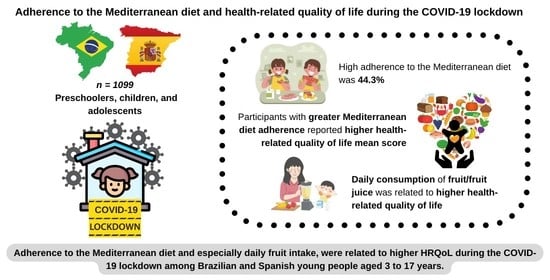
Adherence to the Mediterranean Diet and Health-Related Quality of Life during the COVID-19 Lockdown: A Cross-Sectional Study including Preschoolers, Children, and Adolescents from Brazil and Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Procedures
2.2.1. Health-Related Quality of Life (Dependent Variable)
2.2.2. Adherence to the Mediterranean Diet (Independent Variable)
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report—51; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Adil, M.T.; Rahman, R.; Whitelaw, D.; Jain, V.; Al-Taan, O.; Rashid, F.; Munasinghe, A.; Jambulingam, P. SARS-CoV-2 and the Pandemic of COVID-19. Postgrad. Med. J. 2021, 97, 110–116. [Google Scholar] [CrossRef]
- Neville, R.D.; Lakes, K.D.; Hopkins, W.G.; Tarantino, G.; Draper, C.E.; Beck, R.; Madigan, S. Global Changes in Child and Adolescent Physical Activity During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2022, 176, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Della Valle, P.G.; Mosconi, G.; Nucci, D.; Vigezzi, G.P.; Gentile, L.; Gianfredi, V.; Bonaccio, M.; Gianfagna, F.; Signorelli, C.; Iacoviello, L.; et al. Adherence to the Mediterranean Diet during the COVID-19 National Lockdowns: A Systematic Review of Observational Studies. Acta Biomed. 2021, 92, e2021440. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.; Puppo, F.; Del Bo’, C.; Vinelli, V.; Riso, P.; Porrini, M.; Martini, D. A Systematic Review of Worldwide Consumption of Ultra-Processed Foods: Findings and Criticisms. Nutrients 2021, 13, 2778. [Google Scholar] [CrossRef] [PubMed]
- Pourghazi, F.; Eslami, M.; Ehsani, A.; Ejtahed, H.-S.; Qorbani, M. Eating Habits of Children and Adolescents during the COVID-19 Era: A Systematic Review. Front. Nutr. 2022, 9, 1004953. [Google Scholar] [CrossRef] [PubMed]
- Fore, H.H.; Dongyu, Q.; Beasley, D.M.; Ghebreyesus, T.A. Child Malnutrition and COVID-19: The Time to Act Is Now. Lancet 2020, 396, 517–518. [Google Scholar] [CrossRef]
- Scapaticci, S.; Neri, C.R.; Marseglia, G.L.; Staiano, A.; Chiarelli, F.; Verduci, E. The Impact of the COVID-19 Pandemic on Lifestyle Behaviors in Children and Adolescents: An International Overview. Ital. J. Pediatr. 2022, 48, 22. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Strauss, J.; Neumark-Sztainer, D.; Story, M.; Boutelle, K. Correlates of Psychosocial Well-Being among Overweight Adolescents: The Role of the Family. J. Consult. Clin. Psychol. 2007, 75, 181–186. [Google Scholar] [CrossRef]
- Magriplis, E.; Zampelas, A. Chapter 3—Mediterranean Diet in Children and Adolescents. In The Mediterranean Diet, 2nd ed.; Preedy, V.R., Watson, R.R., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 25–39. ISBN 978-0-12-818649-7. [Google Scholar]
