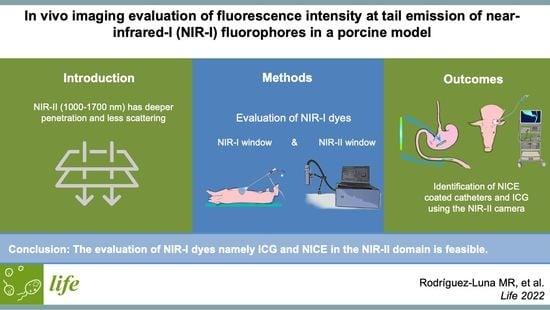
In Vivo Imaging Evaluation of Fluorescence Intensity at Tail Emission of Near-Infrared-I (NIR-I) Fluorophores in a Porcine Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. ICG Dye Preparation
2.2. Fluorescent NICE-Coated Catheter Preparation
2.3. Operating Setup and Experimental Workflow
Animal Model
2.4. Post-Processing Fluorescence Analyses
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hirche, C.; Engel, H.; Kolios, L.; Cognie, J.; Hünerbein, M.; Lehnhardt, M.; Kremer, T. An experimental study to evaluate the fluobeam 800 imaging system for fluorescence-guided lymphatic imaging and sentinel node biopsy. Surg. Innov. 2013, 20, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, S.; Tokuishi, K.; Anami, K.; Miyawaki, M.; Moroga, T.; Kamei, M.; Suehiro, S.; Ono, K.; Takeno, S.; Chujo, M.; et al. Video-assisted thoracoscopic indocyanine green fluorescence imaging system shows sentinel lymph nodes in non-small-cell lung cancer. J. Thorac. Cardiovasc. Surg. 2011, 141, 141–144. [Google Scholar] [CrossRef] [Green Version]
- Meershoek, P.; KleinJan, G.H.; van Willigen, D.M.; Bauwens, K.P.; Spa, S.J.; van Beurden, F.; van Gennep, E.J.; Mottrie, A.M.; van der Poel, H.G.; Buckle, T.; et al. Multi-wavelength fluorescence imaging with a da Vinci Firefly—A technical look behind the scenes. J. Robot. Surg. 2020, 15, 751–760. [Google Scholar] [CrossRef]
- Bsc, L.V.M.; Handgraaf, H.J.M.; Diana, M.; Dijkstra, J.; Ishizawa, T.; Vahrmeijer, A.L.; Mieog, J.S.D. A practical guide for the use of indocyanine green and methylene blue in fluorescence-guided abdominal surgery. J. Surg. Oncol. 2018, 118, 283–300. [Google Scholar] [CrossRef] [Green Version]
- Frangioni, J.V. In vivo near-infrared fluorescence imaging. Curr. Opin. Chem. Biol. 2003, 7, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Eich, C.; Cruz, L.J. Recent Advances in Rare-Earth-Doped Nanoparticles for NIR-II Imaging and Cancer Theranostics. Front. Chem. 2020, 8, 496. [Google Scholar] [CrossRef] [PubMed]
- Vahrmeijer, A.L.; Hutteman, M.; Van Der Vorst, J.R.; Van De Velde, C.J.H.; Frangioni, J.V. Image-guided cancer surgery using near-infrared fluorescence. Nat. Rev. Clin. Oncol. 2013, 10, 507–518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FDA. Drugs @ FDA: FDA-Approved Drugs. In Prod. Inser. Indocyanine Green. 2021. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&applno=011525 (accessed on 14 February 2021).
