Front. Pharmacol. 2022, 13, 918479. [Google Scholar] [CrossRef] [PubMed]
- Alsayadi, A.I.; Abutaha, N.; Almutairi, B.O.; Al-Mekhlafi, F.A.; Wadaan, M.A. Evaluating the efficacy of an innovative herbal formulation (HF6) on different human cancer cell lines. Environ. Sci. Pollut. Res. 2022, 29, 51768–51777. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Jayawardana, R.; Galappaththy, P.; Constantine, G.R.; Gunawardana, N.D.V.; Katulanda, P. Efficacy and safety of ‘true’ cinnamon (Cinnamomum zeylanicum) as a pharmaceutical agent in diabetes: A systematic review and meta-analysis. Diabet. Med. 2012, 29, 1480–1492. [Google Scholar] [CrossRef]
- Clinical Trials about the Use of Cinnamon Extract in Cancer. Available online: clinicaltrials.gov (accessed on 18 February 2023).
- Maiuolo, J.; Gliozzi, M.; Carresi, C.; Musolino, V.; Oppedisano, F.; Scarano, F.; Nucera, S.; Scicchitano, M.; Bosco, F.; Macri, R.; et al. Nutraceuticals and Cancer: Potential for Natural Polyphenols. Nutrients 2021, 13, 3834. [Google Scholar] [CrossRef]
- Liu, Y.; An, T.; Wan, D.; Yu, B.; Fan, Y.; Pei, X. Targets and mechanism used by cinnamaldehyde, the main active ingredient in cinnamon, in the treatment of breast cancer. Front. Pharmacol. 2020, 11, 582719. [Google Scholar] [CrossRef]
- Wilson, H.E.; Stanton, D.A.; Rellick, S.; Geldenhuys, W.; Pistilli, E.E. Breast cancer-associated skeletal muscle mitochondrial dysfunction and lipid accumulation is reversed by PPARG. Am. J. Physiol. Physiol. 2021, 320, C577–C590. [Google Scholar] [CrossRef] [PubMed]
- Mofers, A.; Pellegrini, P.; Linder, S.; D’arcy, P. Proteasome-associated deubiquitinases and cancer. Cancer Metastasis Rev. 2017, 36, 635–653. [Google Scholar] [CrossRef]
- Allegra, A.; Di Gioacchino, M.; Tonacci, A.; Petrarca, C.; Musolino, C.; Gangemi, S. Multiple myeloma cell-derived exosomes: Implications on tumorigenesis, diagnosis, prognosis and therapeutic strategies. Cells 2021, 10, 2865. [Google Scholar] [CrossRef]
- Gopalakrishnan, S.; Ediga, H.H.; Reddy, S.S.; Reddy, G.B.; Ismail, A. Procyanidin-B2 enriched fraction of cinnamon acts as a proteasome inhibitor and anti-proliferative agent in human prostate cancer cells. IUBMB Life 2018, 70, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Borner, C. The Bcl-2 protein family: Sensors and checkpoints for life-or-death decisions. Mol. Immunol. 2003, 39, 615–647. [Google Scholar] [CrossRef] [PubMed]
- Jochum, W.; Passegué, E.; Wagner, E.F. AP-1 in mouse development and tumorigenesis. Oncogene 2001, 20, 2401–2412. [Google Scholar] [CrossRef]
- Kwon, H.-K.; Jeon, W.K.; Hwang, J.-S.; Lee, C.-G.; So, J.-S.; Park, J.-A.; Ko, B.S.; Im, S.-H. Cinnamon extract suppresses tumor progression by modulating angiogenesis and the effector function of CD8+ T cells. Cancer Lett. 2009, 278, 174–182. [Google Scholar] [CrossRef]
- Rahmani, M.; Nkwocha, J.; Hawkins, E.; Pei, X.; Parker, R.E.; Kmieciak, M.; Leverson, J.D.; Sampath, D.; Ferreira-Gonzalez, A.; Grant, S. Cotargeting BCL-2 and PI3K induces BAX-Dependent mitochondrial apoptosis in AML cells. Cancer Res. 2018, 78, 3075–3086. [Google Scholar] [CrossRef]
- Delannoy, A.; Wilhelm, E.; Eilebrecht, S.; Alvarado-Cuevas, E.M.; Benecke, A.G.; Bell, B. BIM and NOXA are mitochondrial effectors of TAF6δ-driven apoptosis. Cell Death Dis. 2018, 9, 70. [Google Scholar] [CrossRef]
