Indirect Nutrition and Mobility Risks during Hospitalization: An Architectural Perspective on the nutritionDay Study Findings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Method
2.2. Sample and Data Analysis
3. Results
3.1. Demographics
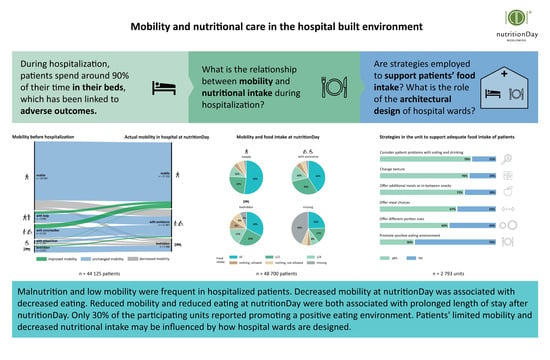
3.2. Mobility, Nutritional Intake, and Well-Being
4. Discussion
4.1. Main Findings and Their Implications
4.2. Ward and Hospital Design Challenges
4.3. Future Research Directions
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Przesmycka, N. Contemporary Trends in the Design of Hospital Wards in the Context of Ergonomic Issues. In Ergonomics for People with Disabilities; Walter de Gruyter GmbH & Co KG: Berlin, Germany, 2018; pp. 85–100. [Google Scholar] [CrossRef]
- Alalouch, C.; Aspinall, P.; Smith, H. Architects’ Priorities for Hospital-Ward Design Criteria: Application of Choice-Based Conjoint Analysis in Architectural Research. J. Archit. Plann. Res. 2015, 32, 1–22. [Google Scholar]
- Dixon, R.; Goodman, H.; Noakes, T. Health Service Buildings. In The Architects’ Handbook; Pickard, Q., Ed.; Blackwell Science Ltd.: Oxford, UK, 2002; pp. 108–136. [Google Scholar]
- Zisberg, A.; Syn-hershko, A. Factors Related to the Mobility of Hospitalized Older Adults: A Prospective Cohort Study. Geriatr. Nurs. 2016, 37, 96–100. [Google Scholar] [CrossRef]
- Brown, C.J.; Friedkin, R.J.; Inouye, S.K. Prevalence and Outcomes of Low Mobility in Hospitalized Older Patients. J. Am. Geriatr. Soc. 2004, 52, 1263–1270. [Google Scholar] [CrossRef]
- Charlton, K.E.; Nichols, C.; Bowden, S.; Lambert, K.; Barone, L.; Mason, M.; Milosavljevic, M. Older Rehabilitation Patients Are at High Risk of Malnutrition. J. Nutr. Health Aging 2010, 14, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Ferguson, M.; Banks, M.; Batterham, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and Poor Food Intake Are Associated with Prolonged Hospital Stay, Frequent Readmissions, and Greater in-Hospital Mortality: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2013, 32, 737–745. [Google Scholar] [CrossRef] [Green Version]
- Correia, M.I.T.D.; Waitzberg, D.L. The Impact of Malnutrition on Morbidity, Mortality, Length of Hospital Stay and Costs Evaluated through a Multivariate Model Analysis. Clin. Nutr. 2003, 22, 235–239. [Google Scholar] [CrossRef]
- Hiesmayr, M.; Schindler, K.; Pernicka, E.; Schuh, C.; Schoeniger-Hekele, A.; Bauer, P.; Laviano, A.; Lovell, A.D.; Mouhieddine, M.; Schuetz, T.; et al. Decreased Food Intake Is a Risk Factor for Mortality in Hospitalised Patients: The NutritionDay Survey 2006. Clin. Nutr. 2009, 28, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Barker, L.A.; Gout, B.S.; Crowe, T.C. Hospital Malnutrition: Prevalence, Identification and Impact on Patients and the Healthcare System. Int. J. Environ. Res. Public Health 2011, 8, 514–527. [Google Scholar] [CrossRef] [Green Version]
- Baptiste, F.; Egan, M.; Dubouloz-Wilner, C.J. Geriatric Rehabilitation Patients’ Perceptions of Unit Dining Locations. Can. Geriatr. J. 2014, 17, 38–44. [Google Scholar] [CrossRef] [Green Version]
- Eurostat. Hospital Discharges and Average Length of Stay; OECD iLibrary: Berlin, Germany, 2022; pp. 1–17. [CrossRef]
- Wilson, A.; Evans, S.; Frost, G. A Comparison of the Amount of Food Served and Consumed According to Meal Service System. J. Hum. Nutr. Diet. 2000, 13, 271–275. [Google Scholar] [CrossRef]