- World Health Organization. Healthy Diet; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Pyramid Today. Science and Cultural Updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [Green Version]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean Diet and Multiple Health Outcomes: An Umbrella Review of Meta-Analyses of Observational Studies and Randomised Trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Köppen, V. Das Geographische System Der Klimate; Gebrüder Borntraeger: Berlin, Germany, 1936. [Google Scholar]
- Carrillo, H.A.; Ramírez-Vélez, R. Adherence to the Mediterranean Diet in a Sample of Colombian Schoolchildren: An Evaluation of the Psychometric Properties of the Kidmed Questionnaire [Adherencia a La Dieta Mediterránea En Una Población Escolar Colombiana: Evaluación de Las Propiedades Psicométricas Del Cuestionario Kidmed]. Nutr. Hosp. 2020, 37, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.I.S.D.S.; Forte, G.C.; Marostica, P.J.C. Translation and Cultural Adaptation of the Mediterranean Diet Quality Index in Children and Adolescents [Tradução E Adaptação Cultural Do Mediterranean Diet Quality Index In Children And Adolescents]. Rev. Paul. Pediatr. 2020, 38, e2018242. [Google Scholar] [CrossRef] [PubMed]
- Bawaked, R.A.; Schröder, H.; Ribas-Barba, L.; Izquierdo-Pulido, M.; Pérez-Rodrigo, C.; Fíto, M.; Serra-Majem, L. Association of Diet Quality with Dietary Inflammatory Potential in Youth. Food Nutr. Res. 2017, 61, 1328961. [Google Scholar] [CrossRef] [Green Version]
- Mistretta, A.; Marventano, S.; Antoci, M.; Cagnetti, A.; Giogianni, G.; Nolfo, F.; Rametta, S.; Pecora, G.; Marranzano, M. Mediterranean Diet Adherence and Body Composition among Southern Italian Adolescents. Obes. Res. Clin. Pract. 2017, 11, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Pereira-da-Silva, L.; Rêgo, C.; Pietrobelli, A. The Diet of Preschool Children in the Mediterranean Countries of the European Union: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 572. [Google Scholar] [CrossRef] [Green Version]
- Cabrera, S.G.; Fernández, N.H.; Hernández, C.R.; Nissensohn, M.; Román-Viña, B.; Serra-Majem, L. KIDMED Test; Prevalence of Low Adherence to the Mediterranean Diet in Children and Young: A Systematic Review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [CrossRef]
- Gil, J.F.L.; Camargo, E.; Lucas, J.L.Y. Adherencia a la dieta mediterránea en escolares de Educación Primaria partícipes en actividad física: Una revisión sistemática. Cult. Cienc. Y Deporte 2020, 15, 267–275. [Google Scholar]
- Grosso, G.; Galvano, F. Mediterranean Diet Adherence in Children and Adolescents in Southern European Countries. NFS J. 2016, 3, 13–19. [Google Scholar] [CrossRef] [Green Version]
- Haverman, L.; Limperg, P.F.; Young, N.L.; Grootenhuis, M.A.; Klaassen, R.J. Paediatric Health-Related Quality of Life: What Is It and Why Should We Measure It? Arch. Dis. Child. 2017, 102, 393–400. [Google Scholar] [CrossRef]
- World Health Organisation. WHOQOL—Measuring Quality of Life|The World Health Organization. Available online: https://www.who.int/tools/whoqol (accessed on 9 January 2023).