- Glab, J.A.; Puthalakath, H.; Zhang, S.R.; Vinh, A.; Drummond, G.R.; Sobey, C.G.; De Silva, T.M.; Kim, H.A. Bim deletion reduces functional deficits following ischemic stroke in association with modulation of apoptosis and inflammation. NeuroMolecular Med. 2022, 24, 405–414. [Google Scholar] [CrossRef]
- Zhang, X.; Ge, J.; Zhu, X.; Zhang, H.; Wang, Y.; Xu, T.; Jiang, W.; Zhang, B. Effects and mechanism of oxymatrine combined with compound Yinchen granules on the apoptosis of hepatocytes through the Akt/FoxO3a/Bim pathway. BioMed. Res. Int. 2022, 2022, 8644356. [Google Scholar] [CrossRef] [PubMed]
- Jenner, A.; Peña-Blanco, A.; Salvador-Gallego, R.; Ugarte-Uribe, B.; Zollo, C.; Ganief, T.; Bierlmeier, J.; Mund, M.; Lee, J.E.; Ries, J.; et al. DRP1 interacts directly with BAX to induce its activation and apoptosis. EMBO J. 2022, 41, e108587. [Google Scholar] [CrossRef] [PubMed]
- Spitz, A.Z.; Gavathiotis, E. Physiological and pharmacological modulation of BAX. Trends Pharmacol. Sci. 2022, 43, 206–220. [Google Scholar] [CrossRef] [PubMed]
- Toruno, C.; Carbonneau, S.; Stewart, R.A.; Jette, C. Interdependence of bad and puma during ionizing-radiation-induced apoptosis. PLoS ONE 2014, 9, e88151. [Google Scholar] [CrossRef]
- Zhou, H.; Fang, Q.; Li, N.; Yu, M.; Chen, H.; Guo, S. ASMq protects against early burn wound progression in rats by alleviating oxidative stress and secondary mitochondria-associated apoptosis via the Erk/p90RSK/Bad pathway. Mol. Med. Rep. 2021, 23, 390. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, Y.; Xia, S.; Kong, Q.; Li, S.; Liu, X.; Junqueira, C.; Meza-Sosa, K.F.; Mok, T.M.Y.; Ansara, J.; et al. Gasdermin E suppresses tumour growth by activating anti-tumour immunity. Nature 2020, 579, 415–420. [Google Scholar] [CrossRef]
- Ng, S.S.; Rivera, F.D.L.; Yan, J.; Corvino, D.; Das, I.; Zhang, P.; Kuns, R.; Chauhan, S.B.; Hou, J.; Li, X.-Y.; et al. The NK cell granule protein NKG7 regulates cytotoxic granule exocytosis and inflammation. Nat. Immunol. 2020, 21, 1205–1218. [Google Scholar] [CrossRef]
- Läubli, H.; Borsig, L. Altered cell adhesion and glycosylation promote cancer immune suppression and metastasis. Front. Immunol. 2019, 10, 2120. [Google Scholar] [CrossRef]
- Cao, X.; Cai, S.F.; Fehniger, T.A.; Song, J.; Collins, L.I.; Piwnica-Worms, D.R.; Ley, T.J. Granzyme B and perforin are important for Regulatory T cell-mediated suppression of tumor clearance. Immunity 2007, 27, 635–646. [Google Scholar] [CrossRef]
- Hiroyasu, S.; Zeglinski, M.R.; Zhao, H.; Pawluk, M.A.; Turner, C.T.; Kasprick, A.; Tateishi, C.; Nishie, W.; Burleigh, A.; Lennox, P.A.; et al. Granzyme B inhibition reduces disease severity in autoimmune blistering diseases. Nat. Commun. 2021, 12, 302. [Google Scholar] [CrossRef]
- Velotti, F.; Barchetta, I.; Cimini, F.A.; Cavallo, M.G. Granzyme B in Inflammatory Diseases: Apoptosis, Inflammation, Extracellular Matrix Remodeling, Epithelial-to-Mesenchymal Transition and Fibrosis. Front. Immunol. 2020, 11, 587581. [Google Scholar] [CrossRef] [PubMed]