- Baldwin, C.; Kimber, K.; Gibbs, M.; Weekes, C. Supportive Interventions for Enhancing Dietary Intake in Malnourished or Nutritionally At-Risk Adults. Cochrane Database Syst. Rev. 2016, 12, CD009840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Association, H.C. Protected Mealtimes Policy; Emerald Group Publishing Limited: London, UK, 2004; Volume 40. [Google Scholar] [CrossRef]
- Porter, J.; Haines, T.P.; Truby, H. The Efficacy of Protected Mealtimes in Hospitalised Patients: A Stepped Wedge Cluster Randomised Controlled Trial. BMC Med. 2017, 15, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porter, J.; Ottrey, E.; Huggins, C.E. Protected Mealtimes in Hospitals and Nutritional Intake: Systematic Review and Meta-Analyses. Int. J. Nurs. Stud. 2017, 65, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Hickson, M.; Connolly, A.; Whelan, K. Impact of Protected Mealtimes on Ward Mealtime Environment, Patient Experience and Nutrient Intake in Hospitalised Patients. J. Hum. Nutr. Diet. 2011, 24, 370–374. [Google Scholar] [CrossRef]
- Huxtable, S.; Palmer, M. The Efficacy of Protected Mealtimes in Reducing Mealtime Interruptions and Improving Mealtime Assistance in Adult Inpatients in an Australian Hospital. Eur. J. Clin. Nutr. 2013, 67, 904–910. [Google Scholar] [CrossRef]
- Hope, K.; Ferguson, M.; Reidlinger, D.P.; Agarwal, E. “I Don’t Eat When I’m Sick”: Older People’s Food and Mealtime Experiences in Hospital. Maturitas 2017, 97, 6–13. [Google Scholar] [CrossRef]
- Naithani, S.; Whelan, K.; Thomas, J.; Gulliford, M.C.; Morgan, M. Hospital Inpatients’ Experiences of Access to Food: A Qualitative Interview and Observational Study. Health Expect. 2008, 11, 294–303. [Google Scholar] [CrossRef] [Green Version]
- Markovski, K.; Nenov, A.; Ottaway, A.; Skinner, E. Does Eating Environment Have an Impact on the Protein and Energy Intake in the Hospitalised Elderly? Nutr. Diet. 2017, 74, 224–228. [Google Scholar] [CrossRef]
- Buckinx, F.; Reginster, J.Y.; Morelle, A.; Paquot, N.; Labeye, N.; Locquet, M.; Adam, S.; Bruyère, O. Influence of Environmental Factors on Food Intake among Nursing Home Residents: A Survey Combined with a Video Approach. Clin. Interv. Aging 2017, 12, 1055–1064. [Google Scholar] [CrossRef] [Green Version]
- Keller, H.H.; Carrier, N.; Slaughter, S.; Lengyel, C.; Steele, C.M.; Duizer, L.; Brown, K.S.; Chaudhury, H.; Yoon, M.N.; Duncan, A.M.; et al. Making the Most of Mealtimes (M3): Protocol of a Multi-Centre Cross-Sectional Study of Food Intake and Its Determinants in Older Adults Living in Long Term Care Homes. BMC Geriatr. 2017, 17, 15. [Google Scholar] [CrossRef] [Green Version]
- McLaren-Hedwards, T.; D’cunha, K.; Elder-Robinson, E.; Smith, C.; Jennings, C.; Marsh, A.; Young, A. Effect of Communal Dining and Dining Room Enhancement Interventions on Nutritional, Clinical and Functional Outcomes of Patients in Acute and Sub-Acute Hospital, Rehabilitation and Aged-Care Settings: A Systematic Review. Nutr. Diet. 2022, 79, 140–168. [Google Scholar] [CrossRef] [PubMed]
- Hartwell, H.J.; Shepherd, P.A.; Edwards, J.S.A. Effects of a Hospital Ward Eating Environment on Patients’ Mealtime Experience: A Pilot Study. Nutr. Diet. 2013, 70, 332–338. [Google Scholar] [CrossRef]
