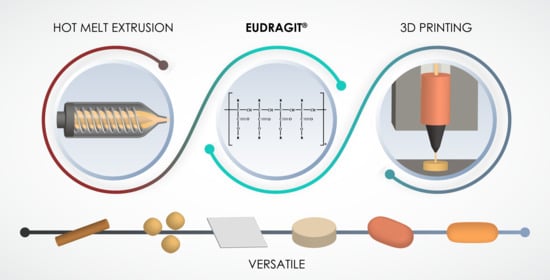
Eudragit®: A Versatile Family of Polymers for Hot Melt Extrusion and 3D Printing Processes in Pharmaceutics
Abstract
:1. Introduction
2. Current Scenario
3. Hot Melt Extrusion
3.1. Solid Dispersions (SDs)
3.2. Tablets
3.3. Other Dosage Forms Obtained by HME
4. 3D Printing
4.1. Fused Deposition Modeling
4.2. Other Techniques
5. Quality Assessment of Dosage Forms Produced by HME and 3D Printing
6. Final Remarks and Challenges
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Wang, H.; Dumpa, N.; Bandari, S.; Durig, T.; Repka, M.A. Fabrication of Taste-Masked Donut-Shaped Tablets Via Fused Filament Fabrication 3D Printing Paired with Hot-Melt Extrusion Techniques. AAPS PharmSciTech 2020, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dumpa, N.; Butreddy, A.; Wang, H.; Komanduri, N.; Bandari, S.; Repka, M.A. 3D printing in personalized drug delivery: An overview of hot-melt extrusion-based fused deposition modeling. Int. J. Pharm. 2021, 600, 120501. [Google Scholar] [CrossRef] [PubMed]
- Bandari, S.; Nyavanandi, D.; Dumpa, N.; Repka, M.A. Coupling Hot Melt Extrusion and Fused Deposition Modeling: Critical Properties for Successful Performance. Adv. Drug Deliv. Rev. 2021, 172, 52–63. [Google Scholar] [CrossRef]
- Tran, P.H.L.; Lee, B.J.; Tran, T.T.D. Recent studies on the processes and formulation impacts in the development of solid dispersions by hot-melt extrusion. Eur. J. Pharm. Biopharm. 2021, 164, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Tambe, S.; Jain, D.; Agarwal, Y.; Amin, P. Hot-melt extrusion: Highlighting recent advances in pharmaceutical applications. J. Drug Deliv. Sci. Technol. 2021, 63, 102452. [Google Scholar] [CrossRef]
- Cantin, O.; Siepmann, F.; Willart, J.F.; Danede, F.; Siepmann, J.; Karrout, Y. PEO hot melt extrudates for controlled drug delivery: Importance of the type of drug and loading. J. Drug Deliv. Sci. Technol. 2021, 61, 102238. [Google Scholar] [CrossRef]
- Patki, M.; Palekar, S.; Nukala, P.K.; Vartak, R.; Patel, K. Overdose and Alcohol Sensitive Immediate Release System (OASIS) for Deterring Accidental Overdose or Abuse of Drugs. AAPS PharmSciTech 2021, 22, 1–12. [Google Scholar] [CrossRef]
- Emam, M.F.; Taha, N.F.; Mursi, N.M.; Emara, L.H. Preparation, characterization and in-Vitro/in-Vivo evaluation of meloxicam extruded pellets with enhanced bioavailability and stability. Drug Dev. Ind. Pharm. 2021, 47, 163–175. [Google Scholar] [CrossRef]
- Dumpa, N.R.; Sarabu, S.; Bandari, S.; Zhang, F.; Repka, M.A. Chronotherapeutic Drug Delivery of Ketoprofen and Ibuprofen for Improved Treatment of Early Morning Stiffness in Arthritis Using Hot-Melt Extrusion Technology. AAPS PharmSciTech 2018, 19, 2700–2709. [Google Scholar] [CrossRef]
- Koutsamanis, I.; Spoerk, M.; Arbeiter, F.; Eder, S.; Roblegg, E. Development of porous polyurethane implants manufactured via hot-melt extrusion. Polymers 2020, 12, 2950. [Google Scholar] [CrossRef] [PubMed]
- Albarahmieh, E.; Qi, S.; Craig, D.Q.M. Hot melt extruded transdermal films based on amorphous solid dispersions in Eudragit RS PO: The inclusion of hydrophilic additives to develop moisture-activated release systems. Int. J. Pharm. 2016, 514, 270–281. [Google Scholar] [CrossRef]
- Marreto, R.N.; Cardoso, G.; dos Santos Souza, B.; Martin-Pastor, M.; Cunha-Filho, M.; Taveira, S.F.; Concheiro, A.; Alvarez-Lorenzo, C. Hot melt-extrusion improves the properties of cyclodextrin-based poly(pseudo)rotaxanes for transdermal formulation. Int. J. Pharm. 2020, 586, 119510. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.; Elshaer, A.; Sareh, P.; Elsayed, M.; Hassanin, H. Additive Manufacturing Technologies for Drug Delivery Applications. Int. J. Pharm. 2020, 580, 119245. [Google Scholar] [CrossRef] [PubMed]
- ISO/ASTM Standard Terminology for Additive Manufacturing Technologies—General Principles Terminoology; ASTM International: West Conshohocken, PA, USA, 2015.