- Allegra, A.; Tonacci, A.; Pioggia, G.; Musolino, C.; Gangemi, S. Anticancer activity of Rosmarinus officinalis L.: Mechanisms of Action and therapeutic potentials. Nutrients 2020, 12, 1739. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, A.H.; Zhang, F.; Dunlap, G.; Gomez-Rivas, E.; Watts, G.F.M.; Faust, H.J.; Rupani, K.V.; Mears, J.R.; Meednu, N.; Wang, R.; et al. Granzyme K+CD8 T cells form a core population in inflamed human tissue. Sci. Transl. Med. 2022, 14, eabo0686. [Google Scholar] [CrossRef] [PubMed]
- Saad, B.; AbouAtta, B.S.; Basha, W.; Hmade, A.; Kmail, A.; Khasib, S.; Said, O. Hypericum triquetrifolium—Derived factors downregulate the production levels of LPS-induced nitric oxide and tumor necrosis factor-αin THP-1 cells. Evid.-Based Complement. Altern. Med. 2011, 2011, 586470. [Google Scholar] [CrossRef]
- Caserta, S.; Innao, V.; Musolino, C.; Allegra, A. Immune checkpoint inhibitors in multiple myeloma: A review of the literature. Pathol.—Res. Pract. 2020, 216, 153114. [Google Scholar] [CrossRef]
- Singh, N.; Baby, D.; Rajguru, J.P.; Patil, P.B.; Thakkannavar, S.S.; Pujari, V.B. Inflammation and cancer. Ann. Afr. Med. 2019, 18, 121–126. [Google Scholar] [CrossRef]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Murata, M. Inflammation and cancer. Environ. Health Prev. Med. 2018, 23, 50. [Google Scholar] [CrossRef]
- Diakos, C.I.; Charles, K.A.; McMillan, D.C.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, e493–e503. [Google Scholar] [CrossRef]
- Khandia, R.; Munjal, A. Interplay between inflammation and cancer. Rep. Pract. Oncol. Radiother. 2019, 119, 199–245. [Google Scholar] [CrossRef]
- Handy, R.L.C.; Moore, P.K.; Handy, R.L.C.; Moore, P.K. A comparison of the effects ofL-NAME, 7-NI andL-NIL on carrageenan-induced hindpaw oedema and NOS activity. Br. J. Pharmacol. 1998, 123, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-E.; Son, J.E.; Jeong, H.; Kim, D.J.; Seo, S.G.; Lee, E.; Lim, T.G.; Kimbung, Y.R.; Chen, H.; Bode, A.M.; et al. A Novel Cinnamon-Related Natural Product with Pim-1 Inhibitory Activity Inhibits Leukemia and Skin Cancer. Cancer Res. 2015, 75, 2716–2728. [Google Scholar] [CrossRef] [PubMed]
- Samuels, Y.; Wang, Z.; Bardelli, A.; Silliman, N.; Ptak, J.; Szabo, S.; Yan, H.; Gazdar, A.; Powell, S.M.; Riggins, G.J.; et al. High Frequency of Mutations of the PIK3CA Gene in Human Cancers. Science 2004, 304, 554. [Google Scholar] [CrossRef]
- Cheng, J.Q.; Ruggeri, В.K. Amplification of AKT2 in human pancreatic cancer cells and inhibition of ATK2 expression and tumorigenicity by antisense RNA. Proc. Natl. Acad. Sci. USA 1996, 93, 3636–3641. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, B.A.; Huang, L.; Wood, M.; Cheng, J.Q.; Testa, J.R. Amplification and overexpression of the AKT2 oncogene in a subset of human pancreatic ductal adenocarcinomas. Mol. Carcinog. 1998, 21, 81–86. [Google Scholar] [CrossRef]
- Xia, P.; Xu, X.-Y. PI3K/Akt/mTOR signaling pathway in cancer stem cells: From basic research to clinical application. Am. J. Cancer Res. 2015, 5, 1602–1609. [Google Scholar]
- Jelic, M.; Mandic, A.; Maricic, S.; Srdjenovic, B. Oxidative stress and its role in cancer. J. Cancer Res. Ther. 2021, 17, 22–28. [Google Scholar] [CrossRef]
- Reuter, S.; Gupta, S.C.; Chaturvedi, M.M.; Aggarwal, B.B. Oxidative stress, inflammation, and cancer: How are they linked? Free Radic. Biol. Med. 2010, 49, 1603–1616. [Google Scholar] [CrossRef]
