What do Portuguese Women Prefer Regarding Vaginal Products? Results from a Cross-Sectional Web-Based Survey
Abstract
:1. Introduction
2. Experimental Section
2.1. Type of Study and Questionnaire Development
2.2. Study Population, Recruitment and Sample
2.3. Statistical Analysis
3. Results and Discussion
| Queries | Age Groups (% within Group) | |||||
|---|---|---|---|---|---|---|
| 18–24 | 25–34 | 35–44 | 45–54 | 55–65 | Total Sample | |
| In which of the following situations would you apply a product in the vagina? | ||||||
| Contraception | 34.7 | 34.6 | 30.0 | 22.9 | 25.3 | 30.1 |
| Treatment/prevention of diseases following medical prescription | 84.6 | 86.3 | 87.4 | 82.5 | 82.7 | 82.8 |
| Treatment/prevention of diseases even without medical prescription | 25.8 | 27.0 | 19.0 | 18.7 | 15.3 | 21.9 |
| Menstrual hygienic purposes (tampon, cup) | 87.0 | 82.1 | 74.5 | 65.4 | 58.7 | 74.5 |
| Sexual lubrication | 49.9 | 52.4 | 47.1 | 42.8 | 53.3 | 47.6 |
| Sexual stimulation | 24.1 | 22.4 | 20.4 | 18.1 | 18.0 | 20.6 |
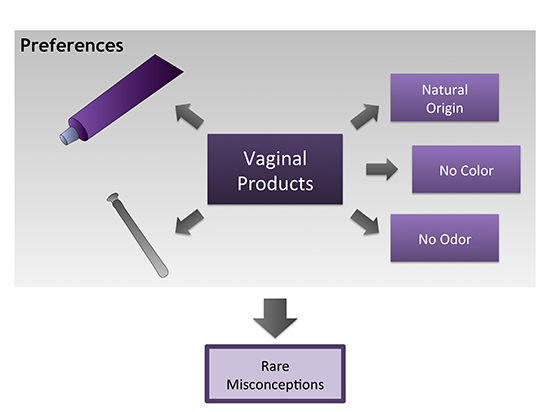
| Which characteristics of a vaginal product do you consider relevant? | ||||||
| Color | 15.7 | 15.5 | 11.9 | 12.6 | 15.5 | 14.1 |
| Odor * | 64.4 | 62.0 | 58.5 | 51.5 | 44.7 | 58.9 |
| Flavor * | 9.8 | 5.8 | 6.4 | 3.5 | 1.2 | 6.1 |
| Origin of ingredients (natural/synthetic) | 45.2 | 38.4 | 41.2 | 40.9 | 39.8 | 40.8 |
| What dosage form would you prefer for an intravaginal medication? (more than one answer could be selected) | ||||||
| Vaginal tablet/capsule * | 48.0 | 42.3 | 37.6 | 46.8 | 43.5 | 42.5 |
| Vaginal suppository * | 33.2 | 48.7 | 50.7 | 55.0 | 53.4 | 47.7 |
| Gel/cream/ointment * | 74.8 | 65.0 | 62.1 | 59.4 | 60.2 | 64.6 |
| Irrigation solution * | 36.0 | 26.7 | 23.7 | 29.5 | 19.9 | 27.3 |
| Foam | 26.1 | 21.4 | 19.9 | 20.5 | 17.4 | 21.3 |
| Ring * | 11.8 | 14.8 | 10.4 | 9.1 | 3.7 | 11.5 |
| Film | 5.6 | 5.4 | 3.9 | 4.1 | 3.1 | 4.7 |


4. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- das Neves, J.; Palmeira-de-Oliveira, R.; Palmeira-de-Oliveira, A.; Rodrigues, F.; Sarmento, B. Vaginal mucosa and drug delivery. In Mucoadhesive Materials and Drug Delivery Systems; Khutoryanskiy, V., Ed.; Wiley: Chichester, UK, 2014; pp. 99–131. [Google Scholar]
- Alexander, N.J.; Baker, E.; Kaptein, M.; Karck, U.; Miller, L.; Zampaglione, E. Why consider vaginal drug administration? Fertil. Steril. 2004, 82, 1–12. [Google Scholar] [CrossRef]
- Acarturk, F. Mucoadhesive vaginal drug delivery systems. Recent Pat. Drug Deliv. Formul. 2009, 3, 193–205. [Google Scholar] [CrossRef]
- Rohan, L.C.; Sassi, A.B. Vaginal drug delivery systems for HIV prevention. AAPS J. 2009, 11, 78–87. [Google Scholar] [CrossRef]
- Elias, C.; Coggins, C. Acceptability research on female-controlled barrier methods to prevent heterosexual transmission of HIV: Where have we been? Where are we going? J. Womens Health Gend. Based Med. 2001, 10, 163–173. [Google Scholar] [CrossRef]
- Mardh, P.A.; Rodrigues, A.G.; Genc, M.; Novikova, N.; Martinez-de-Oliveira, J.; Guaschino, S. Facts and myths on recurrent vulvovaginal candidosis—A review on epidemiology, clinical manifestations, diagnosis, pathogenesis and therapy. Int. J. STD AIDS 2002, 13, 522–539. [Google Scholar] [CrossRef]
