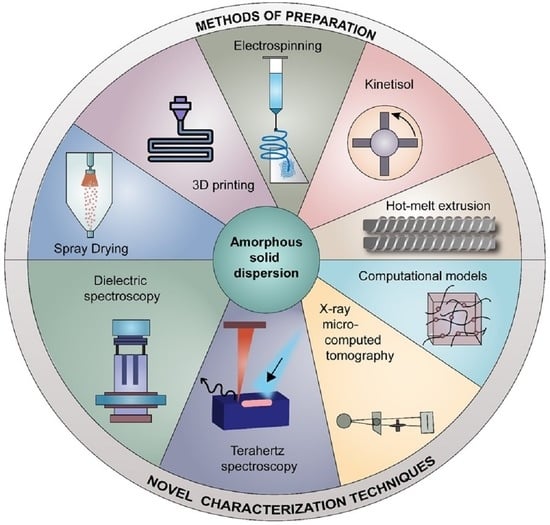
Recent Advances in Amorphous Solid Dispersions: Preformulation, Formulation Strategies, Technological Advancements and Characterization
Abstract
:1. Introduction
2. Recent Advances in Preformulation
3. Advances in ASD Formulation Approaches
3.1. Mitigating the Pill Burden by High Drug Loaded ASDs
3.2. SUBA™ Technology (via Spray Drying Process)
3.3. Use of Polymeric Combinations for Enhanced Bioavailability
3.3.1. Polymeric Combinations in HME
3.3.2. Polymer Combinations in Spray-Drying
3.4. Addition of Surfactants
3.4.1. Addition of Surfactants in HME
3.4.2. Addition of Surfactants in Spray Drying
3.4.3. Using Polymeric Salts for Enhancing Solubility
4. Recent Advancements in the Manufacturing of ASDs
4.1. Kinetisol®
4.2. 3D Printing
4.2.1. Selective Laser Sintering
4.2.2. Fused Deposition Modeling and Direct Powder Extrusion
4.3. Electronanospinning
5. Advances in Characterization Techniques
5.1. Tetrahertz Spectroscopy
5.2. Dielectric Spectroscopy
5.3. X-ray Micro-Computed Tomography
6. Computational Models for Stability Predictions
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Duong, T.V.; Nguyen, H.T.; Taylor, L.S. Combining enabling formulation strategies to generate supersaturated solutions of delamanid: In situ salt formation during amorphous solid dispersion fabrication for more robust release profiles. Eur. J. Pharm. Biopharm. 2022, 174, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Coty, J.-B.; Martin, C.; Telò, I.; Spitzer, D. Use of Spray Flash Evaporation (SFE) technology to improve dissolution of poorly soluble drugs: Case study on furosemide nanocrystals. Int. J. Pharm. 2020, 589, 119827. [Google Scholar] [CrossRef] [PubMed]
- Baghel, S.; Cathcart, H.; O’Reilly, N.J. Polymeric Amorphous Solid Dispersions: A Review of Amorphization, Crystallization, Stabilization, Solid-State Characterization, and Aqueous Solubilization of Biopharmaceutical Classification System Class II Drugs. J. Pharm. Sci. 2016, 105, 2527–2544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, Y.; Ho, C. Amorphous Solid Dispersions: Utilization and Challenges in Drug Discovery and Development. J. Pharm. Sci. 2015, 104, 3237–3258. [Google Scholar] [PubMed]
- França, M.T.; Martins Marcos, T.; Costa, P.F.A.; Bazzo, G.C.; Nicolay Pereira, R.; Gerola, A.P.; Stulzer, H.K. Eutectic mixture and amorphous solid dispersion: Two different supersaturating drug delivery system strategies to improve griseofulvin release using saccharin. Int. J. Pharm. 2022, 615, 121498. [Google Scholar] [CrossRef]
- Vasconcelos, T.; Marques, S.; das Neves, J.; Sarmento, B. Amorphous solid dispersions: Rational selection of a manufacturing process. Adv. Drug Deliv. Rev. 2016, 100, 85–101. [Google Scholar] [CrossRef]
- Ditzinger, F.; Price, D.J.; Ilie, A.-R.; Köhl, N.J.; Jankovic, S.; Tsakiridou, G.; Aleandri, S.; Kalantzi, L.; Holm, R.; Nair, A.; et al. Lipophilicity and hydrophobicity considerations in bio-enabling oral formulations approaches—A PEARRL review. J. Pharm. Pharmacol. 2018, 71, 464–482. [Google Scholar] [CrossRef] [Green Version]
- Meruva, S.; Thool, P.; Gong, Y.; Karki, S.; Bowen, W.; Kumar, S. Role of wetting agents and disintegrants in development of danazol nanocrystalline tablets. Int. J. Pharm. 2020, 577, 119026. [Google Scholar] [CrossRef] [PubMed]
- Mamidi, H.K.; Palekar, S.; Nukala, P.K.; Mishra, S.M.; Patki, M.; Fu, Y.; Supner, P.; Chauhan, G.; Patel, K. Process optimization of twin-screw melt granulation of fenofibrate using design of experiment (DoE). Int. J. Pharm. 2021, 593, 120101. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, S.; Imam, S.S.; Hussain, A.; Altamimi, M.A.; Alruwaili, N.K.; Alotaibi, F.; Alanazi, A.; Shakeel, F. Potential of solid dispersions to enhance solubility, bioavailability, and therapeutic efficacy of poorly water-soluble drugs: Newer formulation techniques, current marketed scenario and patents. Drug Deliv. 2020, 27, 1625–1643. [Google Scholar] [CrossRef] [PubMed]
- Baral, K.C.; Song, J.-G.; Lee, S.H.; Bajracharya, R.; Sreenivasulu, G.; Kim, M.; Lee, K.; Han, H.-K. Enhanced Bioavailability of AC1497, a Novel Anticancer Drug Candidate, via a Self-Nanoemulsifying Drug Delivery System. Pharmaceutics 2021, 13, 1142. [Google Scholar] [CrossRef]
- Srinivasan, P.; Almutairi, M.; Dumpa, N.; Sarabu, S.; Bandari, S.; Zhang, F.; Ashour, E.; Repka, M.A. Theophylline-nicotinamide pharmaceutical co-crystals generated using hot melt extrusion technology: Impact of polymeric carriers on processability. J. Drug. Deliv. Sci. Technol. 2021, 61, 102128. [Google Scholar] [CrossRef] [PubMed]
- Haser, A.; Zhang, F. New Strategies for Improving the Development and Performance of Amorphous Solid Dispersions. AAPS PharmSciTech 2018, 19, 978–990. [Google Scholar] [CrossRef]
- Meruva, S.; Thool, P.; Shah, S.; Karki, S.; Bowen, W.; Ghosh, I.; Kumar, S. Formulation and performance of Irbesartan nanocrystalline suspension and granulated or bead-layered dried powders—Part I. Int. J. Pharm. 2019, 568, 118189. [Google Scholar] [CrossRef]
- Sekiguchi, K.; Obi, N. Studies on Absorption of Eutectic Mixture. I. A Comparison of the Behavior of Eutectic Mixture of Sulfathiazole and that of Ordinary Sulfathiazole in Man. Chem. Pharm. Bull. 1961, 9, 866–872. [Google Scholar] [CrossRef] [Green Version]
- Kallakunta, V.R.; Sarabu, S.; Bandari, S.; Batra, A.; Bi, V.; Durig, T.; Repka, M.A. Stable amorphous solid dispersions of fenofibrate using hot melt extrusion technology: Effect of formulation and process parameters for a low glass transition temperature drug. J. Drug. Deliv. Sci. Technol. 2020, 58, 101395. [Google Scholar] [CrossRef]
- Sun, D.D.; Lee, P.I. Evolution of Supersaturation of Amorphous Pharmaceuticals: The Effect of Rate of Supersaturation Generation. Mol. Pharm. 2013, 10, 4330–4346. [Google Scholar] [CrossRef] [PubMed]
- Bhujbal, S.V.; Mitra, B.; Jain, U.; Gong, Y.; Agrawal, A.; Karki, S.; Taylor, L.S.; Kumar, S.; Zhou, Q. Pharmaceutical amorphous solid dispersion: A review of manufacturing strategies. Acta Pharm. Sin. B 2021, 11, 2505–2536. [Google Scholar] [PubMed]
- Almotairy, A.; Almutairi, M.; Althobaiti, A.; Alyahya, M.; Sarabu, S.; Alzahrani, A.; Zhang, F.; Bandari, S.; Repka, M.A. Effect of pH modifiers on the solubility, dissolution rate, and stability of telmisartan solid dispersions produced by hot-melt extrusion technology. J. Drug. Deliv. Sci. Technol. 2021, 65, 102674. [Google Scholar] [CrossRef]
- Newman, A.; Knipp, G.; Zografi, G. Assessing the performance of amorphous solid dispersions. J. Pharm. Sci. 2012, 101, 1355–1377. [Google Scholar] [CrossRef]
- Xie, T.; Taylor, L.S. Effect of Temperature and Moisture on the Physical Stability of Binary and Ternary Amorphous Solid Dispersions of Celecoxib. J. Pharm. Sci. 2017, 106, 100–110. [Google Scholar] [CrossRef] [Green Version]