- Klaunig, J.E. Oxidative Stress and Cancer. Curr. Pharm. Des. 2020, 24, 4771–4778. [Google Scholar] [CrossRef]
- Kudryavtseva, A.V.; Krasnov, G.S.; Dmitriev, A.A.; Alekseev, B.Y.; Kardymon, O.L.; Sadritdinova, A.F.; Fedorova, M.S.; Pokrovsky, A.V.; Melnikova, N.V.; Kaprin, A.D.; et al. Mitochondrial dysfunction and oxidative stress in aging and cancer. Oncotarget 2016, 7, 44879–44905. [Google Scholar] [CrossRef]
- Sajadimajd, S.; Khazaei, M. Oxidative Stress and Cancer: The Role of Nrf2. Curr. Cancer Drug Targets 2018, 18, 538–557. [Google Scholar] [CrossRef] [PubMed]
- Sosa, V.; Moliné, T.; Somoza, R.; Paciucci, R.; Kondoh, H.; Lleonart, M.E. Oxidative stress and cancer: An overview. Ageing Res. Rev. 2013, 12, 376–390. [Google Scholar] [CrossRef] [PubMed]
- Chikara, S.; Nagaprashantha, L.D.; Singhal, J.; Horne, D.; Awasthi, S.; Singhal, S.S. Oxidative stress and dietary phytochemicals: Role in cancer chemoprevention and treatment. Cancer Lett. 2018, 413, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Caliri, A.W.; Tommasi, S.; Besaratinia, A. Relationships among smoking, oxidative stress, inflammation, macromolecular damage, and cancer. Mutat. Res. Mol. Mech. Mutagen. 2021, 787, 108365. [Google Scholar] [CrossRef]
- Dashti, G.R.; Assadollahi, V.; Parivar, K.; Roudbari, N.H.; Khalatbary, A.R.; Motamedi, M.; Ezatpour, B. The effect of aqueous cinnamon extract on the apoptotic process in acute myeloid leukemia HL-60 cells. Adv. Biomed. Res. 2013, 2, 25. [Google Scholar] [CrossRef]
- Alesci, A.; Nicosia, N.; Fumia, A.; Giorgianni, F.; Santini, A.; Cicero, N. Resveratrol and immune cells: A link to improve human health. Molecules 2022, 27, 424. [Google Scholar] [CrossRef]
- Murdaca, G.; Greco, M.; Tonacci, A.; Negrini, S.; Borro, M.; Puppo, F.; Gangemi, S. IL-33/IL-31 axis in immune-mediated and allergic diseases. Int. J. Mol. Sci. 2019, 20, 5856. [Google Scholar] [CrossRef]
- Mannucci, C.; Calapai, F.; Cardia, L.; Inferrera, G.; D’arena, G.; Di Pietro, M.; Navarra, M.; Gangemi, S.; Spagnolo, E.V.; Calapai, G. Clinical pharmacology of Citrus aurantium and Citrus sinensis for the treatment of anxiety. Evid.-Based Complement. Altern. Med. 2018, 2018, 3624094. [Google Scholar] [CrossRef]
- Innao, V.; Allegra, A.; Ginaldi, L.; Pioggia, G.; De Martinis, M.; Musolino, C.; Gangemi, S. Reviewing the significance of vitamin D substitution in monoclonal gammopathies. Int. J. Mol. Sci. 2021, 22, 4922. [Google Scholar] [CrossRef]
- Ferlazzo, N.; Cirmi, S.; Calapai, G.; Ventura-Spagnolo, E.; Gangemi, S.; Navarra, M. Anti-inflammatory activity of citrus bergamia derivatives: Where do we stand? Molecules 2016, 21, 1273. [Google Scholar] [CrossRef]
- Di Salvo, E.; Casciaro, M.; Giorgianni, C.M.; Cicero, N.; Gangemi, S. Age-related diseases and foods generating chlorinative stress. Antioxidants 2023, 12, 249. [Google Scholar] [CrossRef] [PubMed]
- Vitalini, S.; Nalbone, L.; Bernardi, C.; Iriti, M.; Costa, R.; Cicero, N.; Giarratana, F.; Vallone, L. Ginger and parsley essential oils: Chemical composition, antimicrobial activity, and evaluation of their application in cheese preservation. Nat. Prod. Res. 2022, 1–6. [Google Scholar] [CrossRef]
