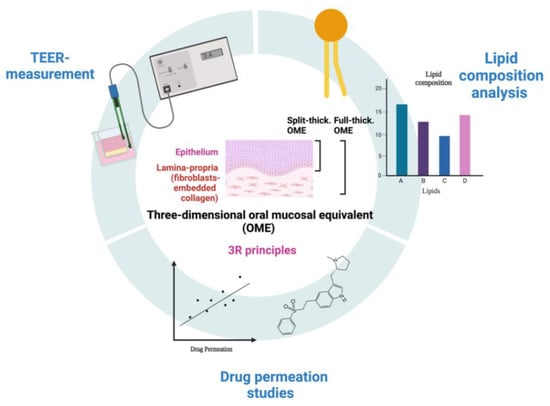
Three-Dimensional Oral Mucosal Equivalents as Models for Transmucosal Drug Permeation Studies
Abstract
:1. Introduction
1.1. Interest in Research in Mucosal Tissue
1.2. Tissue Architecture and Non-Keratinized Epithelium
1.3. Status and Unmet Need of Mucosal Equivalents for Pharmaceutical Applications
2. Materials and Methods
2.1. Materials
2.2. Composition of Cell Culture Media and Buffers
2.3. Cell Culture
2.4. Full-Thickness Tissue-Enginereed Oral Mucosa
2.4.1. Preparation of the Lamina Propria
2.4.2. Addition of Epithelial OKF6 TERT-2
2.5. Split-Thickness Tissue-Engineered Oral Mucosa
2.6. Histology of Tissue-Enginereed Oral Mucosa
2.7. Drug Permeation Studies across Tissue-Enginereed Oral Mucosa
2.8. Drug Quantification in Permeation Experiments
2.9. Transepithelial Electrical Resistance (TEER)
2.10. TEER Measurements for Evaluation of 3D Growth, Shelf-Life and Tissue Integrity
2.11. Lipid Extraction from Cell Monolayer and Tissue-Enginereed Oral Mucosa
2.12. High-Performance Thin-Layer Chromatography (HPTLC)
2.13. Data Analysis for Permeation Experiment
3. Results and Discussion
3.1. Development and Characterization of Full- and Split-Thickness Oral Mucosa Models
3.2. Assessment of Full- and Split-Thickness Oral Mucosa Models for Drug Permeation Studies
3.3. The 3R Approach (Replacement, Reduction and Refinement of Animal-Derived Ingredients) in the Tissue-Engineering Protocol
3.4. Evaluation of the Lipid Composition in Full-Thickness Tissue-Engineered Oral Mucosa
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jeyanathan, M.; Afkhami, S.; Smaill, F.; Miller, M.S.; Lichty, B.D.; Xing, Z. Immunological considerations for COVID-19 vaccine strategies. Nat. Rev. Immunol. 2020, 20, 615–632. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.F.; Liu, F.; Brown, M.B. Advances in oral transmucosal drug delivery. J. Control. Release 2011, 153, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Sattar, M.; Sayed, O.M.; Lane, M.E. Oral transmucosal drug delivery–Current status and future prospects. Int. J. Pharm. 2014, 471, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Squier, C.A.; Kremer, M.J. Biology of oral mucosa and esophagus. J. Natl. Cancer Inst. Monogr. 2001, 2001, 7–15. [Google Scholar] [CrossRef]
- Tabatabaei, F.; Moharamzadeh, K.; Tayebi, L. Three-Dimensional In Vitro Oral Mucosa Models of Fungal and Bacterial Infections. Tissue Eng. Part B Rev. 2020, 26, 443–460. [Google Scholar] [CrossRef]
- Dongari-Bagtzoglou, A.; Kashleva, H. Development of a highly reproducible three-dimensional organotypic model of the oral mucosa. Nat. Protoc. 2006, 1, 2012. [Google Scholar] [CrossRef]
- Moharamzadeh, K.; Brook, I.M.; Van Noort, R.; Scutt, A.M.; Thornhill, M.H. Tissue-engineered Oral Mucosa: A Review of the Scientific Literature. J. Dent. Res. 2007, 86, 115–124. [Google Scholar] [CrossRef]
- Jennings, L.R.; Colley, H.E.; Ong, J.; Panagakos, F.; Masters, J.G.; Trivedi, H.M.; Murdoch, C.; Whawell, S. Development and characterization of in vitro human oral mucosal equivalents derived from immortalized oral keratinocytes. Tissue Eng. Part C Methods 2016, 22, 1108–1117. [Google Scholar] [CrossRef]