- Quilló, G.L.; Bhonsale, S.; Gielen, B.; Van Impe, J.F.; Collas, A.; Xiouras, C. Crystal Growth Kinetics of an Industrial Active Pharmaceutical Ingredient: Implications of Different Representations of Supersaturation and Simultaneous Growth Mechanisms. Cryst. Growth Des. 2021, 21, 5403–5420. [Google Scholar] [CrossRef]
- Ashwathy, P.; Anto, A.T.; Sudheesh, M.S. A mechanistic review on the dissolution phase behavior and supersaturation stabilization of amorphous solid dispersions. Drug Dev. Ind. Pharm. 2021, 47, 1–11. [Google Scholar] [CrossRef]
- Bolla, P.K. Formulation Strategies to Enhance Solubility and Permeability of Small Molecules for Drug Delivery Applications. Ph.D. Thesis, University of Texas at El Paso, El Paso, TX, USA, 2020. [Google Scholar]
- Kaushik, R.; Budhwar, V.; Kaushik, D. An Overview on Recent Patents and Technologies on Solid Dispersion. Recent Pat. Drug Deliv. Formul. 2020, 14, 63–74. [Google Scholar] [CrossRef]
- Wilson, V.R.; Lou, X.; Osterling, D.J.; Stolarik, D.F.; Jenkins, G.J.; Nichols, B.L.B.; Dong, Y.; Edgar, K.J.; Zhang, G.G.Z.; Taylor, L.S. Amorphous solid dispersions of enzalutamide and novel polysaccharide derivatives: Investigation of relationships between polymer structure and performance. Sci. Rep. 2020, 10, 18535. [Google Scholar] [CrossRef]
- Pandi, P.; Bulusu, R.; Kommineni, N.; Khan, W.; Singh, M. Amorphous solid dispersions: An update for preparation, characterization, mechanism on bioavailability, stability, regulatory considerations and marketed products. Int. J. Pharm. 2020, 586, 119560. [Google Scholar] [CrossRef]
- Vasconcelos, T.; Sarmento, B.; Costa, P. Solid dispersions as strategy to improve oral bioavailability of poor water soluble drugs. Drug Discov. Today 2007, 12, 1068–1075. [Google Scholar] [CrossRef]
- Tan, D.K.; Davis, D.A.; Miller, D.A.; Williams, R.O.; Nokhodchi, A. Innovations in Thermal Processing: Hot-Melt Extrusion and KinetiSol® Dispersing. AAPS PharmSciTech 2020, 21, 312. [Google Scholar] [CrossRef]
- Thakkar, R.; Jara, M.O.; Swinnea, S.; Pillai, A.R.; Maniruzzaman, M. Impact of Laser Speed and Drug Particle Size on Selective Laser Sintering 3D Printing of Amorphous Solid Dispersions. Pharmaceutics 2021, 13, 1149. [Google Scholar] [CrossRef]
- Nukala, P.K.; Palekar, S.; Solanki, N.; Fu, Y.; Patki, M.; Shohatee, A.A.; Trombetta, L.; Patel, K. Investigating the application of FDM 3D printing pattern in preparation of patient-tailored dosage forms. J. 3D Print. Med. 2019, 3, 23–37. [Google Scholar] [CrossRef]
- Józó, M.; Simon, N.; Yi, L.; Móczó, J.; Pukánszky, B. Improved Release of a Drug with Poor Water Solubility by Using Electrospun Water-Soluble Polymers as Carriers. Pharmaceutics 2022, 14, 34. [Google Scholar] [CrossRef]
- Górniak, A.; Złocińska, A.; Trojan, M.; Pęcak, A.; Karolewicz, B. Preformulation Studies of Ezetimibe-Simvastatin Solid Dispersions in the Development of Fixed-Dose Combinations. Pharmaceutics 2022, 14, 912. [Google Scholar] [CrossRef]
- Zhang, L.; Luan, H.; Lu, W.; Wang, H. Preformulation Studies and Enabling Formulation Selection for an Insoluble Compound at Preclinical Stage-From In Vitro, In Silico to In Vivo. J. Pharm. Sci. 2020, 109, 950–958. [Google Scholar] [CrossRef] [Green Version]
- Shah, H.S.; Chaturvedi, K.; Kuang, S.; Wang, J. Accelerating pre-formulation investigations in early drug product life cycles using predictive methodologies and computational algorithms. Ther. Deliv. 2021, 12, 789–797. [Google Scholar] [CrossRef]
- Santitewagun, S.; Thakkar, R.; Zeitler, J.A.; Maniruzzaman, M. Detecting Crystallinity Using Terahertz Spectroscopy in 3D Printed Amorphous Solid Dispersions. Mol. Pharm. 2022, 19, 2380–2389. [Google Scholar] [CrossRef]
- S’ari, M.; Blade, H.; Cosgrove, S.; Drummond-Brydson, R.; Hondow, N.; Hughes, L.P.; Brown, A. Characterization of Amorphous Solid Dispersions and Identification of Low Levels of Crystallinity by Transmission Electron Microscopy. Mol. Pharm. 2021, 18, 1905–1919. [Google Scholar] [CrossRef]
- Ma, X.; Williams, R.O. Characterization of amorphous solid dispersions: An update. J. Drug. Deliv. Sci. Technol. 2019, 50, 113–124. [Google Scholar] [CrossRef]
- Iyer, R.; Petrovska Jovanovska, V.; Berginc, K.; Jaklič, M.; Fabiani, F.; Harlacher, C.; Huzjak, T.; Sanchez-Felix, M.V. Amorphous Solid Dispersions (ASDs): The Influence of Material Properties, Manufacturing Processes and Analytical Technologies in Drug Product Development. Pharmaceutics 2021, 13, 1682. [Google Scholar] [CrossRef]
- Bhujbal, S.V.; Zemlyanov, D.Y.; Cavallaro, A.; Mangal, S.; Taylor, L.S.; Zhou, Q.T. Qualitative and Quantitative Characterization of Composition Heterogeneity on the Surface of Spray Dried Amorphous Solid Dispersion Particles by an Advanced Surface Analysis Platform with High Surface Sensitivity and Superior Spatial Resolution. Mol. Pharm. 2018, 15, 2045–2053. [Google Scholar] [CrossRef]
- Hancock, B.C.; Chauhan, H.V. Special Topic Cluster of Articles on “Advancement in the Formulation, Characterization and Performance of Amorphous Solid Dispersions (ASDs)”. J. Pharm. Sci. 2021, 110, 1431. [Google Scholar] [CrossRef]
- Lee, W.Y.T.; Boersen, A.N.; Hui, H.W.; Chow, S.F.; Wan, K.Y.; Chow, H.L.A. Delivery of Poorly Soluble Compounds by Amorphous Solid Dispersions. Curr. Pharm. Des. 2014, 20, 303–324. [Google Scholar] [CrossRef]
- Baird, J.A.; Taylor, L.S. Evaluation of amorphous solid dispersion properties using thermal analysis techniques. Adv. Drug Deliv. Rev. 2012, 64, 396–421. [Google Scholar] [CrossRef]
- Mamidi, H.K. Preformulation Studies for the Preparation of Amorphous Solid Dispersions. Ph.D. Thesis, Saint John’s University, New York, NY, USA, 2021. [Google Scholar]
- Jia, W.; Yawman, P.D.; Pandya, K.M.; Sluga, K.; Ng, T.; Kou, D.; Nagapudi, K.; Luner, P.E.; Zhu, A.; Zhang, S.; et al. Assessing the Interrelationship of Microstructure, Properties, Drug Release Performance, and Preparation Process for Amorphous Solid Dispersions Via Noninvasive Imaging Analytics and Material Characterization. Pharm. Res. 2022. [Google Scholar] [CrossRef] [PubMed]
- Rask, M.B.; Knopp, M.M.; Olesen, N.E.; Holm, R.; Rades, T. Comparison of two DSC-based methods to predict drug-polymer solubility. Int. J. Pharm. 2018, 540, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Chen, H.; Wang, Y.; Wang, R.; Xu, J.; Zhang, C. Amorphous Solid Dispersions: Role of the Polymer and Its Importance in Physical Stability and In Vitro Performance. Pharmaceutics 2022, 14, 1747. [Google Scholar] [CrossRef] [PubMed]
- Mathers, A.; Hassouna, F.; Klajmon, M.; Fulem, M. Comparative Study of DSC-Based Protocols for API–Polymer Solubility Determination. Mol. Pharm. 2021, 18, 1742–1757. [Google Scholar] [CrossRef]