- Wright, L.; Hickson, M.; Frost, G. Eating Together Is Important: Using a Dining Room in an Acute Elderly Medical Ward Increases Energy Intake. J. Hum. Nutr. Diet. 2006, 19, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Greysen, S.R.; Patel, M.S. Inpatient Notes: Bedrest Is Toxic—Why Mobility Matters in the Hospital. Ann. Intern. Med. 2018, 169, HO2–HO3. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.J.; Redden, Ã.D.T.; Flood, Ã.K.L.; Allman, R.M. The Underrecognized Epidemic of Low Mobility During Hospitalization of Older Adults. J. Am. Geriatr. Soc. 2009, 57, 1660–1665. [Google Scholar] [CrossRef] [PubMed]
- Pavon, J.M.; Sloane, R.J.; Pieper, C.F.; Colón-Emeric, C.S.; Cohen, H.J.; Gallagher, D.; Hall, K.S.; Morey, M.C.; McCarty, M.; Hastings, S.N. Accelerometer-Measured Hospital Physical Activity and Hospital-Acquired Disability in Older Adults. J. Am. Geriatr. Soc. 2020, 68, 261–265. [Google Scholar] [CrossRef]
- Greysen, S.R.; Hoi-Cheung, D.; Garcia, V.; Kessell, E.; Sarkar, U.; Goldman, L.; Schneidermann, M.; Critchfield, J.; Pierluissi, E.; Kushel, M. “missing Pieces”—Functional, Social, and Environmental Barriers to Recovery for Vulnerable Older Adults Transitioning from Hospital to Home. J. Am. Geriatr. Soc. 2014, 62, 1556–1561. [Google Scholar] [CrossRef] [Green Version]
- Kirk, J.W.; Bodilsen, A.C.; Sivertsen, D.M.; Husted, R.S.; Nilsen, P.; Tjørnhøj-Thomsen, T. Disentangling the Complexity of Mobility of Older Medical Patients in Routine Practice: An Ethnographic Study in Denmark. PLoS ONE 2019, 14, e0214271. [Google Scholar] [CrossRef]
- Zisberg, A.; Agmon, M.; Gur-Yaish, N.; Rand, D.; Hayat, Y.; Gil, E. No One Size Fits All—The Development of a Theory-Driven Intervention to Increase in-Hospital Mobility: The “ WALK-FOR ” Study. BMC Geriatr. 2018, 18, 91. [Google Scholar] [CrossRef] [Green Version]
- Boltz, M.; Capezuti, E.; Shabbat, N. Nursing Staff Perceptions of Physical Function in Hospitalized Older Adults. Appl. Nurs. Res. 2011, 24, 215–222. [Google Scholar] [CrossRef]
- Brown, C.J.; Williams, B.R.; Woodby, L.L.; Davis, L.L.; Allman, R.M. Barriers to Mobility During Hospitalization from the Perspectives of Older Patients and Their Nurses and Physicians. J. Hosp. Med. 2007, 2, 305–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- So, C.; Pierluissi, E. Attitudes and Expectations Regarding Exercise in the Hospital of Hospitalized Older Adults: A Qualitative Study. J. Am. Geriatr. Soc. 2012, 60, 713–718. [Google Scholar] [CrossRef]
- Nutrition Day. Nutritionday Worldwide. Available online: https://www.nutritionday.org/en/-35-.languages/languages.html (accessed on 30 November 2022).
- Kortebein, P.; Symons, T.B.; Ferrando, A.; Paddon-Jones, D.; Ronsen, O.; Protas, E.; Conger, S.; Lombeida, J.; Wolfe, R.; Evans, W.J. Functional Impact of 10 Days of Bed Rest in Healthy Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 1076–1081. [Google Scholar] [CrossRef] [Green Version]
- Walton, K.; Williams, P.; Tapsell, L.; Hoyle, M.; Shen, Z.W.; Gladman, L.; Nurka, M. Observations of Mealtimes in Hospital Aged Care Rehabilitation Wards. Appetite 2013, 67, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Young, C.; Farrah, K. Room Service Food Delivery Models for Hospital In-Patients: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, USA, 2019; Available online: http://europepmc.org/books/NBK545103 (accessed on 30 November 2022).