- Egami, M.; Haraguchi, Y.; Shimizu, T.; Yamato, M.; Okano, T. Latest status of the clinical and industrial applications of cell sheet engineering and regenerative medicine. Arch. Pharmacal Res. 2014, 37, 96–106. [Google Scholar] [CrossRef]
- Klausner, M.; Handa, Y.; Aizawa, S. In vitro three-dimensional organotypic culture models of the oral mucosa. Vitr. Cell Dev. Biol. Anim. 2021, 57, 148–159. [Google Scholar] [CrossRef]
- Kubilus, J.; Breyfolgle, B.; Ayehunie, S.; Dale, B.; Kimball, J.R.; Wertz, P.W.; Klausner, M. Characterization and Testing of New Buccal and Gingival Tissue Models. In Proceedings of the 35th Annual Meeting of the American Association for Dental Research: MatTek Corporation, Ashland, MA, USA, March 2006. [Google Scholar]
- Dickson, M.A.; Hahn, W.C.; Ino, Y.; Ronfard, V.; Wu, J.Y.; Weinberg, R.A.; Louis, D.N.; Li, F.P.; Rheinwald, J.G. Human keratinocytes that express hTERT and also bypass a p16INK4a-enforced mechanism that limits life span become immortal yet retain normal growth and differentiation characteristics. Mol. Cell. Biol. 2000, 20, 1436–1447. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.R.; Svensäter, G.; Herzberg, M.C. Identification of novel LPXTG-linked surface proteins from Streptococcus gordonii. Microbiology 2009, 155, 1977. [Google Scholar] [CrossRef] [PubMed]
- Dongari-Bagtzoglou, A.; Kashleva, H. Development of a novel three-dimensional in vitro model of oral Candida infection. Microb. Pathog. 2006, 40, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Eder, C.; Falkner, E.; Nehrer, S.; Losert, U.M.; Schoeffl, H. Introducing the concept of the 3Rs into tissue engineering research. Altex 2006, 23, 17–23. [Google Scholar] [PubMed]
- Motta, S.; Monti, M.; Sesana, S.; Caputo, R.; Carelli, S.; Ghidoni, R. Ceramide composition of the psoriatic scale. Biochim. Et. Biophys. Acta (BBA)-Mol. Basis Dis. 1993, 1182, 147–151. [Google Scholar] [CrossRef]
- van Smeden, J.; Janssens, M.; Gooris, G.S.; Bouwstra, J.A. The important role of stratum corneum lipids for the cutaneous barrier function. Biochim. Biophys. Acta 2014, 1841, 295–313. [Google Scholar] [CrossRef]
- Cayir, A.; Cobanoglu, H.; Coskun, M. Assessment of the genotoxic potential of a migraine-specific drug by comet and cytokinesis-block micronucleus assays. Expert Opin. Drug Metab. Toxicol. 2020, 16, 441–446. [Google Scholar] [CrossRef]
- Valetti, S.; Riaz, A.; Doko, A.; Sultana, K.; Eskandari, M.; Prgomet, Z.; Feiler, A.; Rönn, R.; Dahlström, B.; Engblom, J.; et al. Oral transmucosal delivery of Eletriptan for neurological diseases. Int J Pharm 2022, 627, 122222. [Google Scholar] [CrossRef]
- ICH. International Conference on Harmonization, Validation of Analytical Procedures: Text and Methodology Q2(R1); ICH Harmonised Tripartite Guideline: Rockville, MD, USA, 2005; pp. 1–13. [Google Scholar]
- Boiten, W.; Absalah, S.; Vreeken, R.; Bouwstra, J.; van Smeden, J. Quantitative analysis of ceramides using a novel lipidomics approach with three dimensional response modelling. Biochim. Biophys. Acta 2016, 1861, 1652–1661. [Google Scholar] [CrossRef]
- Diaz-del Consuelo, I.; Jacques, Y.; Pizzolato, G.-P.; Guy, R.H.; Falson, F. Comparison of the lipid composition of porcine buccal and esophageal permeability barriers. Arch. Oral. Biol. 2005, 50, 981–987. [Google Scholar] [CrossRef]