- Anane-Adjei, A.B.; Jacobs, E.; Nash, S.C.; Askin, S.; Soundararajan, R.; Kyobula, M.; Booth, J.; Campbell, A. Amorphous solid dispersions: Utilization and challenges in preclinical drug development within AstraZeneca. Int. J. Pharm. 2022, 614, 121387. [Google Scholar] [CrossRef]
- Mamidi, H.K.; Rohera, B.D. Material-Sparing Approach using Differential Scanning Calorimeter and Response Surface Methodology for Process Optimization of Hot-Melt Extrusion. J. Pharm. Sci. 2021, 110, 3838–3850. [Google Scholar] [CrossRef]
- Blaabjerg, L.I.; Bulduk, B.; Lindenberg, E.; Löbmann, K.; Rades, T.; Grohganz, H. Influence of Glass Forming Ability on the Physical Stability of Supersaturated Amorphous Solid Dispersions. J. Pharm. Sci. 2019, 108, 2561–2569. [Google Scholar] [CrossRef]
- Baird, J.A.; Van Eerdenbrugh, B.; Taylor, L.S. A Classification System to Assess the Crystallization Tendency of Organic Molecules from Undercooled Melts. J. Pharm. Sci. 2010, 99, 3787–3806. [Google Scholar] [CrossRef]
- Nurzyńska, K.; Booth, J.; Roberts, C.J.; McCabe, J.; Dryden, I.; Fischer, P.M. Long-Term Amorphous Drug Stability Predictions Using Easily Calculated, Predicted, and Measured Parameters. Mol. Pharm. 2015, 12, 3389–3398. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Qian, K.; Jacobs, E.; Amstad, E.; Jones, D.S.; Stella, L.; Andrews, G.P. The Investigation of Flory–Huggins Interaction Parameters for Amorphous Solid Dispersion Across the Entire Temperature and Composition Range. Pharmaceutics 2019, 11, 420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mamidi, H.K.; Rohera, B.D. Application of Thermodynamic Phase Diagrams and Gibbs Free Energy of Mixing for Screening of Polymers for Their Use in Amorphous Solid Dispersion Formulation of a Non-Glass-Forming Drug. J. Pharm. Sci. 2021, 110, 2703–2717. [Google Scholar] [CrossRef] [PubMed]
- Dohrn, S.; Luebbert, C.; Lehmkemper, K.; Kyeremateng, S.O.; Degenhardt, M.; Sadowski, G. Solvent influence on the phase behavior and glass transition of Amorphous Solid Dispersions. Eur. J. Pharm. Biopharm. 2021, 158, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Mendonsa, N.; Almutairy, B.; Kallakunta, V.R.; Sarabu, S.; Thipsay, P.; Bandari, S.; Repka, M.A. Manufacturing strategies to develop amorphous solid dispersions: An overview. J. Drug. Deliv. Sci. Technol. 2020, 55, 101459. [Google Scholar] [CrossRef] [PubMed]
- Nukala, P.K.; Palekar, S.; Patki, M.; Fu, Y.; Patel, K. Multi-dose oral abuse deterrent formulation of loperamide using hot melt extrusion. Int. J. Pharm. 2019, 569, 118629. [Google Scholar] [CrossRef]
- Tambe, S.; Jain, D.; Agarwal, Y.; Amin, P. Hot-melt extrusion: Highlighting recent advances in pharmaceutical applications. J. Drug. Deliv. Sci. Technol. 2021, 63, 102452. [Google Scholar] [CrossRef]
- Juluri, A.; Popescu, C.; Zhou, L.; Murthy, R.N.; Gowda, V.K.; Kumar, C.P.; Pimparade, M.B.; Repka, M.A.; Murthy, S.N. Taste Masking of Griseofulvin and Caffeine Anhydrous Using Kleptose Linecaps DE17 by Hot Melt Extrusion. AAPS PharmSciTech 2016, 17, 99–105. [Google Scholar] [CrossRef]
- Kotamarthy, L.; Feng, X.; Alayoubi, A.; Kumar Bolla, P.; Ramachandran, R.; Ashraf, M.; O’Connor, T.; Zidan, A. Switching from batch to continuous granulation: A case study of metoprolol succinate ER tablets. Int. J. Pharm. 2022, 617, 121598. [Google Scholar] [CrossRef]
- Manda, P.; Popescu, C.; Juluri, A.; Janga, K.; Kakulamarri, P.R.; Narishetty, S.; Narasimha Murthy, S.; Repka, M.A. Micronized Zaleplon Delivery via Orodispersible Film and Orodispersible Tablets. AAPS PharmSciTech 2018, 19, 1358–1366. [Google Scholar] [CrossRef]
- Jain, D.D.; Tambe, S.M.; Amin, P.D. Formulation performance window for manufacturing cellulose-based sustained-release mini-matrices of highly water-soluble drug via hot-melt extrusion technology. Cellulose 2022, 29, 3323–3350. [Google Scholar] [CrossRef]
- Jain, D.D.; Tambe, S.M.; Amin, P.D. Oral Controlled Drug Delivery by Hot-Melt Extrusion Technology. In Advancements in Controlled Drug Delivery Systems; Verma, S., Verma, S.K., Eds.; IGI Global: Hershey, PA, USA, 2022; pp. 205–236. [Google Scholar]
- Wang, B.; Liu, F.; Xiang, J.; He, Y.; Zhang, Z.; Cheng, Z.; Liu, W.; Tan, S. A critical review of spray-dried amorphous pharmaceuticals: Synthesis, analysis and application. Int. J. Pharm. 2021, 594, 120165. [Google Scholar] [CrossRef] [PubMed]
- Baumann, J.M.; Adam, M.S.; Wood, J.D. Engineering Advances in Spray Drying for Pharmaceuticals. Annu. Rev. Chem. Biomol. Eng. 2021, 12, 217–240. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Van den Mooter, G. Spray drying formulation of amorphous solid dispersions. Adv. Drug Deliv. Rev. 2016, 100, 27–50. [Google Scholar] [CrossRef]
- Vig, B.; Morgen, M. Chapter 30—Formulation, Process Development, and Scale-Up: Spray-Drying Amorphous Solid Dispersions for Insoluble Drugs. In Developing Solid Oral Dosage Forms, 2nd ed.; Qiu, Y., Chen, Y., Zhang, G.G.Z., Yu, L., Mantri, R.V., Eds.; Academic Press: Boston, MA, USA, 2017; pp. 793–820. [Google Scholar]
- Stagner, W.C.; Iyer, M.; Rathod, V.; Meruva, S.; Staton, S.; Haware, R.V. Human volunteer, in vitro, and molecular level evaluation of an optimized taste-masked isoniazid-chitosan spray-dried microparticle matrix. Int. J. Pharm. 2019, 572, 118774. [Google Scholar] [CrossRef]
- Srinarong, P.; de Waard, H.; Frijlink, H.W.; Hinrichs, W.L.J. Improved dissolution behavior of lipophilic drugs by solid dispersions: The production process as starting point for formulation considerations. Expert Opin. Drug Deliv. 2011, 8, 1121–1140. [Google Scholar] [CrossRef]
- Qian, K.; Stella, L.; Jones, D.S.; Andrews, G.P.; Du, H.; Tian, Y. Drug-Rich Phases Induced by Amorphous Solid Dispersion: Arbitrary or Intentional Goal in Oral Drug Delivery? Pharmaceutics 2021, 13, 889. [Google Scholar] [CrossRef]
- Mudie, D.M.; Buchanan, S.; Stewart, A.M.; Smith, A.; Shepard, K.B.; Biswas, N.; Marshall, D.; Ekdahl, A.; Pluntze, A.; Craig, C.D.; et al. A novel architecture for achieving high drug loading in amorphous spray dried dispersion tablets. Int. J. Pharm. X 2020, 2, 100042. [Google Scholar] [CrossRef]
- Mudie, D.M.; Stewart, A.M.; Biswas, N.; Brodeur, T.J.; Shepard, K.B.; Smith, A.; Morgen, M.M.; Baumann, J.M.; Vodak, D.T. Novel High-Drug-Loaded Amorphous Dispersion Tablets of Posaconazole; In Vivo and In Vitro Assessment. Mol. Pharm. 2020, 17, 4463–4472. [Google Scholar] [CrossRef]
- Bechtold, M.K.; Packhaeuser, C.B.; Fastnacht, K.M.; Liepold, B.H.; Steitz, B.; Cahill, J.K.; Lennon, K.J. Immediate release pharmaceutical formulation of 4-[3-(4-cyclopropanecarbonyl-piperazine-1-carbonyl)-4-fluoro-benzyl]-2H-phthalazin-1-one. U.S. Patent 8,475,842, 2 July 2013. [Google Scholar]
- Mudge, S.J.; Hayes, D.; Lukas, S. Itraconazole compositions and dosage forms, and methods of using the same. U.S. Patent 9,272,046, 1 March 2016. [Google Scholar]
- Available online: https://tolsura.com/ (accessed on 4 July 2022).