- Allegra, A.; Cicero, N.; Mirabile, G.; Cancemi, G.; Tonacci, A.; Musolino, C.; Gangemi, S. Critical role of aquaporins in cancer: Focus on hematological malignancies. Cancers 2022, 14, 4182. [Google Scholar] [CrossRef] [PubMed]
- Cicero, N.; Gangemi, S.; Allegra, A. Natural products and oxidative stress: Potential agents against multiple myeloma. Nat. Prod. Res. 2023, 37, 687–690. [Google Scholar] [CrossRef]
- Cicero, N.; Gervasi, T.; Durazzo, A.; Lucarini, M.; Macrì, A.; Nava, V.; Giarratana, F.; Tardugno, R.; Vadalà, R.; Santini, A. Mineral and microbiological analysis of spices and aromatic herbs. Foods 2022, 11, 548. [Google Scholar] [CrossRef] [PubMed]
- Cirmi, S.; Ferlazzo, N.; Lombardo, G.E.; Ventura-Spagnolo, E.; Gangemi, S.; Calapai, G.; Navarra, M. Neurodegenerative Diseases: Might citrus flavonoids play a protective role? Molecules 2016, 21, 1312. [Google Scholar] [CrossRef]
- Contino, M.; Leonardi, C.; Genovese, C.; Scalisi, E.M.; Pecoraro, R.; Ignoto, S.; Failla, C.; Ferruggia, G.; Salvaggio, A.; Asero, P.; et al. Antioxidant activity of two Opuntia Mill. species fruit extracts on human sperm quality after a freeze-thaw cycle. Nat. Prod. Res. 2022, 1–7. [Google Scholar] [CrossRef]
- Arlotta, C.; Toscano, V.; Genovese, C.; Calderaro, P.; Puglia, G.D.; Raccuia, S.A. Nutraceutical content and genetic diversity share a common pattern in new pomegranate genotypes. Molecules 2022, 27, 389. [Google Scholar] [CrossRef]
- Tibullo, D.; Caporarello, N.; Giallongo, C.; Anfuso, C.D.; Genovese, C.; Arlotta, C.; Puglisi, F.; Parrinello, N.L.; Bramanti, V.; Romano, A.; et al. Antiproliferative and Antiangiogenic Effects of Punica granatum Juice (PGJ) in Multiple Myeloma (MM). Nutrients 2016, 8, 611. [Google Scholar] [CrossRef]
- Allegra, A.; Petrarca, C.; Di Gioacchino, M.; Casciaro, M.; Musolino, C.; Gangemi, S. Modulation of cellular redox parameters for improving therapeutic responses in multiple myeloma. Antioxidants 2022, 11, 455. [Google Scholar] [CrossRef]
- Di Salvo, E.; Allegra, A.; Casciaro, M.; Gangemi, S. IL-31, itch and hematological malignancies. Clin. Mol. Allergy 2021, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Di Salvo, E.; Ventura-Spagnolo, E.; Casciaro, M.; Navarra, M.; Gangemi, S. IL-33/IL-31 Axis: A potential inflammatory pathway. Mediat. Inflamm. 2018, 2018, 3858032. [Google Scholar] [CrossRef] [PubMed]
- Borgia, F.; Custurone, P.; Pomi, F.L.; Cordiano, R.; Alessandrello, C.; Gangemi, S. IL-31: State of the art for an inflammation-oriented interleukin. Int. J. Mol. Sci. 2022, 23, 6507. [Google Scholar] [CrossRef] [PubMed]
- Di Gioacchino, M.; Della Valle, L.; Allegra, A.; Pioggia, G.; Gangemi, S. AllergoOncology: Role of immune cells and immune proteins. Clin. Transl. Allergy 2022, 12, e12133. [Google Scholar] [CrossRef]
- Di Salvo, E.; Casciaro, M.; Gangemi, S. IL-33 genetics and epigenetics in immune-related diseases. Clin. Mol. Allergy 2021, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Su, M.; Zhao, R.; Ouyang, H.; Dong, X.; Hu, P.; Pei, Q.; Lu, J.; Li, Z.; Zhang, C.; et al. Cinnamon effectively inhibits the activity of leukemia stem cells. Genet. Mol. Res. 2016, 15, 1–17. [Google Scholar] [CrossRef]
- Pelcovits, A.; Niroula, R. Acute myeloid leukemia: A review. Rhode Isl. Med. J. 2020, 103, 38–40. [Google Scholar]