- Edwards, D.; Carrier, J.; Hopkinson, J. Assistance at Mealtimes in Hospital Settings and Rehabilitation Units for Patients (>65 Years) from the Perspective of Patients, Families and Healthcare Professionals: A Mixed Methods Systematic Review. Int. J. Nurs. Stud. 2017, 69, 100–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitelock, G.; Aromataris, E. Effectiveness of Mealtime Interventions to Improve Nutritional Intake of Adult Patients in the Acute Care Setting: A Systematic Review. JBI Evid. Synth. 2013, 11, 263–305. [Google Scholar] [CrossRef] [Green Version]
- Zisberg, A.; Shadmi, E.; Gur-Yaish, N.; Tonkikh, O.; Sinoff, G. Hospital-Associated Functional Decline: The Role of Hospitalization Processes Beyond Individual Risk Factors. J. Am. Geriatr. Soc. 2015, 63, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Covinsky, K.E.; Pierluissi, E.; Johnston, C.B. Hospitalization-Associated Disability “She Was Probably Able to Ambulate, but I’m Not Sure”. JAMA J. Am. Med. Assoc. 2011, 306, 1782–1793. [Google Scholar] [CrossRef]
- Jong, J.; Porter, J.; Palermo, C.; Ottrey, E. Meals beyond the Bedside: An Ethnographic Exploration of Staffs’ Perspectives and Experiences of Communal Dining in Subacute Care. Nurs. Health Sci. 2021, 23, 372–380. [Google Scholar] [CrossRef]
- Kevdzija, M.; Marquardt, G. Stroke Patients’ Nonscheduled Activity during Inpatient Rehabilitation and Its Relationship with the Architectural Layout: A Multicenter Shadowing Study. Top. Stroke Rehabil. 2022, 29, 9–15. [Google Scholar] [CrossRef]
- Agmon, M.; Zisberg, A.; Gil, E.; Rand, D.; Gur-Yaish, N.; Azriel, M. Association Between 900 Steps a Day and Functional Decline in Older Hospitalized Patients. JAMA Intern. Med. 2017, 177, 272–274. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.D.M.; Snaith, P.A. The Social Behaviour of Geriatric Patients at Mealtimes: An Observational and an Intervention Study. Age Ageing 1980, 9, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Palmer, R.M.; Counsell, S.; Landefeld, C.S. Clinical Intervention Trials: The ACE Unit. Clin. Geriatr. Med. 1998, 14, 831–849. [Google Scholar] [CrossRef] [PubMed]
- Feenstra, F. Reactivating Hospital, Active Patients Through Special Design. HERD Health Environ. Res. Des. J. 2021, 14, 87–105. [Google Scholar] [CrossRef]
- Ragneskog, H.; Bråne, G.; Karlsson, I.; Kihlgren, M. Influence of Dinner Music on Food Intake and Symptoms Common in Dementia. Scand. J. Caring Sci. 1996, 10, 11–17. [Google Scholar] [CrossRef]
- Richeson, N.E.; Neil, D.J. Therapeutic Recreation Music Intervention to Decrease Mealtime Agitation and Increase Food Intake in Older Adults With Dementia. Am. J. Recreat. Ther. 2004, 3, 37–41. [Google Scholar]
- Thomas, D.W.; Smith, M. The Effect of Music on Caloric Consumption among Nursing Home Residents with Dementia of the Alzheimer’s Type. Act. Adapt. Aging 2009, 33, 1–16. [Google Scholar] [CrossRef]
- Edwards, N.E.; Beck, A.M. Animal-Assisted Therapy and Nutrition in Alzheimer’s Disease. West J. Nurs. Res. 2002, 24, 697–712. [Google Scholar] [CrossRef]
- Hansen, K.V.; Frøiland, C.T.; Testad, I. Porcelain for All—A Nursing Home Study. Int. J. Health Care Qual. Assur. 2018, 31, 662–675. [Google Scholar] [CrossRef]