- Rauseo, A.M.; Mazi, P.; Lewis, P.; Burnett, B.; Mudge, S.; Spec, A. Bioavailability of Single-Dose SUBA-Itraconazole Compared to Conventional Itraconazole under Fasted and Fed Conditions. Antimicrob. Agents Chemother. 2021, 65, e0013421. [Google Scholar] [CrossRef]
- Butreddy, A.; Sarabu, S.; Almutairi, M.; Ajjarapu, S.; Kolimi, P.; Bandari, S.; Repka, M.A. Hot-melt extruded hydroxypropyl methylcellulose acetate succinate based amorphous solid dispersions: Impact of polymeric combinations on supersaturation kinetics and dissolution performance. Int. J. Pharm. 2022, 615, 121471. [Google Scholar] [CrossRef] [PubMed]
- Butreddy, A. Hydroxypropyl methylcellulose acetate succinate as an exceptional polymer for amorphous solid dispersion formulations: A review from bench to clinic. Eur. J. Pharm. Biopharm. 2022, 177, 289–307. [Google Scholar] [CrossRef] [PubMed]
- Wlodarski, K.; Zhang, F.; Liu, T.; Sawicki, W.; Kipping, T. Synergistic Effect of Polyvinyl Alcohol and Copovidone in Itraconazole Amorphous Solid Dispersions. Pharm. Res. 2018, 35, 16. [Google Scholar] [CrossRef] [PubMed]
- Pöstges, F.; Kayser, K.; Stoyanov, E.; Wagner, K.G. Boost of solubility and supersaturation of celecoxib via synergistic interactions of methacrylic acid-ethyl acrylate copolymer (1:1) and hydroxypropyl cellulose in ternary amorphous solid dispersions. Int. J. Pharm. X 2022, 4, 100115. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, S.; Wang, S.; Liu, C.; Su, C.; Hageman, M.; Hussain, M.; Haskell, R.; Stefanski, K.; Qian, F. Initial Drug Dissolution from Amorphous Solid Dispersions Controlled by Polymer Dissolution and Drug-Polymer Interaction. Pharm. Res. 2016, 33, 2445–2458. [Google Scholar] [CrossRef]
- Monschke, M.; Wagner, K.G. Impact of HPMCAS on the Dissolution Performance of Polyvinyl Alcohol Celecoxib Amorphous Solid Dispersions. Pharmaceutics 2020, 12, 541. [Google Scholar] [CrossRef]
- Everaerts, M.; Cools, L.; Adriaensens, P.; Reekmans, G.; Baatsen, P.; Van den Mooter, G. Investigating the Potential of Ethyl Cellulose and a Porosity-Increasing Agent as a Carrier System for the Formulation of Amorphous Solid Dispersions. Mol. Pharm. 2022, 19, 2712–2724. [Google Scholar] [CrossRef]
- Ohyagi, N.; Ueda, K.; Higashi, K.; Yamamoto, K.; Kawakami, K.; Moribe, K. Synergetic Role of Hypromellose and Methacrylic Acid Copolymer in the Dissolution Improvement of Amorphous Solid Dispersions. J. Pharm. Sci. 2017, 106, 1042–1050. [Google Scholar] [CrossRef]
- Rahman, M.; Coelho, A.; Tarabokija, J.; Ahmad, S.; Radgman, K.; Bilgili, E. Synergistic and antagonistic effects of various amphiphilic polymer combinations in enhancing griseofulvin release from ternary amorphous solid dispersions. Eur. J. Pharm. Sci. 2020, 150, 105354. [Google Scholar] [CrossRef]
- Kalhapure, R.S.; Bolla, P.K.; Boddu, S.H.; Renukuntla, J. Evaluation of Oleic Acid and Polyethylene Glycol Monomethyl Ether Conjugate (PEGylated Oleic Acid) as a Solubility Enhancer of Furosemide. Processes 2019, 7, 520. [Google Scholar] [CrossRef]
- Kapourani, A.; Tzakri, T.; Valkanioti, V.; Kontogiannopoulos, K.N.; Barmpalexis, P. Drug crystal growth in ternary amorphous solid dispersions: Effect of surfactants and polymeric matrix-carriers. Int. J. Pharm. X 2021, 3, 100086. [Google Scholar] [CrossRef] [PubMed]
- Saboo, S.; Bapat, P.; Moseson, D.E.; Kestur, U.S.; Taylor, L.S. Exploring the Role of Surfactants in Enhancing Drug Release from Amorphous Solid Dispersions at Higher Drug Loadings. Pharmaceutics 2021, 13, 735. [Google Scholar] [CrossRef] [PubMed]
- Siriwannakij, N.; Heimbach, T.; Serajuddin, A.T.M. Aqueous Dissolution and Dispersion Behavior of Polyvinylpyrrolidone Vinyl Acetate-based Amorphous Solid Dispersion of Ritonavir Prepared by Hot-Melt Extrusion with and without Added Surfactants. J. Pharm. Sci. 2021, 110, 1480–1494. [Google Scholar] [CrossRef]
- Yang, L.; Wu, P.; Xu, J.; Xie, D.; Wang, Z.; Wang, Q.; Chen, Y.; Li, C.H.; Zhang, J.; Chen, H.; et al. Correction to: Development of Apremilast Solid Dispersion Using TPGS and PVPVA with Enhanced Solubility and Bioavailability. AAPS PharmSciTech 2021, 22, 176. [Google Scholar] [CrossRef] [PubMed]
- Indulkar, A.S.; Lou, X.; Zhang, G.G.Z.; Taylor, L.S. Role of Surfactants on Release Performance of Amorphous Solid Dispersions of Ritonavir and Copovidone. Pharm. Res. 2022, 39, 381–397. [Google Scholar] [CrossRef]
- Yen, C.-W.; Kuhn, R.; Hu, C.; Zhang, W.; Chiang, P.-C.; Chen, J.Z.; Hau, J.; Estevez, A.; Nagapudi, K.; Leung, D.H. Impact of surfactant selection and incorporation on in situ nanoparticle formation from amorphous solid dispersions. Int. J. Pharm. 2021, 607, 120980. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Taylor, L.S. Improved dissolution of an enteric polymer and its amorphous solid dispersions by polymer salt formation. Int. J. Pharm. 2022, 622, 121886. [Google Scholar] [CrossRef]
- Ellenberger, D.J.; Miller, D.A.; Williams, R.O. Expanding the Application and Formulation Space of Amorphous Solid Dispersions with KinetiSol®: A Review. AAPS PharmSciTech 2018, 19, 1933–1956. [Google Scholar] [CrossRef]
- DiNunzio, J.C.; Brough, C.; Hughey, J.R.; Miller, D.A.; Williams, R.O.; McGinity, J.W. Fusion production of solid dispersions containing a heat-sensitive active ingredient by hot melt extrusion and Kinetisol® dispersing. Eur. J. Pharm. Biopharm. 2010, 74, 340–351. [Google Scholar] [CrossRef]
- Miller, D.A.; Keen, J.M. KinetiSol®-Based Amorphous Solid Dispersions. In Amorphous Solid Dispersions: Theory and Practice; Shah, N., Sandhu, H., Choi, D.S., Chokshi, H., Malick, A.W., Eds.; Springer: New York, NY, USA, 2014; pp. 567–577. [Google Scholar]
- Palekar, S.; Nukala, P.K.; Mishra, S.M.; Kipping, T.; Patel, K. Application of 3D printing technology and quality by design approach for development of age-appropriate pediatric formulation of baclofen. Int. J. Pharm. 2019, 556, 106–116. [Google Scholar] [CrossRef]
- Nukala, P.K.; Palekar, S.; Patki, M.; Patel, K. Abuse Deterrent Immediate Release Egg-Shaped Tablet (Egglets)Using 3D Printing Technology: Quality by Design to Optimize Drug Release andExtraction. AAPS PharmSciTech 2019, 20, 80. [Google Scholar] [CrossRef] [PubMed]
- Palekar, S.; Nukala, P.K.; Patel, K. Aversion liquid-filled drug releasing capsule (3D-RECAL): A novel technology for the development of immediate release abuse deterrent formulations using a fused deposition modelling (FDM) 3D printer. Int. J. Pharm. 2022, 621, 121804. [Google Scholar] [CrossRef] [PubMed]
- Dumpa, N.; Butreddy, A.; Wang, H.; Komanduri, N.; Bandari, S.; Repka, M.A. 3D printing in personalized drug delivery: An overview of hot-melt extrusion-based fused deposition modeling. Int. J. Pharm. 2021, 600, 120501. [Google Scholar] [CrossRef] [PubMed]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.Q.; Hui, D. Additive manufacturing (3D printing): A review of materials, methods, applications and challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Pistone, M.; Racaniello, G.F.; Arduino, I.; Laquintana, V.; Lopalco, A.; Cutrignelli, A.; Rizzi, R.; Franco, M.; Lopedota, A.; Denora, N. Direct cyclodextrin-based powder extrusion 3D printing for one-step production of the BCS class II model drug niclosamide. Drug Deliv. Transl. Res. 2022, 12, 1895–1910. [Google Scholar] [CrossRef] [PubMed]
- Gueche, Y.A.; Sanchez-Ballester, N.M.; Cailleaux, S.; Bataille, B.; Soulairol, I. Selective Laser Sintering (SLS), a New Chapter in the Production of Solid Oral Forms (SOFs) by 3D Printing. Pharmaceutics 2021, 13, 1212. [Google Scholar] [CrossRef]