- Valetti, S.; Thomsen, H.; Wankar, J.; Falkman, P.; Manet, I.; Feiler, A.; Ericson, M.B.; Engblom, J. Can mesoporous nanoparticles promote bioavailability of topical pharmaceutics? Int. J. Pharm. 2021, 602, 120609. [Google Scholar] [CrossRef] [PubMed]
- Paolo Dotto, G. Signal transduction pathways controlling the switch between keratinocyte growth and differentiation. Crit. Rev. Oral Biol. Med. 1999, 10, 442–457. [Google Scholar] [CrossRef] [PubMed]
- Yadev, N.P.; Murdoch, C.; Saville, S.P.; Thornhill, M.H. Evaluation of tissue engineered models of the oral mucosa to investigate oral candidiasis. Microb. Pathog. 2011, 50, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, B.; Kolli, A.R.; Esch, M.B.; Abaci, H.E.; Shuler, M.L.; Hickman, J.J. TEER measurement techniques for in vitro barrier model systems. J. Lab. Autom. 2015, 20, 107–126. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, J.; van Deurs, B.; Pedersen, M.; Rassing, M.R. TR146 cells grown on filters as a model for human buccal epithelium: I. Morphology, growth, barrier properties, and permeability. Int. J. Pharm. 1995, 125, 165–184. [Google Scholar] [CrossRef]
- Klausner, M.; Ayehunie, S.; Breyfogle, B.A.; Wertz, P.W.; Bacca, L.; Kubilus, J. Organotypic human oral tissue models for toxicological studies. Toxicol. Vitr. 2007, 21, 938–949. [Google Scholar] [CrossRef]
- Gidvall, S.; Björklund, S.; Feiler, A.; Dahlström, B.; Rönn, R.; Engblom, J.; Valetti, S. A novel versatile flow-donor chamber as biorelevant ex-vivo test assessing oral mucoadhesive formulations. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2021, 166, 105983. [Google Scholar] [CrossRef]
- Van Der Valk, J.; Bieback, K.; Buta, C.; Cochrane, B.; Dirks, W.; Fu, J.; Hickman, J.; Hohensee, C.; Kolar, R.; Liebsch, M. Fetal bovine serum (FBS): Past–present–future. Altex 2018, 35, 98–118. [Google Scholar] [CrossRef]
- Suzuki, A.; Sekiya, S.; Gunshima, E.; Fujii, S.; Taniguchi, H. EGF signaling activates proliferation and blocks apoptosis of mouse and human intestinal stem/progenitor cells in long-term monolayer cell culture. Lab. Investig. 2010, 90, 1425–1436. [Google Scholar] [CrossRef]
- Kautsky, M.B.; Fleckman, P.; Dale, B.A. Retinoic Acid Regulates Oral Epithelial Differentiation by Two Mechanisms. J. Investig. Dermatol. 1995, 104, 224–230. [Google Scholar] [CrossRef]
- Abidin, F.Z.; Gouveia, R.M.; Connon, C.J. Application of retinoic acid improves form and function of tissue engineered corneal construct. Organogenesis 2015, 11, 122–136. [Google Scholar] [CrossRef] [PubMed]
- Ouellette, M.-È.; Bérubé, J.-C.; Bourget, J.-M.; Vallée, M.; Bossé, Y.; Fradette, J. Linoleic acid supplementation of cell culture media influences the phospholipid and lipid profiles of human reconstructed adipose tissue. PLoS ONE 2019, 14, e0224228. [Google Scholar] [CrossRef] [PubMed]
- Madison, K.C.; Wertz, P.W.; Strauss, J.S.; Downing, D.T. Lipid composition of cultured murine keratinocytes. J. Investig. Dermatol. 1986, 87, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Kent, K.D.; Bomser, J.A. Bovine pituitary extract provides remarkable protection against oxidative stress in human prostate epithelial cells. Vitr. Cell. Dev. Biol. -Anim. 2003, 39, 388–394. [Google Scholar] [CrossRef]