- Allegra, A.; Spatari, G.; Mattioli, S.; Curti, S.; Innao, V.; Ettari, R.; Allegra, A.G.; Giorgianni, C.; Gangemi, S.; Musolino, C. Formaldehyde exposure and acute myeloid leukemia: A review of the literature. Medicina 2019, 55, 638. [Google Scholar] [CrossRef]
- Schoene, N.W.; Kelly, M.A.; Polansky, M.M.; Anderson, R.A. Water-soluble polymeric polyphenols from cinnamon inhibit proliferation and alter cell cycle distribution patterns of hematologic tumor cell lines. Cancer Lett. 2005, 230, 134–140. [Google Scholar] [CrossRef]
- Singh, G.; Maurya, S.; Delampasona, M.; Catalan, C.A. A comparison of chemical, antioxidant and antimicrobial studies of cinnamon leaf and bark volatile oils, oleoresins and their constituents. Food Chem. Toxicol. 2007, 45, 1650–1661. [Google Scholar] [CrossRef]
- Bukhari, S.; Siddique, M.H.; Naeem, A.; Khan, I.; Ali, Z.; Essa, A.; Fazal, F.; Anis, R.A.; Moran, L.; Sultan, A.; et al. Combined efficacy of Cinnamomum zeylanicum and doxorubicin against leukemia through regulation of TRAIL and NF-kappa B pathways in rat model. Mol. Biol. Rep. 2022, 49, 6495–6507. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, C.; Santos, R.X.; Cardoso, S.; Correia, S.; Oliveira, P.J.; Santos, M.S.; Moreira, P.I. Doxorubicin: The good, the bad and the ugly effect. Curr. Med. Chem. 2009, 16, 3267–3285. [Google Scholar] [CrossRef] [PubMed]
- Atale, N.; Gupta, S.; Yadav, U.; Rani, V. Cell-death assessment by fluorescent and nonfluorescent cytosolic and nuclear staining techniques. J. Microsc. 2014, 255, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Sederstrom, J.M. Assaying cell cycle status using flow cytometry. Curr. Protoc. Mol. Biol. 2015, 111, 28.6.1–28.6.11. [Google Scholar] [CrossRef]
- Lämmle, C.A.; Varady, A.; Müller, T.G.; Sturtzel, C.; Riepl, M.; Mathes, B.; Eichhorst, J.; Sporbert, A.; Lehmann, M.; Kräusslich, H.; et al. Photocaged hoechst enables subnuclear visualization and cell selective staining of DNA in vivo. ChemBioChem 2020, 22, 548–556. [Google Scholar] [CrossRef]
- Cooper, J.; Um, I.H.; Arandjelović, O.; Harrison, D.J. Lymphocyte classification from hoechst stained slides with deep learning. Cancers 2022, 14, 5957. [Google Scholar] [CrossRef]
- Lukinavičius, G.; Blaukopf, C.; Pershagen, E.; Schena, A.; Reymond, L.; Derivery, E.; Gonzalez-Gaitan, M.; D’este, E.; Hell, S.W.; Gerlich, D.W.; et al. SiR–Hoechst is a far-red DNA stain for live-cell nanoscopy. Nat. Commun. 2015, 6, 8497. [Google Scholar] [CrossRef]
- Weinberg, O.K.; Arber, D.A. Erythroleukemia: An Update. Curr. Oncol. Rep. 2021, 23, 69. [Google Scholar] [CrossRef]
- Al-Rawashde, F.A.; Taib, W.R.W.; Ismail, I.; Johan, M.F.; Al-Wajeeh, A.S.; Al-Jamal, H.A.N. Thymoquinone induces downregulation of BCR-ABL/JAK/STAT pathway and apoptosis in K562 leukemia cells. Asian Pac. J. Cancer Prev. 2021, 22, 3959–3965. [Google Scholar] [CrossRef]
- Tian, Z.; Yang, L.; Huang, M.; Sun, C.; Chen, M.; Zhao, W.; Peng, J.; Guo, G. Antitumor activity and mechanism of action of the antimicrobial peptide AMP-17 on human leukemia K562 cells. Molecules 2022, 27, 8109. [Google Scholar] [CrossRef]
