1. Introduction
Orodispersible films (ODFs) are single-layer or multi-layer thin polymer sheets intended for rapid dissolution or disintegration in the oral cavity. They are usually applied directly to the tongue (Ph. Eur.) [
1]. The FDA defines ODFs as a thin dosage form that disintegrates rapidly upon contact with a liquid [
2]. A suitable ODF should be thin and flexible but resistant enough to be easily used and simply packed. The film should not be sticky and hold the form without rolling. Another important aspect is the pleasant taste and low irritability. The disintegration time should be as short as possible [
3]. Most of these properties are influenced by the content of water or other plasticizers in the film structure.
ODFs are still not a common dosage form. However, oral films can be found in patent literature from the 1960s. Pfizer was the first company to start manufacturing breath freshener Listerine
® PocketPaks in 2001 [
4]. In 2003 the first oral film with API (Chloraseptic
® with benzocaine for sore throat treatment) was rolled out, followed by the first oral strip containing a prescription drug (Ondasetron Rapidfilm
®, antiemetic), registered in 2010 [
4,
5].
ODFs, as an innovative dosage form, take advantage of simple application and rapid disintegration in the mouth, suitable for patients with difficulty in swallowing tablets (children, geriatric patients, patients with Parkinson’s disease, dysphagia, or vomiting). ODFs can impact drugs’ therapeutic effects [
5]. They reduce side effects like gastrointestinal irritation. When the film is applied into the oral cavity, part of the active substance is absorbed directly into the bloodstream through the oral mucosa. Hence, acid degradation in the stomach may be limited, which is advantageous for drugs sensitive to low pH, and the hepatic first-pass effect is reduced, increasing bioavailability [
5].
On the other hand, oral films are burdened with certain limitations, such as the ability to incorporate only a limited amount of drugs; hence they are mainly suitable for highly effective and low dose drugs. Their production requires the use of solvents and subsequent drying, which may adversely affect the stability of the drug [
6]. The main hurdle for patients’ acceptance of ODFs is taste (most APIs are bitter or generally unpleasant). Usually, it is necessary to add sweeteners and flavorings to the composition to mask the taste of the active ingredients, which reduces the usable amount of API and may even have a deteriorative effect on the film-forming properties of the main polymer [
4,
7].
Oral films are produced in several ways. The most common is solvent casting and hot-melt extrusion. Other options are the rolling method or spraying the layers onto the first layer formed by solvent casting. The main disadvantage of these methods is the need for subsequential steps of drying and cutting to the desired shape and size [
4,
8].
In the last decade, the production of dosage forms using 3D printing has come to the fore. This technology enables on-demand fabrication of personalized medicines and customized dosage forms in a layer-by-layer fashion into the geometry represented by a digital model. By using 3D printing it is possible to create an individual medication with different release profiles, active substance content, or the shape and size of the dosage form quickly [
8,
9]. Presumably, 3D technology will improve the resulting complexity of the product and allow personalization and on-demand manufacturing since it brings in possibilities to create small batches at low cost, even in compounding pharmacies [
10,
11].
Several 3D printing technologies have already been applied in the preparation of ODFs. In 2019, personalized ODFs with warfarin were prepared by semisolid extrusion (SSE). The results confirmed excellent dose to dimension linearity and content uniformity, important for substances with a narrow therapeutic index. Since this is a one-step process, it also can be applied in on-demand hospital compounding [
12]. Another example of 3D printed ODFs are films containing aripiprazole prepared by fused deposition modeling (FDM), containing polyvinyl alcohol (PVA) as the main film-forming component. The results show that this method is certainly suitable for preparing personalized dosage forms. FDM printing also incorporates specific features, such as haptic identifiers or Braille encoding for visually impaired patients [
13].
Moreover, since no solvent is used, recrystallization issues, generally connected to SSE, are not a concern for FDM. It is even possible to enhance the solubility of the incorporated drug by solid dispersion forming through the process of hot-melt extrusion. However, FDM lacks the simplicity of SSE due to the extra work step of filament preparation and prepared ODFs suffer from prolonged disintegration time, inherent to FDM technology [
14]. In another study, orodispersible films with maltodextrins were prepared by direct extrusion of melted excipients, omitting the preparation of filaments typical for FDM. Moreover, printing the ODFs directly onto the primary packaging reduced another work step through this approach [
15,
16].
The combination of 3D printing and orodispersible forms could be a step towards automation and higher efficiency in preparing drugs tailored to a specific patient in a hospital or pharmacy. An example is the formulation of ODFs with cannabinol, which may be dosed exactly according to the patient’s weight [
4,
17].
In all the technologies for ODFs preparation (solvent casting, SSE), where excipients and active ingredients are dissolved or suspended in a solution, drying is the critical step, as it may affect the physical state of the incorporated drug and the overall properties of ODFs [
4].
When improper or uncontrolled drying is used, unstable or therapeutically unsuitable polymorphs may be present in final ODFs since drug recrystallization may be affected by the length of drying, temperature, ambient humidity, and solvent used. This may reduce treatment effectiveness or even result in adverse effects due to the presence of toxic polymorphs [
18].
Regarding ODFs’ properties, the relation between residual moisture content (RMC) and one of the main parameters of ODF quality, disintegration time, was established by Preis et al. who concluded that films of higher RMC tend to disintegrate quickly [
19]. Appropriate RMC is also crucial for plasticizing effects. The type and amount of plasticizers significantly impact ODF flexibility closely related to the ease of handling and packaging [
4,
20].
High RMC in ODFs can also lead to physical instability of the API (drug recrystallization) and to increased water activity, which facilitates microbial growth [
21]. Borges et al. proposed a range of 3–6% RMC for ODFs based on evaluating commercial ODFs of various compositions [
21]. In another study, Foo et al. manufactured orodispersible films with an RMC of 3.4–6.2%. Their mechanical and application properties were satisfactory [
22].
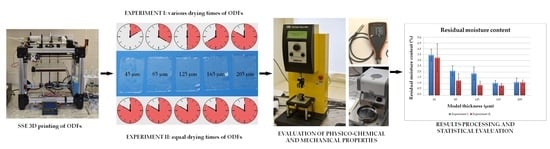
This work aimed to compare two setups of drying used to prepare ODFs by SSE 3D printing. The selected formulation was used to prepare ODFs of different thicknesses by the SSE printing method modified according to the previous experiment [
10], which was repeated to prove the reproducibility of the process. Subsequently, the drying process was modified to allow more thorough drying by equalizing drying time for all batches differing in film thicknesses. Statistical evaluation of film properties was undertaken to assess whether equalizing the drying time improves the properties of ODFs enough to justify prolonging the preparation by additional drying and to evaluate the effects of drying setup on ODFs in general.
4. Conclusions
SSE 3D printed ODFs with different drying processes were compared. Statistically significant impacts of drying time on thickness, moisture content, hardness, deformation at hardness, work at hardness, peak load, tensile work, and tensile strength were found. These impacts are caused by the change in moisture content, which affects the physico-chemical properties of the films. Statistical evaluation of ODFs properties showed that weight, disintegration, and elongation differences are not statistically dependent on the drying setup.
The films prepared using the in-process drying met the recommended limits for moisture content. The plasticizing properties of water were preserved, contributing to good mechanical properties. The sole in-process drying is an acceptable drying method.
In conclusion, using different drying setups is a suitable way to fine-tune the properties of SSE printed ODFs without compromising the weight uniformity or disintegration time. However, such tuning comes at the cost of longer preparation times, reducing the effectiveness of this manufacturing method as a tool for the preparation of ODFs.