- Selvaratnam, L.; Cruchley, A.T.; Navsaria, H.; Wertz, P.W.; Hagi-Pavli, E.P.; Leigh, I.M.; Squier, C.A.; Williams, D.M. Permeability barrier properties of oral keratinocyte cultures: A model of intact human oral mucosa. Oral. Dis. 2001, 7, 252–258. [Google Scholar] [CrossRef]
- Squier, C.A. The permeability of oral mucosa. Crit. Rev. Oral Biol. Med. Off. Publ. Am. Assoc. Oral Biol. 1991, 2, 13–32. [Google Scholar] [CrossRef]
- Vannet, B.V.; De Wever, B.; Adriaens, E.; Ramaeckers, F.; Bottenberg, P. The evaluation of sodium lauryl sulphate in toothpaste on toxicity on human gingiva and mucosa: A 3D in vitro model. Dentistry 2015, 5, 1000325. [Google Scholar] [CrossRef]
- Patel, V.F.; Liu, F.; Brown, M.B. Modeling the oral cavity: In vitro and in vivo evaluations of buccal drug delivery systems. J. Control. Release Off. J. Control. Release Soc. 2012, 161, 746–756. [Google Scholar] [CrossRef]
- Ponec, M.; Weerheim, A.; Kempenaar, J.; Mommaas, A.M.; Nugteren, D.H. Lipid composition of cultured human keratinocytes in relation to their differentiation. J. Lipid. Res. 1988, 29, 949–961. [Google Scholar] [CrossRef]
- Schmidt, R.; Parish, E.J.; Dionisius, V.; Cathelineau, C.; Michel, S.; Shroot, B.; Rolland, A.; Brzokewicz, A.; Reichert, U. Modulation of Cellular Cholesterol and Its Effect on Cornified Envelope Formation in Cultured Human Epidermal Keratinocytes. J. Investig. Dermatol. 1991, 97, 771–775. [Google Scholar] [CrossRef]
- Law, S.; Wertz, P.W.; Swartzendruber, D.C.; Squier, C.A. Regional variation in content, composition and organization of porcine epithelial barrier lipids revealed by thin-layer chromatography and transmission electron microscopy. Arch. Oral. Biol. 1995, 40, 1085–1091. [Google Scholar] [CrossRef] [PubMed]







| Sample | TEER Reported (Ω·cm2) | |||
|---|---|---|---|---|
| After ALI Differentiation | 1 Week Shelf Life | Directly after Drug Permeation Studies | 24 h Recovery after Drug Permeation Studies | |
| Full-thickness mucosa | 118 ± 8 | 112 ± 32 | 79 ± 5 * | 87 ± 43 |
| Split-thickness mucosa | 140 ± 50 | 143 ± 51 | 97 ± 41 * | 110 ± 53 |
| EpiOral™ | 134 ± 28 | 24 ± 24 | 40 ± 40 | 44 ± 3 |
| Membrane | J (µg/cm2/h) | SD (µg/cm2/h) | R2 |
|---|---|---|---|
| EpiOral™ | 28.8 | 0.006 | 0.972 |
| Full-thickness oral mucosa | 29.6 | 0.003 | 0.998 |
| Split-thickness oral mucosa | 106.3 | 0.106 | 0.998 |
| Collagen (acellular + cellular) | 70.7 | 0.007 | 0.991 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riaz, A.; Gidvall, S.; Prgomet, Z.; Hernandez, A.R.; Ruzgas, T.; Nilsson, E.J.; Davies, J.; Valetti, S. Three-Dimensional Oral Mucosal Equivalents as Models for Transmucosal Drug Permeation Studies. Pharmaceutics 2023, 15, 1513. https://doi.org/10.3390/pharmaceutics15051513
Riaz A, Gidvall S, Prgomet Z, Hernandez AR, Ruzgas T, Nilsson EJ, Davies J, Valetti S. Three-Dimensional Oral Mucosal Equivalents as Models for Transmucosal Drug Permeation Studies. Pharmaceutics. 2023; 15(5):1513. https://doi.org/10.3390/pharmaceutics15051513
Chicago/Turabian StyleRiaz, Azra, Sanna Gidvall, Zdenka Prgomet, Aura Rocio Hernandez, Tautgirdas Ruzgas, Emelie J. Nilsson, Julia Davies, and Sabrina Valetti. 2023. "Three-Dimensional Oral Mucosal Equivalents as Models for Transmucosal Drug Permeation Studies" Pharmaceutics 15, no. 5: 1513. https://doi.org/10.3390/pharmaceutics15051513