- Lehmann, S.; Haug, E.; Bjørknes, R.; Sandal, G.M.; Fadnes, L.T.; Skogen, J.C. Quality of Life among Young People in Norway during the COVID-19 Pandemic. A Longitudinal Study. Eur. Child Adolesc. Psychiatry 2022, 1–11. [Google Scholar] [CrossRef]
- Nobari, H.; Fashi, M.; Eskandari, A.; Villafaina, S.; Murillo-Garcia, Á.; Pérez-Gómez, J. Effect of COVID-19 on Health-Related Quality of Life in Adolescents and Children: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4563. [Google Scholar] [CrossRef] [PubMed]
- Romero-Robles, M.A.; Ccami-Bernal, F.; Ortiz-Benique, Z.N.; Pinto-Ruiz, D.F.; Benites-Zapata, V.A.; Patiño, D.C. Adherence to Mediterranean Diet Associated with Health-Related Quality of Life in Children and Adolescents: A Systematic Review. BMC Nutr. 2022, 8, 57. [Google Scholar] [CrossRef]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. The Clustering of Diet, Physical Activity and Sedentary Behavior in Children and Adolescents: A Review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 4. [Google Scholar] [CrossRef] [Green Version]
- Ul-Haq, Z.; Mackay, D.F.; Fenwick, E.; Pell, J.P. Meta-Analysis of the Association between Body Mass Index and Health-Related Quality of Life among Children and Adolescents, Assessed Using the Pediatric Quality of Life Inventory Index. J. Pediatr. 2013, 162, 280–286.e1. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 Pandemic on Quality of Life and Mental Health in Children and Adolescents in Germany. Eur. Child Adolesc. Psychiatry 2022, 31, 879–889. [Google Scholar] [CrossRef]
- Titis, E. Parental Perspectives of the Impact of COVID-19 Lockdown on Food-Related Behaviors: Systematic Review. Foods 2022, 11, 2851. [Google Scholar] [CrossRef]
- Ahn, S.N. The Potential Impact of COVID-19 on Health-Related Quality of Life in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14740. [Google Scholar] [CrossRef]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between Physical Fitness and Adherence to the Mediterranean Diet with Health-Related Quality of Life in Adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Health 2018, 28, 631–635. [Google Scholar] [CrossRef]
- Muros, J.J.; Pérez, F.S.; Ortega, F.Z.; Sánchez, V.M.G.; Knox, E. The Association between Healthy Lifestyle Behaviors and Health-Related Quality of Life among Adolescents. J. Pediatr. (Rio. J.) 2017, 93, 406–412. [Google Scholar] [CrossRef]
- Costarelli, V.; Koretsi, E.; Georgitsogianni, E. Health-Related Quality of Life of Greek Adolescents: The Role of the Mediterranean Diet. Qual. Life Res. 2013, 22, 951–956. [Google Scholar] [CrossRef]
- Ferrer-Cascales, R.; Albaladejo-Blázquez, N.; Ruiz-Robledillo, N.; Clement-Carbonell, V.; Sánchez-SanSegundo, M.; Zaragoza-Martí, A. Higher Adherence to the Mediterranean Diet Is Related to More Subjective Happiness in Adolescents: The Role of Health-Related Quality of Life. Nutrients 2019, 11, 698. [Google Scholar] [CrossRef]
- Papadaki, S.; Carayanni, V.; Notara, V.; Chaniotis, D. Anthropometric, Lifestyle Characteristics, Adherence to the Mediterranean Diet, and COVID-19 Have a High Impact on the Greek Adolescents’ Health-Related Quality of Life. Foods 2022, 11, 2726. [Google Scholar] [CrossRef] [PubMed]
- Wille, N.; Badia, X.; Bonsel, G.; Burström, K.; Cavrini, G.; Devlin, N.; Egmar, A.-C.; Greiner, W.; Gusi, N.; Herdman, M.; et al. Development of the EQ-5D-Y: A Child-Friendly Version of the EQ-5D. Qual. Life Res. 2010, 19, 875–886. [Google Scholar] [CrossRef] [Green Version]
- Gusi, N.; Perez-Sousa, M.A.; Gozalo-Delgado, M.; Olivares, P.R. Validez y fiabilidad de la versión proxy del EQ-5D-Y en español. An. Pediatría 2014, 81, 212–219. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Available online: https://www.who.int/publications-detail-redirect/924154693X (accessed on 2 January 2023).