- Tetyczka, C.; Brisberger, K.; Reiser, M.; Zettl, M.; Jeitler, R.; Winter, C.; Kolb, D.; Leitinger, G.; Spoerk, M.; Roblegg, E. Itraconazole Nanocrystals on Hydrogel Contact Lenses via Inkjet Printing: Implications for Ophthalmic Drug Delivery. ACS Appl. Nano Mater. 2022, 5, 9435–9446. [Google Scholar] [CrossRef]
- Li, R.; Pan, Y.; Chen, D.; Xu, X.; Yan, G.; Fan, T. Design, Preparation and In Vitro Evaluation of Core–Shell Fused Deposition Modelling 3D-Printed Verapamil Hydrochloride Pulsatile Tablets. Pharmaceutics 2022, 14, 437. [Google Scholar] [CrossRef]
- Davis, D.A.; Thakkar, R.; Su, Y.; Williams, R.O.; Maniruzzaman, M. Selective Laser Sintering 3-Dimensional Printing as a Single Step Process to Prepare Amorphous Solid Dispersion Dosage Forms for Improved Solubility and Dissolution Rate. J. Pharm. Sci. 2021, 110, 1432–1443. [Google Scholar] [CrossRef]
- Charoo, N.A.; Barakh Ali, S.F.; Mohamed, E.M.; Kuttolamadom, M.A.; Ozkan, T.; Khan, M.A.; Rahman, Z. Selective laser sintering 3D printing—An overview of the technology and pharmaceutical applications. Drug Dev. Ind. Pharm. 2020, 46, 869–877. [Google Scholar] [CrossRef]
- Li, M.; Han, Y.; Zhou, M.; Chen, P.; Gao, H.; Zhang, Y.; Zhou, H. Experimental investigating and numerical simulations of the thermal behavior and process optimization for selective laser sintering of PA6. J. Manuf. Process. 2020, 56, 271–279. [Google Scholar] [CrossRef]
- Gayer, C.; Ritter, J.; Bullemer, M.; Grom, S.; Jauer, L.; Meiners, W.; Pfister, A.; Reinauer, F.; Vučak, M.; Wissenbach, K.; et al. Development of a solvent-free polylactide/calcium carbonate composite for selective laser sintering of bone tissue engineering scaffolds. Mater. Sci. Eng. C 2019, 101, 660–673. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Sharma, V.S.; Sachdeva, A. Application of response surface methodology to analyze the effect of selective laser sintering parameters on dimensional accuracy. Prog. Addit. Manuf. 2019, 4, 3–12. [Google Scholar] [CrossRef]
- Goodridge, R.D.; Tuck, C.J.; Hague, R.J.M. Laser sintering of polyamides and other polymers. Prog. Mater. Sci. 2012, 57, 229–267. [Google Scholar] [CrossRef]
- Lekurwale, S.; Karanwad, T.; Banerjee, S. Selective laser sintering (SLS) of 3D printlets using a 3D printer comprised of IR/red-diode laser. Ann. 3D Print. Med. 2022, 6, 100054. [Google Scholar] [CrossRef]
- Gueche, Y.A.; Sanchez-Ballester, N.M.; Bataille, B.; Aubert, A.; Rossi, J.-C.; Soulairol, I. A QbD Approach for Evaluating the Effect of Selective Laser Sintering Parameters on Printability and Properties of Solid Oral Forms. Pharmaceutics 2021, 13, 1701. [Google Scholar] [CrossRef]
- Akilesh, M.; Elango, P.R.; Devanand, A.A.; Soundararajan, R.; Varthanan, P.A. Optimization of Selective Laser Sintering Process Parameters on Surface Quality. In 3D Printing and Additive Manufacturing Technologies; Kumar, L.J., Pandey, P.M., Wimpenny, D.I., Eds.; Springer: Singapore, 2019; pp. 141–157. [Google Scholar]
- Crump, S.S. Fast, precise, safe prototypes with FDM. ASME PED 1991, 50, 53–60. [Google Scholar]
- Vithani, K.; Goyanes, A.; Jannin, V.; Basit, A.W.; Gaisford, S.; Boyd, B.J. An Overview of 3D Printing Technologies for Soft Materials and Potential Opportunities for Lipid-based Drug Delivery Systems. Pharm. Res. 2018, 36, 4. [Google Scholar] [CrossRef] [Green Version]
- Goyanes, A.; Det-Amornrat, U.; Wang, J.; Basit, A.W.; Gaisford, S. 3D scanning and 3D printing as innovative technologies for fabricating personalized topical drug delivery systems. J. Control. Release 2016, 234, 41–48. [Google Scholar] [CrossRef]
- Goyanes, A.; Fina, F.; Martorana, A.; Sedough, D.; Gaisford, S.; Basit, A.W. Development of modified release 3D printed tablets (printlets) with pharmaceutical excipients using additive manufacturing. Int. J. Pharm. 2017, 527, 21–30. [Google Scholar] [CrossRef]
- Mohamed, O.A.; Masood, S.H.; Bhowmik, J.L. Optimization of fused deposition modeling process parameters: A review of current research and future prospects. Adv. Manuf. 2015, 3, 42–53. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Jaisingh Sheoran, A.; Kumar, H. Fused Deposition modeling process parameters optimization and effect on mechanical properties and part quality: Review and reflection on present research. Mater. Today Proc. 2020, 21, 1659–1672. [Google Scholar] [CrossRef]
- Kissi, E.O.; Nilsson, R.; Nogueira, L.P.; Larsson, A.; Tho, I. Influence of Drug Load on the Printability and Solid-State Properties of 3D-Printed Naproxen-Based Amorphous Solid Dispersion. Molecules 2021, 26, 4492. [Google Scholar] [CrossRef]
- Fanous, M.; Bitar, M.; Gold, S.; Sobczuk, A.; Hirsch, S.; Ogorka, J.; Imanidis, G. Development of immediate release 3D-printed dosage forms for a poorly water-soluble drug by fused deposition modeling: Study of morphology, solid state and dissolution. Int. J. Pharm. 2021, 599, 120417. [Google Scholar] [CrossRef]
- Fuenmayor, E.; Forde, M.; Healy, A.V.; Devine, D.M.; Lyons, J.G.; McConville, C.; Major, I. Material Considerations for Fused-Filament Fabrication of Solid Dosage Forms. Pharmaceutics 2018, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Goyanes, A.; Allahham, N.; Trenfield, S.J.; Stoyanov, E.; Gaisford, S.; Basit, A.W. Direct powder extrusion 3D printing: Fabrication of drug products using a novel single-step process. Int. J. Pharm. 2019, 567, 118471. [Google Scholar] [CrossRef]
- Yu, D.-G.; Li, J.-J.; Williams, G.R.; Zhao, M. Electrospun amorphous solid dispersions of poorly water-soluble drugs: A review. J. Control. Release 2018, 292, 91–110. [Google Scholar] [CrossRef] [Green Version]
- Modica de Mohac, L.; Keating, A.V.; De Fátima Pina, M.; Raimi-Abraham, B.T. Engineering of Nanofibrous Amorphous and Crystalline Solid Dispersions for Oral Drug Delivery. Pharmaceutics 2019, 11, 7. [Google Scholar] [CrossRef] [Green Version]
- Bai, Y.; Wang, D.; Zhang, Z.; Pan, J.; Cui, Z.; Yu, D.-G.; Annie Bligh, S.-W. Testing of fast dissolution of ibuprofen from its electrospun hydrophilic polymer nanocomposites. Polym. Test. 2021, 93, 106872. [Google Scholar] [CrossRef]
- Uhljar, L.É.; Kan, S.Y.; Radacsi, N.; Koutsos, V.; Szabó-Révész, P.; Ambrus, R. In Vitro Drug Release, Permeability, and Structural Test of Ciprofloxacin-Loaded Nanofibers. Pharmaceutics 2021, 13, 556. [Google Scholar] [CrossRef] [PubMed]
- Vass, P.; Szabó, E.; Domokos, A.; Hirsch, E.; Galata, D.; Farkas, B.; Démuth, B.; Andersen, S.K.; Vigh, T.; Verreck, G.; et al. Scale-up of electrospinning technology: Applications in the pharmaceutical industry. WIREs Nanomed. Nanobiotechnol. 2020, 12, e1611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verreck, G.; Chun, I.; Peeters, J.; Rosenblatt, J.; Brewster, M.E. Preparation and Characterization of Nanofibers Containing Amorphous Drug Dispersions Generated by Electrostatic Spinning. Pharm. Res. 2003, 20, 810–817. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Z.K.; Balogh, A.; Vajna, B.; Farkas, A.; Patyi, G.; Kramarics, Á.; Marosi, G. Comparison of Electrospun and Extruded Soluplus®-Based Solid Dosage Forms of Improved Dissolution. J. Pharm. Sci. 2012, 101, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Höhne, G.W.H.; Hemminger, W.F.; Flammersheim, H.J. Theoretical Fundamentals of Differential Scanning Calorimeters. In Differential Scanning Calorimetry; Höhne, G.W.H., Hemminger, W.F., Flammersheim, H.J., Eds.; Springer: Berlin/Heidelberg, Germany, 2003; pp. 31–63. [Google Scholar]
- Tafu, N.N.; Jideani, V.A. Characterization of Novel Solid Dispersions of Moringa oleifera Leaf Powder Using Thermo-Analytical Techniques. Processes 2021, 9, 2230. [Google Scholar] [CrossRef]