- Yu, C.-H.; Yang, S.-Q.; Li, L.; Xin, Y.; Zhang, F.; Liu, X.-F.; Yi, Z.-C. Identification of potential pathways and microRNA-mRNA networks associated with benzene metabolite hydroquinone-induced hematotoxicity in human leukemia K562 cells. BMC Pharmacol. Toxicol. 2022, 23, 20. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Z.; Polski, J.M.; Kasyan, A.; Medeiros, L.J. Acute erythroid leukemia. Arch. Pathol. Lab. Med. 2010, 134, 1261–1270. [Google Scholar] [CrossRef] [PubMed]
- Nir, Y.; Potasman, I.; Stermer, E.; Tabak, M.; Neeman, I. Controlled trial of the effect of cinnamon extract on Helicobacter pylori. Helicobacter 2000, 5, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, S. Helicobacter pyloriand gastric mucosa-associated lymphoid tissue lymphoma: Recent progress in pathogenesis and management. World J. Gastroenterol. 2013, 19, 8181–8187. [Google Scholar] [CrossRef] [PubMed]
- Pohl, D.; Keller, P.M.; Bordier, V.; Wagner, K. Review of current diagnostic methods and advances in Helicobacter pylori diagnostics in the era of next generation sequencing. World J. Gastroenterol. 2019, 25, 4629–4660. [Google Scholar] [CrossRef]
- Zucca, E.; Bertoni, F. The spectrum of MALT lymphoma at different sites: Biological and therapeutic relevance. Blood 2016, 127, 2082–2092. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-C. Treatment of Helicobacter pylori infection: Current status and future concepts. World J. Gastroenterol. 2014, 20, 5283–5293. [Google Scholar] [CrossRef]
- De Brito, B.B.; da Silva, F.A.F.; Soares, A.S.; Pereira, V.A.; Santos, M.L.C.; Sampaio, M.M.; Neves, P.H.M.; de Melo, F.F. Pathogenesis and clinical management of Helicobacter pylori gastric infection. World J. Gastroenterol. 2019, 25, 5578–5589. [Google Scholar] [CrossRef]
- Deschler, B.; Lübbert, M. Acute myeloid leukemia: Epidemiology and etiology. Cancer 2006, 107, 2099–2107. [Google Scholar] [CrossRef]
- Rahmé, R.; Adès, L.; Thomas, X.; Guerci-Bresler, A.; Pigneux, A.; Vey, N.; Raffoux, E.; Castaigne, S.; Spertini, O.; Wittnebel, S.; et al. Reducing mortality in newly diagnosed standard-risk acute promyelocytic leukemia in elderly patients treated with arsenic trioxide requires major reduction of chemotherapy: A report by the French Belgian Swiss APL group (APL 2006 trial). Haematologica 2018, 103, e519–e521. [Google Scholar] [CrossRef]
- Tawfik, B.; Pardee, T.S.; Isom, S.; Sliesoraitis, S.; Winter, A.; Lawrence, J.; Powell, B.L.; Klepin, H.D. Comorbidity, age, and mortality among adults treated intensively for acute myeloid leukemia (AML). J. Geriatr. Oncol. 2016, 7, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Rajamäki, A.; Hujo, M.; Sund, R.; Prusila, R.E.I.; Kuusisto, M.E.L.; Kuitunen, H.; Jantunen, E.; Mercadal, S.; Sorigue, M.; Sancho, J.; et al. Mortality among patients with low-grade follicular lymphoma: A binational retrospective analysis. Cancer 2022, 128, 2474–2482. [Google Scholar] [CrossRef] [PubMed]
- Boyne, D.J.; Mickle, A.T.; Brenner, D.R.; Friedenreich, C.; Cheung, W.Y.; Tang, K.L.; Wilson, T.A.; Lorenzetti, D.L.; James, M.T.; Ronksley, P.E.; et al. Long-term risk of cardiovascular mortality in lymphoma survivors: A systematic review and meta-analysis. Cancer Med. 2018, 7, 4801–4813. [Google Scholar] [CrossRef]
- Imbesi, S.; Musolino, C.; Allegra, A.; Saija, A.; Morabito, F.; Calapai, G.; Gangemi, S. Oxidative stress in oncohematologic diseases: An update. Expert Rev. Hematol. 2013, 6, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Christidi, E.; Brunham, L.R. Regulated cell death pathways in doxorubicin-induced cardiotoxicity. Cell Death Dis. 2021, 12, 339. [Google Scholar] [CrossRef] [PubMed]