- Dunne, T.E.; Neargarder, S.A.; Cipolloni, P.B.; Cronin-Golomb, A. Visual Contrast Enhances Food and Liquid Intake in Advanced Alzheimer’s Disease. Clin. Nutr. 2004, 23, 533–538. [Google Scholar] [CrossRef]
- Edwards, J.S.A.; Hartwell, H.J. A Comparison of Energy Intake between Eating Positions in a NHS Hospital—A Pilot Study. Appetite 2004, 43, 323–325. [Google Scholar] [CrossRef] [PubMed]
- Nijs, K.A.N.D.; De Graaf, C.; Siebelink, E.; Blauw, Y.H.; Vanneste, V.; Kok, F.J.; Van Staveren, W.A. Effect of Family-Style Meals on Energy Intake and Risk of Malnutrition in Dutch Nursing Home Residents: A Randomized Controlled Trial. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 935–942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolf, A.; Ekman, I.; Dellenborg, L. Everyday Practices at the Medical Ward: A 16-Month Ethnographic Field Study. BMC Health Serv. Res. 2012, 12, 184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fallen-Bailey, R.; Robinson, L. Safe or Sedentary? A Mixed-Methods Survey Exploring Healthcare Professionals’ Views of Promoting Patient Mobility in Hospital. Physiotherapy 2021, 113, 152–153. [Google Scholar] [CrossRef]







| Unit | Median | {IQR} | |
|---|---|---|---|
| Unit size | beds | 30 | {23–40} |
| Actual beds | beds | 23 | {18–31} |
| Patients recruited | patients | 14 | {9–20} |
| Physicians | number | 3 | {2–7} |
| Nurses | number | 5 | {3–8} |
| Dieticians | number | 1 | {0, 1} |
| Physiotherapists | number | 1 | {0–3} |
| Unit | n | Median {IQR} Percent | |
|---|---|---|---|
| Age | year | 48,579 | 66 {51–78} |
| Gender | % female | 24,087/48,700 | 49.5% |
| BMI < 18.5 | n | 3676/46,082 | 8.0% |
| BMI > 30 | n | 8380/46,082 | 18.2% |
| Diagnosis (ICD10) + | n | 82,816 | 100% |
| Digestive | 11,757 | 14.2% | |
| Circulatory | 9883 | 11.9% | |
| Neoplasm | 9028 | 10.9% | |
| Musculoskeletal | 7822 | 9.4% | |
| Respiratory | 7369 | 8.9% | |
| Comorbidities # | n | 78,706 | 100% |
| Diabetes | 10,550 | 13.4% | |
| Cancer | 10,384 | 13.2% | |
| Cardiac insufficiency | 8891 | 11.3% | |
| Infection | 6517 | 8.2% | |
| Chronic lung disease | 5817 | 7.4% | |
| Duration since admission | days | 46,526 | 7 {3–15} |
| Duration after nutritionDay & | days | 35,326 | 6 {2–11} |
| Outcome § | n | 41,885 | 100% |
| Discharged home | 30,362 | 72.5% | |
| Discharged to another HCF | 4137 | 9.9% | |
| Still in hospital on day 30 | 5071 | 11.1% | |
| Death in hospital within 30 days | 1342 | 3.2% |
| n | Percent | |
|---|---|---|
| Mobility before hospitalization | ||
| Mobile | 29,939 | 61.5 |
| With someone‘s help | 5168 | 10.6 |
| With a cane/walker | 6463 | 13.3 |
| With a wheelchair | 1930 | 4.0 |
| Bedridden | 3168 | 6.5 |
| Missing | 2032 | 4.2 |
| Mobility at nutritionDay | ||
| Mobile | 27,683 | 56.8 |
| With assistance | 11,713 | 24.1 |
| Bedridden | 5623 | 11.5 |
| Missing | 3681 | 7.6 |
| In general, how would you say your health is? | ||
| Very good | 3652 | 7.5 |
| Good | 17,199 | 35.3 |
| Fair | 17,783 | 36.5 |
| Poor | 6608 | 13.6 |
| Very poor | 1400 | 2.9 |
| Missing | 2058 | 4.2 |