- Raina, S.A.; Alonzo, D.E.; Zhang, G.G.Z.; Gao, Y.; Taylor, L.S. Impact of Polymers on the Crystallization and Phase Transition Kinetics of Amorphous Nifedipine during Dissolution in Aqueous Media. Mol. Pharm. 2014, 11, 3565–3576. [Google Scholar] [CrossRef]
- Moseson, D.E.; Taylor, L.S. The application of temperature-composition phase diagrams for hot melt extrusion processing of amorphous solid dispersions to prevent residual crystallinity. Int. J. Pharm. 2018, 553, 454–466. [Google Scholar] [CrossRef]
- De Araujo, G.L.B.; Benmore, C.J.; Byrn, S.R. Local Structure of Ion Pair Interaction in Lapatinib Amorphous Dispersions characterized by Synchrotron X-Ray diffraction and Pair Distribution Function Analysis. Sci. Rep. 2017, 7, 46367. [Google Scholar] [CrossRef] [Green Version]
- Tian, B.; Tang, X.; Taylor, L.S. Investigating the Correlation between Miscibility and Physical Stability of Amorphous Solid Dispersions Using Fluorescence-Based Techniques. Mol. Pharm. 2016, 13, 3988–4000. [Google Scholar] [CrossRef]
- Saboo, S.; Mugheirbi, N.A.; Zemlyanov, D.Y.; Kestur, U.S.; Taylor, L.S. Congruent release of drug and polymer: A “sweet spot” in the dissolution of amorphous solid dispersions. J. Control. Release 2019, 298, 68–82. [Google Scholar] [CrossRef]
- Que, C.; Gao, Y.; Raina, S.A.; Zhang, G.G.Z.; Taylor, L.S. Paclitaxel Crystal Seeds with Different Intrinsic Properties and Their Impact on Dissolution of Paclitaxel-HPMCAS Amorphous Solid Dispersions. Cryst. Growth Des. 2018, 18, 1548–1559. [Google Scholar] [CrossRef]
- Lauer, M.E.; Siam, M.; Tardio, J.; Page, S.; Kindt, J.H.; Grassmann, O. Rapid Assessment of Homogeneity and Stability of Amorphous Solid Dispersions by Atomic Force Microscopy—From Bench to Batch. Pharm. Res. 2013, 30, 2010–2022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borde, S.; Hegde, P.; Prathipati, P.; North, J.; Kumari, D.; Chauhan, H. Formulation and characterization of ternary amorphous solid dispersions of a highly potent anti-tubercular agent and curcumin. J. Drug. Deliv. Sci. Technol. 2021, 64, 102564. [Google Scholar] [CrossRef]
- Müller, M.; Platten, F.; Dulle, M.; Fischer, B.; Hoheisel, W.; Serno, P.; Egelhaaf, S.; Breitkreutz, J. Precipitation from amorphous solid dispersions in biorelevant dissolution testing: The polymorphism of regorafenib. Int. J. Pharm. 2021, 603, 120716. [Google Scholar] [CrossRef]
- Solomon, S.; Iqbal, J.; Albadarin, A.B. Insights into the ameliorating ability of mesoporous silica in modulating drug release in ternary amorphous solid dispersion prepared by hot melt extrusion. Eur. J. Pharm. Biopharm. 2021, 165, 244–258. [Google Scholar] [CrossRef]
- Zhang, Q.; Durig, T.; Blass, B.; Fassihi, R. Development of an amorphous based sustained release system for apremilast a selective phosphodiesterase 4 (PDE4) inhibitor. Int. J. Pharm. 2022, 615, 121516. [Google Scholar] [CrossRef]
- Yu, D.; Li, J.; Wang, H.; Pan, H.; Li, T.; Bu, T.; Zhou, W.; Zhang, X. Role of polymers in the physical and chemical stability of amorphous solid dispersion: A case study of carbamazepine. Eur. J. Pharm. Sci. 2022, 169, 106086. [Google Scholar] [CrossRef]
- Bhanderi, A.; Bari, F.; Al-Obaidi, H. Evaluation of the impact of surfactants on miscibility of griseofulvin in spray dried amorphous solid dispersions. J. Drug. Deliv. Sci. Technol. 2021, 64, 102606. [Google Scholar] [CrossRef]
- Bhujbal, S.V.; Pathak, V.; Zemlyanov, D.Y.; Taylor, L.S.; Zhou, Q. Physical Stability and Dissolution of Lumefantrine Amorphous Solid Dispersions Produced by Spray Anti-Solvent Precipitation. J. Pharm. Sci. 2021, 110, 2423–2431. [Google Scholar] [CrossRef]
- Moritani, T.; Kaneko, Y.; Morinaga, T.; Ohtake, H.; Seto, Y.; Sato, H.; Onoue, S. Tranilast-loaded amorphous solid dispersion prepared with fine droplet drying process for improvement of oral absorption and anti-inflammatory effects on chemically-induced colitis. J. Drug. Deliv. Sci. Technol. 2021, 64, 102544. [Google Scholar] [CrossRef]
- Zhao, M.; You, D.; Yin, J.; Sun, W.; Yin, T.; Gou, J.; Zhang, Y.; Wang, Y.; He, H.; Tang, X. Quaternary enteric solid dispersion prepared by hot-melt extrusion to mask the bitter taste and enhance drug stability. Int. J. Pharm. 2021, 597, 120279. [Google Scholar] [CrossRef] [PubMed]
- Jarrells, T.W.; Munson, E.J. Comparison of Differential Scanning Calorimetry, Powder X-ray Diffraction, and Solid-state Nuclear Magnetic Resonance Spectroscopy for Measuring Crystallinity in Amorphous Solid Dispersions—Application to Drug-in-polymer Solubility. J. Pharm. Sci. 2022, 111, 2765–2778. [Google Scholar] [CrossRef] [PubMed]
- Paisana, M.C.; Lino, P.R.; Nunes, P.D.; Pinto, J.F.; Henriques, J.; Paiva, A.M. Laser diffraction as a powerful tool for amorphous solid dispersion screening and dissolution understanding. Eur. J. Pharm. Sci. 2021, 163, 105853. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, P.U.; Cooke, D.G.; Koch, M. Terahertz spectroscopy and imaging—Modern techniques and applications [Laser Photon. Rev. 5, No. 124–166]. Laser Photonics Rev. 2012, 6, 418. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Feng, X.; Williams, R.O.; Zhang, F. Characterization of amorphous solid dispersions. J. Pharm. Investig. 2018, 48, 19–41. [Google Scholar] [CrossRef]
- Sibik, J.; Löbmann, K.; Rades, T.; Zeitler, J.A. Predicting Crystallization of Amorphous Drugs with Terahertz Spectroscopy. Mol. Pharm. 2015, 12, 3062–3068. [Google Scholar] [CrossRef]
- Zeitler, J.A.; Taday, P.F.; Pepper, M.; Rades, T. Relaxation and Crystallization of Amorphous Carbamazepine Studied by Terahertz Pulsed Spectroscopy. J. Pharm. Sci. 2007, 96, 2703–2709. [Google Scholar] [CrossRef]
- Sibik, J.; Zeitler, J.A. Direct measurement of molecular mobility and crystallisation of amorphous pharmaceuticals using terahertz spectroscopy. Adv. Drug Deliv. Rev. 2016, 100, 147–157. [Google Scholar] [CrossRef] [Green Version]
- Davis, D.A.; Miller, D.A.; Santitewagun, S.; Zeitler, J.A.; Su, Y.; Williams, R.O. Formulating a heat- and shear-labile drug in an amorphous solid dispersion: Balancing drug degradation and crystallinity. Int. J. Pharm. X 2021, 3, 100092. [Google Scholar] [CrossRef]
- Deshmukh, K.; Sankaran, S.; Ahamed, B.; Sadasivuni, K.K.; Pasha, K.S.K.; Ponnamma, D.; Rama Sreekanth, P.S.; Chidambaram, K. Chapter 10—Dielectric Spectroscopy. In Spectroscopic Methods for Nanomaterials Characterization; Thomas, S., Thomas, R., Zachariah, A.K., Mishra, R.K., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 237–299. [Google Scholar]
- Pacult, J.; Rams-Baron, M.; Chmiel, K.; Jurkiewicz, K.; Antosik, A.; Szafraniec, J.; Kurek, M.; Jachowicz, R.; Paluch, M. How can we improve the physical stability of co-amorphous system containing flutamide and bicalutamide? The case of ternary amorphous solid dispersions. Eur. J. Pharm. Sci. 2019, 136, 104947. [Google Scholar] [CrossRef]
- Sahoo, A.; Kumar, N.S.K.; Suryanarayanan, R. Crosslinking: An avenue to develop stable amorphous solid dispersion with high drug loading and tailored physical stability. J. Control. Release 2019, 311–312, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Withers, P.J.; Bouman, C.; Carmignato, S.; Cnudde, V.; Grimaldi, D.; Hagen, C.K.; Maire, E.; Manley, M.; Du Plessis, A.; Stock, S.R. X-ray computed tomography. Nat. Rev. Methods Primers 2021, 1, 18. [Google Scholar] [CrossRef]