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Pastor, R.; Bouzas, C.; Albertos, I.; García, C.; García, Á.; Prieto, T.; Velázquez, J.; Sánchez-Jiménez, E.; Rodríguez, R.; Martín, F.J.; et al. Health-Related Quality of Life in Spanish Schoolchildren and Its Association with the Fitness Status and Adherence to the Mediterranean Diet. Nutrients 2022, 14, 2322. [Google Scholar] [CrossRef]
- Arain, M.; Haque, M.; Johal, L.; Mathur, P.; Nel, W.; Rais, A.; Sandhu, R.; Sharma, S. Maturation of the Adolescent Brain. Neuropsychiatr. Dis. Treat. 2013, 9, 449–461. [Google Scholar] [CrossRef] [Green Version]
- Nabbosa, S.; Lee, S. Associations between Food Groups and Health-Related Quality of Life in Korean Adults. Nutrients 2022, 14, 3643. [Google Scholar] [CrossRef] [PubMed]
- Azupogo, F.; Seidu, J.A.; Issaka, Y.B. Higher Vegetable Intake and Vegetable Variety Is Associated with a Better Self-Reported Health-Related Quality of Life (HR-QoL) in a Cross-Sectional Survey of Rural Northern Ghanaian Women in Fertile Age. BMC Public Health 2018, 18, 920. [Google Scholar] [CrossRef] [PubMed]
- Muscaritoli, M. The Impact of Nutrients on Mental Health and Well-Being: Insights From the Literature. Front. Nutr. 2021, 8, 656290. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, T.; Ribeiro, J.P.; de Matos, M.G.; Leal, I.; Ferreira, A. Health-Related Quality of Life in Children and Adolescents: Subjective Well Being. Span. J. Psychol. 2012, 15, 177–186. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; García-Hermoso, A. Adherence to the Mediterranean Diet and Subjective Well-Being among Chilean Children. Appetite 2022, 172, 105974. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; Gaya, A.R.; Reuter, C.P.; Caetano, C.I.; Sentone, R.G.; Caetano, H.B.S.; Brazo-Sayavera, J. Sleep-Related Problems and Eating Habits during COVID-19 Lockdown in a Southern Brazilian Youth Sample. Sleep Med. 2021, 85, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Combs, D.; Goodwin, J.L.; Quan, S.F.; Morgan, W.J.; Shetty, S.; Parthasarathy, S. Insomnia, Health-Related Quality of Life and Health Outcomes in Children: A Seven Year Longitudinal Cohort. Sci. Rep. 2016, 6, 27921. [Google Scholar] [CrossRef] [Green Version]
- López-Gil, J.F.; Brazo-Sayavera, J.; de Campos, W.; Yuste Lucas, J.L. Meeting the Physical Activity Recommendations and Its Relationship with Obesity-Related Parameters, Physical Fitness, Screen Time, and Mediterranean Diet in Schoolchildren. Children 2020, 7, 263. [Google Scholar] [CrossRef]
- García-de-Miguel, M.; Huertas-Hoyas, E.; Pérez-Corrales, J.; Rodríguez-Rivas, C.; García-Bravo, C.; García-Bravo, S.; Camacho-Montaño, L.R. Food Intake Changes and Their Impact on Quality of Life in Spanish Citizens with and without COVID-19 during Lockdown. Healthcare 2022, 10, 1414. [Google Scholar] [CrossRef]
- Zahedi, H.; Djalalinia, S.; Sadeghi, O.; Garizi, F.Z.; Asayesh, H.; Payab, M.; Zarei, M.; Qorbani, M. Breakfast Consumption and Mental Health: A Systematic Review and Meta-Analysis of Observational Studies. Nutr. Neurosci. 2022, 25, 1250–1264. [Google Scholar] [CrossRef]