| Feeling today compared with admission | ||
| Stronger | 20,238 | 41.6 |
| Same | 13,337 | 27.4 |
| Weaker | 8913 | 18.3 |
| Admitted today | 1223 | 2.5 |
| I do not know | 2228 | 4.6 |
| Missing | 2761 | 5.7 |
| n | Percent | |
|---|---|---|
| How did you eat the week before hospital admission | ||
| More than normal | 2221 | 4.6 |
| Normal | 28,642 | 58.8 |
| ¾ | 4991 | 10.2 |
| ½ | 5974 | 12.3 |
| ¼ or less | 4383 | 9.0 |
| I do not know | 388 | 0.8 |
| Missing | 2101 | 4.3 |
| Eating on nutritionDay | ||
| All | 21,911 | 45.0 |
| Half | 12,077 | 24.8 |
| Quarter | 6082 | 12.5 |
| Nothing (allowed to eat) | 2517 | 5.2 |
| Nothing (not allowed to eat) | 3024 | 6.2 |
| Missing | 3089 | 6.3 |
| Change in food intake since admission | ||
| Increased | 6856 | 14.1 |
| Unchanged | 19,381 | 39.8 |
| Decreased | 15,260 | 31.3 |
| I do not know | 3076 | 6.3 |
| Missing | 4127 | 8.5 |
| Eating apart meals | ||
| Yes | 12,391 | 25.4 |
| No | 30,354 | 62.3 |
| I do not know | 504 | 1.0 |
| Missing | 5451 | 11.2 |
| n | Median (days) | IQR (days) | |
|---|---|---|---|
| Mobility before hospitalization and duration since admission | |||
| Mobile (ref) | 28,738 | 5 | {3–12} |
| Mobile with help | 4899 | 9 * | {4–18} |
| Mobile with cane/walker | 6238 | 9 * | {4–18} |
| Use wheelchair | 1800 | 11 * | {5–24} |
| I am bedridden | 2987 | 11 * | {5–24} |
| Missing | 1496 | 8 | {3–17} |
| Mobility before hospitalization and length of stay after nutritionDay | |||
| Mobile (ref) | 22,347 | 5 | {2–9} |
| Mobile with help | 3619 | 7 *** | {3–13} |
| Mobile with cane/walker | 4802 | 7 *** | {3–13} |
| Use wheelchair | 1239 | 8 *** | {3–16} |
| I am bedridden | 2047 | 8 *** | {4–15} |
| Missing | 1064 | 6 *** | {2–13} |
| Actual mobility at nutritionDay and length of stay after nutritionDay | |||
| Mobile (ref) | 20,789 | 5 | {2–9} |
| Mobile with assistance | 8401 | 7 *** | {3–13} |
| I stay in bed | 3772 | 8 *** | {4–15} |
| Missing | 2276 | 6 *** | {2–13} |
| Eating on nutritionDay | |||
| All (ref) | 16,270 | 5 | {2–10} |
| Half | 8638 | 6 *** | {2–12} |
| Quarter | 4332 | 6 *** | {2–13} |
| Nothing (allowed to eat) | 1817 | 6 *** | {3–12} |
| Nothing (not allowed to eat) | 2223 | 6 *** | {3–11} |
| Missing | 1958 | 6 *** | {2–13} |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kevdzija, M.; Laviano, A.; Worf, I.; Schuh, C.; Tarantino, S.; Hiesmayr, M. Indirect Nutrition and Mobility Risks during Hospitalization: An Architectural Perspective on the nutritionDay Study Findings. Nutrients 2023, 15, 1527. https://doi.org/10.3390/nu15061527
Kevdzija M, Laviano A, Worf I, Schuh C, Tarantino S, Hiesmayr M. Indirect Nutrition and Mobility Risks during Hospitalization: An Architectural Perspective on the nutritionDay Study Findings. Nutrients. 2023; 15(6):1527. https://doi.org/10.3390/nu15061527
Chicago/Turabian StyleKevdzija, Maja, Alessandro Laviano, Isabella Worf, Christian Schuh, Silvia Tarantino, and Michael Hiesmayr. 2023. "Indirect Nutrition and Mobility Risks during Hospitalization: An Architectural Perspective on the nutritionDay Study Findings" Nutrients 15, no. 6: 1527. https://doi.org/10.3390/nu15061527