- Dos Santos, J.; de Oliveira, R.S.; de Oliveira, T.V.; Velho, M.C.; Konrad, M.V.; da Silva, G.S.; Deon, M.; Beck, R.C.R. 3D Printing and Nanotechnology: A Multiscale Alliance in Personalized Medicine. Adv. Funct. Mater. 2021, 31, 2009691. [Google Scholar] [CrossRef]
- Brambilla, C.R.M.; Okafor-muo, O.L.; Hassanin, H.; Elshaer, A. 3DP printing of oral solid formulations: A systematic review. Pharmaceutics 2021, 13, 358. [Google Scholar] [CrossRef]
- Abaci, A.; Gedeon, C.; Kuna, A.; Guvendiren, M. Additive manufacturing of oral tablets: Technologies, materials and printed tablets. Pharmaceutics 2021, 13, 156. [Google Scholar] [CrossRef]
- Conceição, J.; Farto-vaamonde, X.; Goyanes, A.; Adeoye, O.; Concheiro, A.; Cabral-marques, H.; Manuel, J.; Lobo, S.; Alvarez-lorenzo, C. Hydroxypropyl- β -cyclodextrin-based fast dissolving carbamazepine printlets prepared by semisolid extrusion 3D printing. Carbohydr. Polym. 2019, 221, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Kobayashi, M.; Martínez-pacheco, R.; Gaisford, S.; Basit, A.W. Fused- filament 3D printing of drug products: Microstructure analysis and drug release characteristics of PVA-based caplets. Int. J. Pharm. 2016, 514, 290–295. [Google Scholar] [CrossRef]
- Hafezi, F.; Scoutaris, N.; Douroumis, D.; Boateng, J. 3D printed chitosan dressing crosslinked with genipin for potential healing of chronic wounds. Int. J. Pharm. 2019, 560, 406–415. [Google Scholar] [CrossRef]
- Elahpour, N.; Pahlevanzadeh, F.; Kharaziha, M.; Bakhsheshi-Rad, H.R.; Ramakrishna, S.; Berto, F. 3D printed microneedles for transdermal drug delivery: A brief review of two decades. Int. J. Pharm. 2021, 597, 120301. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, J.; Deon, M.; Silveira da Silva, G.; Carlos Ruver Beck, R. Multiple variable effects in the customisation of fused deposition modelling 3D-printed medicines: A design of experiments (DoE) approach. Int. J. Pharm. 2021, 597, 120331. [Google Scholar] [CrossRef]
- Holländer, J.; Genina, N.; Jukarainen, H.; Khajeheian, M.; Rosling, A.; Mäkilä, E.; Sandler, N. Three-Dimensional Printed PCL-Based Implantable Prototypes of Medical Devices for Controlled Drug Delivery. J. Pharm. Sci. 2016, 105, 2665–2676. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Zhao, S.; Zhu, M.; Zhu, Y.; Zhang, Y.; Liu, Z.; Zhang, C. 3D-printed magnetic Fe3O4/MBG/PCL composite scaffolds with multifunctionality of bone regeneration, local anticancer drug delivery and hyperthermia. J. Mater. Chem. B 2014, 2, 7583–7595. [Google Scholar] [CrossRef]
- Liu, F.; Li, W.; Liu, H.; Yuan, T.; Yang, Y.; Zhou, W.; Hu, Y.; Yang, Z. Preparation of 3D Printed Chitosan/Polyvinyl Alcohol Double Network Hydrogel Scaffolds. Macromol. Biosci. 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Thakral, S.; Thakral, N.K.; Majumdar, D.K. Eudragit®: A technology evaluation. Expert Opin. Drug Deliv. 2013, 10, 131–149. [Google Scholar] [CrossRef]
- Patra, C.N.; Priya, R.; Swain, S.; Kumar Jena, G.; Panigrahi, K.C.; Ghose, D. Pharmaceutical significance of Eudragit: A review. Futur. J. Pharm. Sci. 2017, 3, 33–45. [Google Scholar] [CrossRef]
- Rowe, R.C.; Sheskey, P.; Quinn, M.E. Handbook of Pharmaceutical Excipients, 6th ed.; Rowe, R.C., Sheskey, P., Quinn, M.E., Eds.; Pharmaceutical Press: London, UK, 2009. [Google Scholar]