- Ahadi, Z.; Kelishadi, R.; Qorbani, M.; Zahedi, H.; Aram, M.; Motlagh, M.E.; Ardalan, G.; Shafiee, G.; Arzaghi, S.M.; Asayesh, H.; et al. Association of Breakfast Intake with Psychiatric Distress and Violent Behaviors in Iranian Children and Adolescents: The CASPIAN- IV Study. Indian J. Pediatr. 2016, 83, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Mullan, B.A.; Singh, M. A Systematic Review of the Quality, Content, and Context of Breakfast Consumption. Nutr. Food Sci. 2010, 40, 81–114. [Google Scholar] [CrossRef]
- Wu, X.Y.; Zhuang, L.H.; Li, W.; Guo, H.W.; Zhang, J.H.; Zhao, Y.K.; Hu, J.W.; Gao, Q.Q.; Luo, S.; Ohinmaa, A.; et al. The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: A systematic review and meta-analysis. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2019, 28, 1989–2015. [Google Scholar] [CrossRef] [PubMed]
- Cenni, S.; Sesenna, V.; Boiardi, G.; Casertano, M.; Di Nardo, G.; Esposito, S.; Strisciuglio, C. The Mediterranean Diet in Paediatric Gastrointestinal Disorders. Nutrients 2023, 15, 79. [Google Scholar] [CrossRef]
- El Amrousy, D.; Elashry, H.; Salamah, A.; Maher, S.; Abd-Elsalam, S.M.; Hasan, S. Adherence to the Mediterranean Diet Improved Clinical Scores and Inflammatory Markers in Children with Active Inflammatory Bowel Disease: A Randomized Trial. J. Inflamm. Res. 2022, 15, 2075–2086. [Google Scholar] [CrossRef]
- Hosseini, B.; Berthon, B.S.; Saedisomeolia, A.; Starkey, M.R.; Collison, A.; Wark, P.A.B.; Wood, L.G. Effects of Fruit and Vegetable Consumption on Inflammatory Biomarkers and Immune Cell Populations: A Systematic Literature Review and Meta-Analysis. Am. J. Clin. Nutr. 2018, 108, 136–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Rodriguez, E.; Biel-Glesson, S.; Fernandez-Navarro, J.R.; Calleja, M.A.; Espejo-Calvo, J.A.; Gil-Extremera, B.; de la Torre, R.; Fito, M.; Covas, M.-I.; Vilchez, P.; et al. Effects of Virgin Olive Oils Differing in Their Bioactive Compound Contents on Biomarkers of Oxidative Stress and Inflammation in Healthy Adults: A Randomized Double-Blind Controlled Trial. Nutrients 2019, 11, 561. [Google Scholar] [CrossRef] [Green Version]
- Dai, J.; Jones, D.P.; Goldberg, J.; Ziegler, T.R.; Bostick, R.M.; Wilson, P.W.; Manatunga, A.K.; Shallenberger, L.; Jones, L.; Vaccarino, V. Association between Adherence to the Mediterranean Diet and Oxidative Stress. Am. J. Clin. Nutr. 2008, 88, 1364–1370. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, A.S.; Strath, L.J.; Sorge, R.E. Dietary Interventions for Treatment of Chronic Pain: Oxidative Stress and Inflammation. Pain 2020, 9, 487–498. [Google Scholar] [CrossRef]
- Ruiz-Roso, M.B.; de Carvalho Padilha, P.; Mantilla-Escalante, D.C.; Ulloa, N.; Brun, P.; Acevedo-Correa, D.; Ferreira Peres, W.A.; Martorell, M.; Aires, M.T.; de Oliveira Cardoso, L.; et al. COVID-19 Confinement and Changes of Adolescent’s Dietary Trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients 2020, 12, 1807. [Google Scholar] [CrossRef]
- Madigan, S.; Eirich, R.; Pador, P.; McArthur, B.A.; Neville, R.D. Assessment of Changes in Child and Adolescent Screen Time During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2022, 176, 1188–1198. [Google Scholar] [CrossRef]