- Koumans, E.H.; Sternberg, M.; Bruce, C.; McQuillan, G.; Kendrick, J.; Sutton, M.; Markowitz, L.E. The prevalence of bacterial vaginosis in the United States, 2001–2004; associations with symptoms, sexual behaviors, and reproductive health. Sex. Transm. Dis. 2007, 34, 864–869. [Google Scholar] [CrossRef]
- Morrow, K.; Rosen, R.; Richter, L.; Emans, A.; Forbes, A.; Day, J.; Morar, N.; Maslankowski, L.; Profy, A.T.; Kelly, C.; et al. The acceptability of an investigational vaginal microbicide, PRO 2000 Gel, among women in a phase I clinical trial. J. Womens Health 2003, 12, 655–666. [Google Scholar] [CrossRef]
- Novak, A.; de la Loge, C.; Abetz, L.; van der Meulen, E.A. The combined contraceptive vaginal ring, NuvaRing: An international study of user acceptability. Contraception 2003, 67, 187–194. [Google Scholar] [CrossRef]
- Marrazzo, J.M.; Cook, R.L.; Wiesenfeld, H.C.; Murray, P.J.; Busse, B.; Krohn, M.; Hillier, S.L. Women’s satisfaction with an intravaginal Lactobacillus capsule for the treatment of bacterial vaginosis. J. Womens Health 2006, 15, 1053–1060. [Google Scholar] [CrossRef]
- Hammett, T.M.; Mason, T.H.; Joanis, C.L.; Foster, S.E.; Harmon, P.; Robles, R.R.; Finlinson, H.A.; Feudo, R.; Vining-Bethea, S.; Jeter, G.; et al. Acceptability of formulations and application methods for vaginal microbicides among drug-involved women: Results of product trials in three cities. Sex. Transm. Dis. 2000, 27, 119–126. [Google Scholar] [CrossRef]
- Coggins, C.; Elias, C.J.; Atisook, R.; Bassett, M.T.; Ettiegnene-Traore, V.; Ghys, P.D.; Jenkins-Woelk, L.; Thongkrajai, E.; VanDevanter, N.L. Women’s preferences regarding the formulation of over-the-counter vaginal spermicides. AIDS 1998, 12, 1389–1391. [Google Scholar] [CrossRef]
- Hardy, E.; de Padua, K.S.; Osis, M.J.; Jimenez, A.L.; Zaneveld, L.J. Women’s preferences for vaginal antimicrobial contraceptives. IV. Attributes of a formulation that would protect from STD/AIDS. Contraception 1998, 58, 251–255. [Google Scholar] [CrossRef]
- Rice, V.M.; Maimbolwa, M.C.; Nkandu, E.M.; Hampton, J.F.; Lee, J.E.; Hildreth, J.E. Cultural differences in acceptability of a vaginal microbicide: A comparison between potential users from Nashville, Tennessee, USA, and Kafue and Mumbwa, Zambia. HIV AIDS 2012, 4, 73–80. [Google Scholar]
- Van den Berg, J.J.; Rosen, R.K.; Bregman, D.E.; Thompson, L.A.; Jensen, K.M.; Kiser, P.F.; Katz, D.F.; Buckheit, K.; Buckheit, R.W.; Morrow, K.M. “Set it and Forget it”: Women’s perceptions and opinions of long-acting topical vaginal gels. AIDS Behav. 2014, 18, 862–870. [Google Scholar] [CrossRef]
- das Neves, J.; Amaral, M.H.; Bahia, M.F. Vaginal drug delivery. In Pharmaceutical Manufacturing Handbook: Production and Processes; Gad, S.C., Ed.; Wiley: Hoboken, NJ, USA, 2008; pp. 809–878. [Google Scholar]
- Machado, R.M.; Palmeira-de-Oliveira, A.; Martinez-De-Oliveira, J.; Palmeira-de-Oliveira, R. Vaginal films for drug delivery. J. Pharm. Sci. 2013, 102, 2069–2081. [Google Scholar] [CrossRef]
- Hardy, E.; de Padua, K.S.; Jimenez, A.L.; Zaneveld, L.J. Women’s preferences for vaginal antimicrobial contraceptives. II. Preferred characteristics according to women’s age and socioeconomic status. Contraception 1998, 58, 239–244. [Google Scholar] [CrossRef]
- Palmeira-de-Oliveira, R.; Duarte, P.; Palmeira-de-Oliveira, A.; das Neves, J.; Amaral, M.H.; Breitenfeld, L.; Martinez-de-Oliveira, J. Women’s experiences, preferences and perceptions regarding vaginal products: Results from a cross-sectional web-based survey in Portugal. Eur. J. Contracept. Reprod. Health Care 2014, in press. [Google Scholar]