- Tadokoro, T.; Ikeda, M.; Ide, T.; Deguchi, H.; Ikeda, S.; Okabe, K.; Ishikita, A.; Matsushima, S.; Koumura, T.; Yamada, K.-I.; et al. Mitochondria-dependent ferroptosis plays a pivotal role in doxorubicin cardiotoxicity. J. Clin. Investig. 2020, 5, e132747. [Google Scholar] [CrossRef] [PubMed]
- Yahfoufi, N.; Alsadi, N.; Jambi, M.; Matar, C. The immunomodulatory and anti-inflammatory role of polyphenols. Nutrients 2018, 10, 1618. [Google Scholar] [CrossRef]
- Carpten, J.D.; Faber, A.L.; Horn, C.; Donoho, G.P.; Briggs, S.L.; Robbins, C.M.; Hostetter, G.; Boguslawski, S.; Moses, T.Y.; Savage, S.; et al. A transforming mutation in the pleckstrin homology domain of AKT1 in cancer. Nature 2007, 448, 439–444. [Google Scholar] [CrossRef]
- Pugh, C.W.; Ratcliffe, P.J. Regulation of angiogenesis by hypoxia: Role of the HIF system. Nat. Med. 2003, 9, 677–684. [Google Scholar] [CrossRef]
- Semenza, G.L. Targeting HIF-1 for cancer therapy. Nat. Rev. Cancer 2003, 3, 721–732. [Google Scholar] [CrossRef]
- Harris, B.; Saleem, S.; Cook, N.; Searle, E. Targeting hypoxia in solid and haematological malignancies. J. Exp. Clin. Cancer Res. 2022, 41, 318. [Google Scholar] [CrossRef] [PubMed]



| Exposure time (h) | 24 | 48 | 72 |
| Cell inhibition (%) | 74.60 | 85.50 | 90.10 |
| Study Title | Conditions | NCT Number |
|---|---|---|
| Improving Insulin Resistance in Gynecological Cancer Patients | Insulin Resistance | NCT04139694 |
| A Dose Escalation Study of the Safety and Pharmacokinetics of GSK1363089 (Formerly XL880) Administered Orally to Subjects with Solid Tumors | Solid Tumors | NCT00742131 |
| RSYR for Fatigue Reduction in Cancer Fatigue Caused by Chemotherapy | Cancer-related Problems/Conditions | NCT05229029 |
| Gustatory Function Following Radiotherapy to the Head and Neck | Head and Neck Cancer | NCT03738657 |
| The Effect of Cinnamon on Ovulation Induction in Women with Polycystic Ovary Syndrome | Polycystic Ovary Syndrome | NCT03778099 |
| Cinnamon Extract on Menstrual Cycles in PolyCystic Ovary Syndrome (PCOS) | Polycystic Ovary Syndrome | NCT01483118 |
| The Effect of Cinnamon Extract on Insulin Resistance Parameters in Polycystic Ovary Syndrome: A Pilot Study | Polycystic Ovary Syndrome | NCT00331279 |
| Effect of Cinnamon Extract on Insulin Resistance in Polycystic Ovary Syndrome | Polycystic Ovary Syndrome | NCT00970541 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caserta, S.; Genovese, C.; Cicero, N.; Gangemi, S.; Allegra, A. The Anti-Cancer Effect of Cinnamon Aqueous Extract: A Focus on Hematological Malignancies. Life 2023, 13, 1176. https://doi.org/10.3390/life13051176
Caserta S, Genovese C, Cicero N, Gangemi S, Allegra A. The Anti-Cancer Effect of Cinnamon Aqueous Extract: A Focus on Hematological Malignancies. Life. 2023; 13(5):1176. https://doi.org/10.3390/life13051176
Chicago/Turabian StyleCaserta, Santino, Claudia Genovese, Nicola Cicero, Sebastiano Gangemi, and Alessandro Allegra. 2023. "The Anti-Cancer Effect of Cinnamon Aqueous Extract: A Focus on Hematological Malignancies" Life 13, no. 5: 1176. https://doi.org/10.3390/life13051176