- Hartman-Munick, S.M.; Lin, J.A.; Milliren, C.E.; Braverman, P.K.; Brigham, K.S.; Fisher, M.M.; Golden, N.H.; Jary, J.M.; Lemly, D.C.; Matthews, A.; et al. Association of the COVID-19 Pandemic With Adolescent and Young Adult Eating Disorder Care Volume. JAMA Pediatr. 2022, 176, 1225–1232. [Google Scholar] [CrossRef] [PubMed]
- Regan, C.; Walltott, H.; Kjellenberg, K.; Nyberg, G.; Helgadóttir, B. Investigation of the Associations between Diet Quality and Health-Related Quality of Life in a Sample of Swedish Adolescents. Nutrients 2022, 14, 2489. [Google Scholar] [CrossRef]
- Marques, A.; Peralta, M.; Santos, T.; Martins, J.; de Matos, M.G. Self-Rated Health and Health-Related Quality of Life Are Related with Adolescents’ Healthy Lifestyle. Public Health 2019, 170, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Shariati-Bafghi, S.-E.; Rashidkhani, B.; Fadardi, J.S.; Safarian, M.; Edalatian, J.; Ranjbar, G.; Nematy, M. Dietary Patterns and Health-Related Quality of Life among Iranian Adolescents. Qual. Life Res. 2022, 31, 789–802. [Google Scholar] [CrossRef] [PubMed]
- Pano, O.; Martínez-Lapiscina, E.H.; Sayón-Orea, C.; Martinez-Gonzalez, M.A.; Martinez, J.A.; Sanchez-Villegas, A. Healthy Diet, Depression and Quality of Life: A Narrative Review of Biological Mechanisms and Primary Prevention Opportunities. World J. Psychiatry 2021, 11, 997–1016. [Google Scholar] [CrossRef]
- Holder, M.D. The Contribution of Food Consumption to Well-Being. ANM 2019, 74, 44–52. [Google Scholar] [CrossRef]
- Górska-Warsewicz, H.; Rejman, K.; Laskowski, W.; Czeczotko, M. Milk and Dairy Products and Their Nutritional Contribution to the Average Polish Diet. Nutrients 2019, 11, 1771. [Google Scholar] [CrossRef]

| Variables | M/n | SD/% |
|---|---|---|
| Age (years) | 11.5 | 4.5 |
| Preschoolers (3–5 years) | 146 | 13.3 |
| Children (6–12 years) | 444 | 40.4 |
| Adolescents (13–17 years) | 509 | 46.3 |
| Sex | ||
| Boys | 576 | 52.4 |
| Girls | 523 | 47.6 |
| Nationality | ||
| Brazilian | 495 | 45.0 |
| Spanish | 604 | 55.0 |
| Breadwinner’s educational level | ||
| University studies | 538 | 49.0 |
| Non-university studies | 561 | 51.0 |
| Socioeconomic status | ||
| FAS-III (score) | 7.5 | 2.3 |
| Anthropometric data | ||
| Weight (kg) | 43.0 | 19.5 |
| Height (cm) | 145.5 | 24.8 |
| BMI (z-score) | 0.9 | 2.0 |
| Overweight/Obesity a | 467 | 42.5 |
| Daily movement behaviors | ||
| Physical activity (days/week) | 4.0 | 2.3 |
| Recreational screen time (h/day) | 7.6 | 5.9 |
| Sleep duration (h/day) | 9.9 | 1.5 |
| Adherence to the MD | ||
| KIDMED (score) | 7.0 | 2.4 |
| Low/Moderate MD | 612 | 55.7 |
| High MD | 487 | 44.3 |
| HRQoL | ||
| VAS (score) | 84.5 | 15.9 |
| Mobility (%, any problem) | 28 | 2.5 |
| Looking after myself (%, any problem) | 112 | 10.2 |
| Doing usual activities (%, any problem) | 113 | 10.3 |
| Having pain or discomfort (%, any problem) | 181 | 16.5 |
| Feeling worried, sad, or unhappy (%, any problem) | 437 | 39.8 |
| HRQoL Domain a | Low/Moderate MD | High MD | p |
|---|---|---|---|