- Hardy, E.; Jimenez, A.L.; de Padua, K.S.; Zaneveld, L.J. Women’s preferences for vaginal antimicrobial contraceptives. III. Choice of a formulation, applicator, and packaging. Contraception 1998, 58, 245–249. [Google Scholar] [CrossRef]
- Nappi, R.E.; Liekens, G.; Brandenburg, U. Attitudes, perceptions and knowledge about the vagina: The international vagina dialogue survey. Contraception 2006, 73, 493–500. [Google Scholar] [CrossRef]
- PORDATA. Available online: www.pordata.pt (accessed on 9 March 2013).
- Instituto Nacional de Estatística. Available online: www.ine.pt (accessed on 9 March 2013).
- Farage, M.A.; Lennon, L.; Ajayi, F. Products used on female genital mucosa. Curr. Probl. Dermatol. 2011, 40, 90–100. [Google Scholar]
- Sobel, J.D. Factors involved in patient choice of oral or vaginal treatment for vulvovaginal candidiasis. Patient Prefer. Adherence 2013, 8, 31–34. [Google Scholar] [CrossRef]
- Mårdh, P.-A.; Wågström, J.; Landgren, M.; Holmén, J. Usage of antifungal drugs for therapy of genital Candida infections, purchased as over-the-counter products or by prescription: I. Analyses of a unique database. Infect. Dis. Obstet. Gynecol. 2004, 12, 91–97. [Google Scholar] [CrossRef]
- Sihvo, S.; Ahonen, R.; Mikander, H.; Hemminki, E. Self-medication with vaginal antifungal drugs: Physicians’ experiences and women’s utilization patterns. Fam. Pract. 2000, 17, 145–149. [Google Scholar] [CrossRef]
- Angotti, L.B.; Lambert, L.C.; Soper, D.E. Vaginitis: Making sense of over-the-counter treatment options. Infect. Dis. Obstet. Gynecol. 2007, 2007, 97424. [Google Scholar] [CrossRef]
- Karasz, A.; Anderson, M. The vaginitis monologues: Women’s experiences of vaginal complaints in a primary care setting. Soc. Sci. Med. 2003, 56, 1013–1021. [Google Scholar] [CrossRef]
- Nappi, R.E.; Kokot-Kierepa, M. Vaginal health: Insights, views & attitudes (VIVA)—Results from an international survey. Climacteric 2012, 15, 36–44. [Google Scholar] [CrossRef]
- Wysocki, S.; Kingsberg, S.; Krychman, M. Management of vaginal atrophy: Implications from the REVIVE survey. Clin. Med. Insights Reprod. Health 2014, 8, 23–30. [Google Scholar] [CrossRef]
- Leiblum, S.R.; Hayes, R.D.; Wanser, R.A.; Nelson, J.S. Vaginal dryness: A comparison of prevalence and interventions in 11 countries. J. Sex. Med. 2009, 6, 2425–2433. [Google Scholar] [CrossRef]
- Sutton, K.S.; Boyer, S.C.; Goldfinger, C.; Ezer, P.; Pukall, C.F. To lube or not to lube: Experiences and perceptions of lubricant use in women with and without dyspareunia. J. Sex. Med. 2012, 9, 240–250. [Google Scholar] [CrossRef]
- Herbenick, D.; Reece, M.; Schick, V.; Sanders, S.A.; Fortenberry, J.D. Women’s use and perceptions of commercial lubricants: Prevalence and characteristics in a nationally representative sample of American adults. J. Sex. Med. 2014, 11, 642–652. [Google Scholar] [CrossRef]
- Joglekar, A.; Rhodes, C.T.; Danish, M. Preferences of women for use of intravaginal medications. Drug Dev. Ind. Pharm. 1991, 17, 2103–2113. [Google Scholar] [CrossRef]
- Suckling, J.; Kennedy, R.; Lethaby, A.; Roberts, H. Using creams, pessaries or a vaginal ring to apply oestrogen vaginally relieves the symptoms of vaginal atrophy, although some creams may cause adverse effects. Cochrane Database Syst. Rev. 2006. [Google Scholar] [CrossRef]