- Gamble, J.F.; Terada, M.; Holzner, C.; Lavery, L.; Nicholson, S.J.; Timmins, P.; Tobyn, M. Application of X-ray microtomography for the characterisation of hollow polymer-stabilised spray dried amorphous dispersion particles. Int. J. Pharm. 2016, 510, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Alhijjaj, M.; Yassin, S.; Reading, M.; Zeitler, J.A.; Belton, P.; Qi, S. Characterization of Heterogeneity and Spatial Distribution of Phases in Complex Solid Dispersions by Thermal Analysis by Structural Characterization and X-ray Micro Computed Tomography. Pharm. Res. 2017, 34, 971–989. [Google Scholar] [CrossRef] [Green Version]
- Qian, F.; Huang, J.; Hussain, M.A. Drug–Polymer Solubility and Miscibility: Stability Consideration and Practical Challenges in Amorphous Solid Dispersion Development. J. Pharm. Sci. 2010, 99, 2941–2947. [Google Scholar] [CrossRef]
- Lu, J.; Cuellar, K.; Hammer, N.I.; Jo, S.; Gryczke, A.; Kolter, K.; Langley, N.; Repka, M.A. Solid-state characterization of Felodipine–Soluplus amorphous solid dispersions. Drug Dev. Ind. Pharm. 2016, 42, 485–496. [Google Scholar] [CrossRef]
- Han, R.; Xiong, H.; Ye, Z.; Yang, Y.; Huang, T.; Jing, Q.; Lu, J.; Pan, H.; Ren, F.; Ouyang, D. Predicting physical stability of solid dispersions by machine learning techniques. J. Control. Release 2019, 311–312, 16–25. [Google Scholar] [CrossRef]
- Mali, S.N.; Tambe, S.; Pratap, A.P.; Cruz, J.N. Molecular Modeling Approaches to Investigate Essential Oils (Volatile Compounds) Interacting with Molecular Targets. In Essential Oils: Applications and Trends in Food Science and Technology; Santana de Oliveira, M., Ed.; Springer International Publishing: Cham, Switzerland, 2022; pp. 417–442. [Google Scholar]
- Walden, D.M.; Bundey, Y.; Jagarapu, A.; Antontsev, V.; Chakravarty, K.; Varshney, J. Molecular Simulation and Statistical Learning Methods toward Predicting Drug–Polymer Amorphous Solid Dispersion Miscibility, Stability, and Formulation Design. Molecules 2021, 26, 182. [Google Scholar] [CrossRef]
- Lee, H.; Kim, J.; Kim, S.; Yoo, J.; Choi, G.J.; Jeong, Y.-S. Deep Learning-Based Prediction of Physical Stability considering Class Imbalance for Amorphous Solid Dispersions. J. Chem. 2022, 2022, 4148443. [Google Scholar] [CrossRef]








| Trade Name | Chemical Name | BCS Class | Manufacturing Technique | Polymers Used | Company | Year of Approval |
|---|---|---|---|---|---|---|
| Cesamet® | Nabilone | II | Solvent evaporation | Povidone | Meda Pharmaceuticals | 1985 |
| Isoptin SR | Verapamil HCl | II | Melt extrusion | Hypromellose | Ranbaxy Laboratories | 1987 |
| Sporanox | Itraconazole | II | Fluid bed bead layering | Hypromellose, Polyethylene glycol | Janssen | 1992 |
| Prograf | Tacrolimus | II | Spray drying | Hypromellose, | Astellas Pharma | 1994 |
| NuvaRing | Etonogestrel/Ethinyl Estradiol | II | Melt extrusion | Ethylene vinylacetate copolymer | Merck | 2001 |
| Kaletra | Lopinavir/Ritonavir | IV/IV | Melt extrusion | Co-povidone, | AbbVie | 2007 |
| Intelence | Etravirine | IV | Spray drying | Hypromellose | Janssen | 2008 |
| Modigraf | Tacrolimus | II | Spray drying | Hypromellose | Astellas Pharma | 2009 |
| Zortress | Everolimus | III | Spray drying | Hypromellose | Novartis | 2010 |
| Norvir Tablet | Ritonavir | IV | Melt extrusion | Co-povidone | AbbVie | 2010 |
| Onmel | Itraconazole | II | Melt extrusion | Hypromellose | Merz Pharma | 2010 |
| Incivek | Telaprevir | II | Spray drying | Hypromellose acetate succinate | Vertex | 2011 |
| Zelboraf | Vemurafenib | IV | Solvent/anti-solvent precipitation | Hypromellose | Roche | 2011 |
| Kalydeco | Ivacaftor | II | Spray drying | Hypromellose acetate succinate | Vertex | 2012 |
| Noxafil | Posaconazole | II | Melt extrusion | Hypromellose acetate succinate | Merck | 2013 |
| Harvoni | Ledipasvir/Sofosbuvir | II/III | Spray drying | Co-povidone | Gilead Sciences | 2014 |
| ViekiraXR™ | Dasabuvir/Ombitasvir/Paritaprevir/Ritonavir | II/IV/IV/IV | Melt extrusion | Co-povidone | AbbVie | 2014 |
| Epclusa | Sofosbuvir/Velpatasvir | III/IV | Spray drying | Co-povidone | Gilead Sciences | 2016 |
| Orkambi | Lumacaftor/Ivacaftor | II/II | Spray drying | Hypromellose acetate succinate, Povidone | Vertex | 2016 |
| Venclexta | Venetoclax | IV | Melt extrusion | Co-povidone | AbbVie | 2016 |
| Zepatier | Elbasvir/Grazoprevir | II/II | Spray drying | Vitamin E polyethylene glycol succinate, Co-povidone, Hypromellose | Merck | 2016 |
| Stivarga | Regorafenib | II | Solvent Evaporation | Povidone | Bayer | 2017 |
| Mavyret™ | Glecaprevir/Pibrentasvir | IV/IV | Melt extrusion | Hypromellose, Co-povidone | AbbVie | 2017 |
| Lynparza | Olaparib | IV | Melt extrusion | Co-povidone | AstraZeneca | 2018 |
| Erleada | Apalutamide | II | Spray drying | Hypromellose acetate succinate | Janssen | 2018 |
| Trikafta | Elexacaftor (Crystalline)/Ivacaftor/Tezacaftor | II or IV | Spray drying | Hypromellose, Hypromellose acetate succinate | Vertex | 2019 |
| Symdeko | Tezacaftor/Ivacaftor and Ivacaftor | II/II or IV | Spray drying | Hypromellose, Hypromellose acetate succinate | Vertex | 2019 |
| Braftovi | Encorafenib | II | Melt extrusion | Co-povidone, Poloxamer 188 | Pfizer | 2020 |
| Oriahnn™ | Elagolix/estradiol/norethindrone acetate | III/II/NA | Melt extrusion | Co-povidone, Hypromellose | AbbVie | 2020 |
| Technique | Key Characteristics | Advantages | Limitations | Applications | Ref |
|---|---|---|---|---|---|
| Differential Scanning Calorimetry | Determination of melting point, glass transition temperature, heat capacity, drug and polymer interactions, determine the degree of crystallinity, and drug crystallization tendency; identify crystalline and amorphous state and molecular mobility. | Suitable for measuring melting; small sample size; easy experimental conditions; cost-effective and quick | Destructive, heat capacity measurement is less sensitive, no knowledge of the nature of the thermal events, and simultaneous thermal events that overlap cannot be resolved. | Solomon et al. utilized DSC in order to estimate the distribution of Felodipine in ternary amorphous dispersions containing Soluplus® and silica. They computed theoretical Tg of binary Felodipine-soluplus® combinations using the Gordon–Taylor equation in their research and compared them to Tg obtained empirically. They concluded that DSC results in a negative deviation in Tg, confirming stronger hydrogen bonding interactions between drug and polymer. | [145] |
| Modulated Differential Scanning Calorimetry | To assess the crystallization tendency of active ingredients, glass transition temperature, knowledge about miscibility with polymers, studying degree and level of crystallinity, crystal growth rate, and molecular mobility (e.g., structural relaxation, viscosity) | Separation of overlapping and complex thermal events, improved sensitivity in heat capacity measurement in comparison to conventional DSC. | Requirement of well-planned experiments, experimentation is very conditional dependent, Melting: challenging interpretation, unreliable mDSC measurement | Zhang et al. performed in silico screening first and further various prototype formulations of apremilast ASDs via spray drying were developed. In this study, the author utilized mDSC to study the miscibility of the drug with polymer, measure Tg, and evaluate the stability of ASDs under stress conditions. It was observed via mDSC analysis that immiscible systems exhibit instability after being stored under stressful conditions and showed multiple Tg in comparison to single Tg obtained from stable ASDs. | [146] |