- Diana, M.; Agnus, V.; Halvax, P.; Liu, Y.-Y.; Dallemagne, B.; Schlagowski, A.-I.; Geny, B.; Diemunsch, P.; Lindner, V.; Marescaux, J. Intraoperative fluorescence-based enhanced reality laparoscopic real-time imaging to assess bowel perfusion at the anastomotic site in an experimental model. Br. J. Surg. 2015, 102, e169–e176. [Google Scholar] [CrossRef] [PubMed]
- Spota, A.; Al-Taher, M.; Felli, E.; Conde, S.M.; Dal Dosso, I.; Moretto, G.; Spinoglio, G.; Baiocchi, G.; Vilallonga, R.; Impellizzeri, H.; et al. Fluorescence-based bowel anastomosis perfusion evaluation: Results from the IHU-IRCAD-EAES EURO-FIGS registry. Surg. Endosc. 2021, 35, 7142–7153. [Google Scholar] [CrossRef]
- Zhu, S.; Yung, B.C.; Chandra, S.; Niu, G.; Antaris, A.L.; Chen, X. Near-Infrared-II (NIR-II) Bioimaging via Off-Peak NIR-I Fluorescence Emission. Theranostics 2018, 8, 4141–4151. [Google Scholar] [CrossRef]
- Starosolski, Z.; Bhavane, R.; Ghaghada, K.B.; Vasudevan, S.A.; Kaay, A.; Annapragada, A. Indocyanine green fluorescence in second near-infrared (NIR-II) window. PLoS ONE 2017, 12, e0187563. [Google Scholar] [CrossRef]
- Kilkenny, C.; Browne, W.J.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Improving Bioscience Research Reporting: The ARRIVE Guidelines for Reporting Animal Research. PLoS Biol. 2010, 8, e1000412. [Google Scholar] [CrossRef] [PubMed]
- Prescott, M.J.; Lidster, K. Improving quality of science through better animal welfare: The NC3Rs strategy. Lab. Anim. 2017, 46, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Barberio, M.; Pizzicannella, M.; Spota, A.; Ashoka, A.H.; Agnus, V.; Al Taher, M.; Jansen-Winkeln, B.; Gockel, I.; Marescaux, J.; Swanström, L.; et al. Preoperative endoscopic marking of the gastrointestinal tract using fluorescence imaging: Submucosal indocyanine green tattooing versus a novel fluorescent over-the-scope clip in a survival experimental study. Surg. Endosc. 2020, 35, 5115–5123. [Google Scholar] [CrossRef]
- Ashoka, A.H.; Kong, S.-H.; Seeliger, B.; Andreiuk, B.; Soares, R.V.; Barberio, M.; Diana, M.; Klymchenko, A.S. Near-infrared fluorescent coatings of medical devices for image-guided surgery. Biomaterials 2020, 261, 120306. [Google Scholar] [CrossRef] [PubMed]
- Barberio, M.; Al-Taher, M.; Felli, E.; Ashoka, A.H.; Marescaux, J.; Klymchenko, A.; Diana, M. Intraoperative ureter identification with a novel fluorescent catheter. Sci. Rep. 2021, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, R.; Barberio, M.; Kanaji, S.; Lapergola, A.; Ashoka, A.H.; Andreiuk, B.; Guerriero, L.; Pizzicannella, M.; Seeliger, B.; Saida, Y.; et al. Hybrid fluorescent magnetic gastrojejunostomy: An experimental feasibility study in the porcine model and human cadaver. Surg. Endosc. 2019, 34, 1393–1400. [Google Scholar] [CrossRef] [PubMed]
- Barberio, M.; Al-Taher, M.; Forgione, A.; Ashoka, A.H.; Felli, E.; Agnus, V.; Marescaux, J.; Klymchenko, A.; Diana, M. A novel method for near-infrared fluorescence imaging of the urethra during perineal and transanal surgery: Demonstration in a cadaveric model. Color. Dis. 2020, 22, 1749–1753. [Google Scholar] [CrossRef] [PubMed]
- Šafranko, S.; Stanković, A.; Hajra, S.; Kim, H.-J.; Strelec, I.; Dutour-Sikirić, M.; Weber, I.; Bosnar, M.H.; Grbčić, P.; Pavelić, S.K.; et al. Preparation of Multifunctional N-Doped Carbon Quantum Dots from Citrus clementina Peel: Investigating Targeted Pharmacological Activities and the Potential Application for Fe3+ Sensing. Pharmaceuticals 2021, 14, 857. [Google Scholar] [CrossRef]