- Whitehead, S.J.; Kilmarx, P.H.; Blanchard, K.; Manopaiboon, C.; Chaikummao, S.; Friedland, B.; Achalapong, J.; Wankrairoj, M.; Mock, P.; Thanprasertsuk, S.; et al. Acceptability of carraguard vaginal gel use among Thai couples. AIDS 2006, 20, 2141–2148. [Google Scholar] [CrossRef]
- Mantell, J.E.; Myer, L.; Carballo-Dieguez, A.; Stein, Z.; Ramjee, G.; Morar, N.S.; Harrison, P.F. Microbicide acceptability research: Current approaches and future directions. Soc. Sci. Med. 2005, 60, 319–330. [Google Scholar] [CrossRef]
- Palmeira-de-Oliveira, A.; Silva, B.M.; Palmeira-de-Oliveira, R.; Martinez-de-Oliveira, J.; Salgueiro, L. Are plant extracts a potential therapeutic approach for genital infections? Curr. Med. Chem. 2013, 20, 2914–2928. [Google Scholar]
- Palmeira-de-Oliveira, A.; Palmeira -de-Oliveira, R.; Gaspar, C.; Salgueiro, L.; Cavaleiro, C.; Martinez-de-Oliveira, J.; Queiroz, J.A.; Rodrigues, A.G. Association of Thymbra capitata essential oil and chitosan (TCCH hydrogel): A putative therapeutic tool for the treatment of vulvovaginal candidosis. Flavour Fragr. J. 2013, 28, 354–359. [Google Scholar] [CrossRef]
- Jordan, S.A.; Cunningham, D.G.; Marles, R.J. Assessment of herbal medicinal products: Challenges, and opportunities to increase the knowledge base for safety assessment. Toxicol. Appl. Pharmacol. 2010, 243, 198–216. [Google Scholar] [CrossRef]
- Cunha, A.R.; Machado, R.M.; Palmeira-de-Oliveira, A.; Martinez-de-Oliveira, J.; das Neves, J.; Palmeira-de-Oliveira, R. Characterization of commercially available vaginal lubricants: A safety perspective. Pharmaceutics 2014, 6, 530–542. [Google Scholar] [CrossRef]
- Gordon, J.S.; McNew, R. Developing the online survey. Nurs. Clin. North Am. 2008, 43, 605–619. [Google Scholar] [CrossRef]
- Denscombe, M. The Good Research Guide: For Small-scale Social Research Projects, 2nd ed.; Open University Press: Buckingham, UK, 2003; p. 272. [Google Scholar]
- Nathanson, A.T.; Reinert, S.E. Windsurfing injuries: Results of a paper- and Internet-based survey. Wilderness Environ. Med. 1999, 10, 218–225. [Google Scholar] [CrossRef]
- Meho, L. E-mail interviewing in qualitative research: A methodological discussion. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 1284–1295. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palmeira-de-Oliveira, R.; Duarte, P.; Palmeira-de-Oliveira, A.; Das Neves, J.; Amaral, M.H.; Breitenfeld, L.; Martinez-de-Oliveira, J. What do Portuguese Women Prefer Regarding Vaginal Products? Results from a Cross-Sectional Web-Based Survey. Pharmaceutics 2014, 6, 543-556. https://doi.org/10.3390/pharmaceutics6040543
Palmeira-de-Oliveira R, Duarte P, Palmeira-de-Oliveira A, Das Neves J, Amaral MH, Breitenfeld L, Martinez-de-Oliveira J. What do Portuguese Women Prefer Regarding Vaginal Products? Results from a Cross-Sectional Web-Based Survey. Pharmaceutics. 2014; 6(4):543-556. https://doi.org/10.3390/pharmaceutics6040543
Chicago/Turabian StylePalmeira-de-Oliveira, Rita, Paulo Duarte, Ana Palmeira-de-Oliveira, José Das Neves, Maria Helena Amaral, Luiza Breitenfeld, and José Martinez-de-Oliveira. 2014. "What do Portuguese Women Prefer Regarding Vaginal Products? Results from a Cross-Sectional Web-Based Survey" Pharmaceutics 6, no. 4: 543-556. https://doi.org/10.3390/pharmaceutics6040543