| Thermogravimetric analysis | Thermal stability, study evaporation profile of feed solution in spray-drying, chemical identification of volatile compounds released from samples | Limited sample size, little sample preparation required, simple to use | Destructive, unable to determine the chemical composition | Yu et al. studied the role of neutral and acidic polymers in the physical and chemical stability of the developed ASDs of carbamazepine. The DSC and TGA analysis revealed that the prepared ASDs are physically stable owing to the formation of strong intermolecular bonds; however, acidic polymers provide an acidic microenvironment, making the developed ASDs susceptible to chemical degradation. | [147] |
| Fourier Transformation Infrared technique (FTIR) | Molecular interactions between drug and polymer, polymorph characterization, phase separation, crystalline and amorphous identification | Quantitative analysis, small sample requirement, non-destructive | Moisture present and less precise findings | Bhanderi et al. confirmed the development of ASDs of griseofulvin and hypromellose acetate succinate along with surfactant employing FTIR. Authors concluded that the peak positions and broadening in the developed ASDs were unaffected by the surfactant presence, indicating that the polarity around the aforementioned groups was unaffected. | [148] |
| Powder X-ray diffraction | Polymorphs screening, detects crystallinity degree, amorphous detection, and drug–polymer miscibility, studies recrystallization behavior, the microstructure of ASDs | The sample size required is small, analysis is simple, qualitative and quantitative, non-destructive | Relatively less sensitive (>5% crystallinity) than DSC, TEM and PLM, details on the chemical structure is provided, which can otherwise be obtained from nuclear mass resonance spectroscopy, infrared spectroscopy and mass spectrometry. | Bhujbal et al. studied Lumefantrine ASDs physical stability and dissolution profile and observed that (a) polymer and (b) drug-to-polymer ratio had a significant effect. Eudragit L 100 showed a crystalline drug peak even at lower drug concentration in PXRD analysis whereas HPMC Phthalate and HPMC AS showed better physical stability and miscibility with the drug. | [149] |
| Polarized Light Microscopy | Polymorphic transition, detect crystallinity (birefringence) and amorphous, crystal shape and size, crystallization route | Non-destructive, simple to use, smaller sample size, reproducible | It is not appropriate for agglomerates, semi-quantitative, and sample recovery is quite laborious. | Moritani et al. prepared tranilast-loaded ASDs for the treatment of inflammatory bowel disorders. There was no discernible birefringence in the PLM picture of ASDs/tranilast, whereas crystalline drug showed considerable birefringence. This result was also in agreement with DSC. | [150] |
| Atomic force microscopy | Visualises molecular mobility, mixture-specific separation rates, drug–polymer miscibility, and bulk and surface dynamics. These variables have a fundamental and integral role in predicting the long-term stability of an ASD. | High resolution up to 1 nm Small sample size, Detect repeated lattice | Expensive, Lengthy scan duration that may cause sample thermal drift, sample preparation is necessary | Zhao et al. developed quaternary enteric ASDs of erythromycin utilizing HME. Raman and AFM have taken advantage of the fact that the bulk of the drug dispersed in the PVP/VA64 matrix (co-povidone), and that the nanometre-sized drug–polymer system confined within the enteric continuous phase to form a solid emulsion-like structure. | [151] |
| Scanning electron microscopy | Analyze particle size, morphology, and surface characteristics of formulation, identifies present of drug crystal, chemical distribution map | Low sample size and high resolution | Necessitates sample preparation (coating and vacuum setting), costly equipment, huge device, and requires housing in a location free from any potential electric, magnetic, or vibration interference | Spray-drying was carried out to prepare ASD formulations of GDC-0334 in PVP/VA 64 (co-povidone) at different drug loadings (20, 30, 40, and 60 percent, w/w), with or without 5% w/w surfactants (Tween 80, SLS, or Vit-E TPGS 1000) by Yen and his coworkers. All four ASD formulations with 5% w/w Tween 80 as constant and varied drug-loading (20–60% w/w) displayed a collapsed spherical shape made up of small, dense particles with sizes between 2 and 3 µm. | [93] |
| Solid-state nuclear magnetic resonance (SSNMR) | Detect crystallinity degree, amorphous identification, drug and polymer interaction, drug and polymer miscibility, molecular mobility | Limited sample size, qualitative and quantitative, easy to prepare the sample, non-destructive | Possibility of recrystallization during analysis, relatively expensive, quantification challenges caused by chemical noise and signal overlaps, longer analysis time | Jarrells et al. measured and compared ASDs crystallinity using the SSNMR technique for nifedipine and polyvinylpyrrolidone drug–polymer system. Authors successfully were able to distinguish residual crystals and crystals formed during storage via SSNMR. | [152] |
| Raman Spectroscopy | Can be applied to study the dissolution behavior in aqueous conditions, and gives information about drug–drug and drug–polymer interaction, drug–polymer miscibility, and phase separation. | Quantitative detection, small sample size, unaffected by water, ability to penetrate glass containers | Sample heating with powerful laser radiation can harm the sample, sample fluorescence and photodegradation, requires sensitive and highly specialised instruments for detection. | Paisana et al. formulated ASDs of itraconazole employing HPMC-acetate succinate medium grade (HPMC-AS M). Author evaluated ASDs suspended in FaSSIF media after 240 min, Raman examination of API: HPMC-AS M (35:65) particles confirmed a faster polymer dissolution rate and associated surface API enrichment. | [153] |
| Transmission electron microscopy | To detect crystalline substances in ASDs, can generate both real-space pictures and electron diffraction patterns. | Smaller sample quantity, quantitative, high spatial resolution imaging, ability to detect crystallinity degree | Certain samples may be damaged by electron beams; tedious sample preparation | Sari et al. prepared ASD of felodipine and polyvinylpyrrolidone/vinyl acetate copolymer (co-povidone) employing the HME technique. PXRD, DSC, and FTIR revealed no evidence of residual crystallinity. However, of the 55 investigated particles, two places with crystals at the edges of milled particles were found using TEM. | [37] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tambe, S.; Jain, D.; Meruva, S.K.; Rongala, G.; Juluri, A.; Nihalani, G.; Mamidi, H.K.; Nukala, P.K.; Bolla, P.K. Recent Advances in Amorphous Solid Dispersions: Preformulation, Formulation Strategies, Technological Advancements and Characterization. Pharmaceutics 2022, 14, 2203. https://doi.org/10.3390/pharmaceutics14102203
Tambe S, Jain D, Meruva SK, Rongala G, Juluri A, Nihalani G, Mamidi HK, Nukala PK, Bolla PK. Recent Advances in Amorphous Solid Dispersions: Preformulation, Formulation Strategies, Technological Advancements and Characterization. Pharmaceutics. 2022; 14(10):2203. https://doi.org/10.3390/pharmaceutics14102203
Chicago/Turabian StyleTambe, Srushti, Divya Jain, Sai Kishore Meruva, Gopinath Rongala, Abhishek Juluri, Girish Nihalani, Hemanth Kumar Mamidi, Pavan Kumar Nukala, and Pradeep Kumar Bolla. 2022. "Recent Advances in Amorphous Solid Dispersions: Preformulation, Formulation Strategies, Technological Advancements and Characterization" Pharmaceutics 14, no. 10: 2203. https://doi.org/10.3390/pharmaceutics14102203