| Mobility | 18 (2.9) | 10 (2.1) | 0.442 |
| Looking after myself | 62 (10.1) | 50 (10.3) | 0.941 |
| Doing usual activities | 71 (11.6) | 42 (8.6) | 0.106 |
| Having pain or discomfort | 115 (18.8) | 66 (13.6) | 0.020 |
| Feeling worried, sad, or unhappy | 246 (40.2) | 191 (39.2) | 0.743 |
| Items | B | SE | LLCI | ULCI | p |
|---|---|---|---|---|---|
| Takes a fruit or fruit juice every day | 3.59 | 1.28 | 1.09 | 6.09 | 0.005 |
| Has a second fruit every day | 0.29 | 1.13 | −1.94 | 2.51 | 0.800 |
| Has fresh or cooked vegetables regularly once a day | −0.05 | 1.20 | −2.41 | 2.31 | 0.968 |
| Has fresh or cooked vegetables more than once a day | −0.04 | 1.15 | −2.29 | 2.21 | 0.973 |
| Consumes fish regularly (at least 2–3 times per week) | −1.84 | 1.14 | −4.07 | 0.39 | 0.106 |
| Goes more than once a week to a fast-food (hamburger) restaurant | 0.99 | 1.55 | −2.05 | 4.02 | 0.522 |
| Likes pulses and eats them more than once a week | 0.00 | 1.41 | −2.78 | 2.77 | 0.999 |
| Consumes pasta or rice almost every day (5 or more times per week) | −0.35 | 1.19 | −2.68 | 1.98 | 0.765 |
| Has cereals or grains (bread, etc.) for breakfast | −0.06 | 1.20 | −2.41 | 2.28 | 0.958 |
| Consumes nuts regularly (at least 2–3 times per week) | −0.13 | 1.06 | −2.22 | 1.96 | 0.905 |
| Uses olive oil at home | −0.76 | 1.75 | −4.20 | 2.68 | 0.665 |
| Skips breakfast | −2.28 | 2.15 | 1.94 | −6.49 | 0.289 |
| Has a dairy product for breakfast (yogurt, milk, etc.) | −0.36 | 1.54 | −3.37 | 2.66 | 0.816 |
| Has commercially baked goods or pastries for breakfast | −0.59 | 1.45 | −3.43 | 2.26 | 0.686 |
| Takes two yogurts and/or some cheese (40 g) daily | 0.10 | 1.00 | −1.86 | 2.06 | 0.921 |
| Takes sweets and candy several times every day | 0.48 | 1.23 | −1.94 | 2.90 | 0.698 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Victoria-Montesinos, D.; Tárraga-Marcos, A.; Brazo-Sayavera, J.; Jiménez-López, E.; Gutiérrez-Espinoza, H.; Panisello Royo, J.M.; Tárraga-López, P.J.; López-Gil, J.F. Adherence to the Mediterranean Diet and Health-Related Quality of Life during the COVID-19 Lockdown: A Cross-Sectional Study including Preschoolers, Children, and Adolescents from Brazil and Spain. Nutrients 2023, 15, 677. https://doi.org/10.3390/nu15030677
Victoria-Montesinos D, Tárraga-Marcos A, Brazo-Sayavera J, Jiménez-López E, Gutiérrez-Espinoza H, Panisello Royo JM, Tárraga-López PJ, López-Gil JF. Adherence to the Mediterranean Diet and Health-Related Quality of Life during the COVID-19 Lockdown: A Cross-Sectional Study including Preschoolers, Children, and Adolescents from Brazil and Spain. Nutrients. 2023; 15(3):677. https://doi.org/10.3390/nu15030677
Chicago/Turabian StyleVictoria-Montesinos, Desirée, Almudena Tárraga-Marcos, Javier Brazo-Sayavera, Estela Jiménez-López, Héctor Gutiérrez-Espinoza, Josefa María Panisello Royo, Pedro J. Tárraga-López, and José Francisco López-Gil. 2023. "Adherence to the Mediterranean Diet and Health-Related Quality of Life during the COVID-19 Lockdown: A Cross-Sectional Study including Preschoolers, Children, and Adolescents from Brazil and Spain" Nutrients 15, no. 3: 677. https://doi.org/10.3390/nu15030677