- Zhu, S.; Tian, R.; Antaris, A.L.; Chen, X.; Dai, H. Near-Infrared-II Molecular Dyes for Cancer Imaging and Surgery. Adv. Mater. 2019, 31, e1900321. [Google Scholar] [CrossRef]
- Buddingh, K.T.; Nieuwenhuijs, V.B.; van Buuren, L.; Hulscher, J.B.F.; de Jong, J.S.; van Dam, G.M. Intraoperative assessment of biliary anatomy for prevention of bile duct injury: A review of current and future patient safety interventions. Surg. Endosc. 2011, 25, 2449–2461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, S.; Yu, Y.; Wang, Z.; Wu, Y.; Qiu, X.; Jian, C.; Yu, A. NIR-II Fluorescence Imaging Using Indocyanine Green Provides Early Prediction of Skin Avulsion-Injury in a Porcine Model. Clin. Cosmet. Investig. Dermatol. 2022, 15, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Fang, C.; Li, B.; Zhang, Z.; Cao, C.; Cai, M.; Su, S.; Sun, X.; Shi, X.; Li, C.; et al. First-in-human liver-tumour surgery guided by multispectral fluorescence imaging in the visible and near-infrared-I/II windows. Nat. Biomed. Eng. 2020, 4, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Chen, L.; Huang, Z.; Qiu, H.; Yu, B. Neutrophils injure gallbladder interstitial Cajal-like cells in a guinea pig model of acute cholecystitis. J. Cell. Physiol. 2019, 234, 4291–4301. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Sevick-Muraca, E.M. A review of performance of near-infrared fluorescence imaging devices used in clinical studies. Br. J. Radiol. 2015, 88, 20140547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oduor, P.; Mizuno, G.; Lewis, J. Strategic options towards an affordable high-performance infrared camera. Image Sens. Technol. Mater. Devices Syst. Appl. III 2016, 9854, 98540F. [Google Scholar] [CrossRef]



| NIR-I Window | NIR-II Window | p Value | |
|---|---|---|---|
| Endoluminal NICE-coated catheters in the small bowel | 0.34 ± 0.007 a.u. | 0.14 ± 0.106 a.u. | p = 0.111 |
| Endoluminal NICE-coated catheters in the stomach | 0.26 ± 0.156 a.u. | 0.09 ± 0.039 a.u. | p = 0.248 |
| CBD after intravenous ICG injection | t5 0.52 ± 0.198 a.u. | 0.12 ± 0.027 a.u. | p = 0.101 |
| t35 0.54 ± 0.216 a.u | 0.18 ± 0.100 a.u | p = 0.129 | |
| t65 0.62 ± 0.251 a.u. | 0.22 ± 0.041 a.u. | p = 0.151 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Luna, M.R.; Okamoto, N.; Al-Taher, M.; Keller, D.S.; Cinelli, L.; Hoskere Ashoka, A.; Klymchenko, A.S.; Marescaux, J.; Diana, M. In Vivo Imaging Evaluation of Fluorescence Intensity at Tail Emission of Near-Infrared-I (NIR-I) Fluorophores in a Porcine Model. Life 2022, 12, 1123. https://doi.org/10.3390/life12081123
Rodríguez-Luna MR, Okamoto N, Al-Taher M, Keller DS, Cinelli L, Hoskere Ashoka A, Klymchenko AS, Marescaux J, Diana M. In Vivo Imaging Evaluation of Fluorescence Intensity at Tail Emission of Near-Infrared-I (NIR-I) Fluorophores in a Porcine Model. Life. 2022; 12(8):1123. https://doi.org/10.3390/life12081123
Chicago/Turabian StyleRodríguez-Luna, María Rita, Nariaki Okamoto, Mahdi Al-Taher, Deborah S. Keller, Lorenzo Cinelli, Anila Hoskere Ashoka, Andrey S. Klymchenko, Jacques Marescaux, and Michele Diana. 2022. "In Vivo Imaging Evaluation of Fluorescence Intensity at Tail Emission of Near-Infrared-I (NIR-I) Fluorophores in a Porcine Model" Life 12, no. 8: 1123. https://doi.org/10.3390/life12081123