- Claeys, B.; De Coen, R.; De Geest, B.G.; De La Rosa, V.R.; Hoogenboom, R.; Carleer, R.; Adriaensens, P.; Remon, J.P.; Vervaet, C. Structural modifications of polymethacrylates: Impact on thermal behavior and release characteristics of glassy solid solutions. Eur. J. Pharm. Biopharm. 2013, 85, 1206–1214. [Google Scholar] [CrossRef] [PubMed]
- Tipduangta, P.; Belton, P.; McAuley, W.J.; Qi, S. The use of polymer blends to improve stability and performance of electrospun solid dispersions: The role of miscibility and phase separation. Int. J. Pharm. 2021, 602, 120637. [Google Scholar] [CrossRef] [PubMed]
- Alyami, H.S.; Ibrahim, M.A.; Alyami, M.H.; Dahmash, E.Z.; Almeanazel, O.T.; Algahtani, T.S.; Alanazi, F.; Alshora, D.H. Formulation of sublingual promethazine hydrochloride tablets for rapid relief of motion sickness. Saudi Pharm. J. 2021, 29, 478–486. [Google Scholar] [CrossRef]
- Peralta, M.F.; Guzman, M.L.; Bracamonte, M.E.; Marco, J.D.; Olivera, M.E.; Carrer, D.C.; Barroso, P.A. Efficacy of topical risedronate and risedronate—Eudragit E complex in a model of cutaneous leishmaniasis induced by Leishmania (Leishmania) amazonensis. Heliyon 2021, 7, e07136. [Google Scholar] [CrossRef]
- Keating, A.V.; Soto, J.; Tuleu, C.; Forbes, C.; Zhao, M.; Craig, D.Q.M. Solid state characterisation and taste masking efficiency evaluation of polymer based extrudates of isoniazid for paediatric administration. Int. J. Pharm. 2018, 536, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.K.; Maniruzzaman, M.; Nokhodchi, A. Development and optimisation of novel polymeric compositions for sustained release theophylline caplets (PrintCap) via FDM 3D printing. Polymers 2020, 12, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bagde, A.; Patel, N.; Patel, K.; Nottingham, E.; Singh, M. Sustained release dosage form of noscapine HCl using hot melt extrusion (HME) technique: Formulation and pharmacokinetics. Drug Deliv. Transl. Res. 2021, 11, 1156–1165. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.; Chawla, A.; Sharma, P.; Pawar, P. Formulation and in vitro evaluation of Eudragit S-100 coated naproxen matrix tablets for colon-targeted drug delivery system. J. Adv. Pharm. Technol. Res. 2013, 4, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Saerens, L.; Dierickx, L.; Lenain, B.; Vervaet, C.; Remon, J.P.; Beer, T. De Raman spectroscopy for the in-line polymer-drug quantification and solid state characterization during a pharmaceutical hot-melt extrusion process. Eur. J. Pharm. Biopharm. 2011, 77, 158–163. [Google Scholar] [CrossRef] [Green Version]
- Park, J.B.; Lee, B.J.; Kang, C.Y.; Tiwari, R.V.; Repka, M.A. Process analytical quality control of tailored drug release formulation prepared via hot-melt extrusion technology. J. Drug Deliv. Sci. Technol. 2017, 38, 51–58. [Google Scholar] [CrossRef] [Green Version]
- Santos Ferreira, I.; Kikhney, J.; Kursawe, L.; Kasper, S.; Gonçalves, L.M.D.; Trampuz, A.; Moter, A.; Bettencourt, A.F.; Almeida, A.J. Encapsulation in Polymeric Microparticles Improves Daptomycin Activity Against Mature Staphylococci Biofilms—a Thermal and Imaging Study. AAPS PharmSciTech 2018, 19, 1625–1636. [Google Scholar] [CrossRef]
- Latha, S.; Selvamani, P.; Suganya, G.; Thimiri Govinda Raj, D.B.; Pal, T.K. Preparation and In-vitro Evaluation of Pantoprazole Sodium Magnetic Microspheres by Emulsion Solvent Evaporation Method. Bionanoscience 2021, 11, 643–647. [Google Scholar] [CrossRef]
- Ali, R. Preparation and characterization of dexamethasone polymeric nanoparticle by membrane emulsification method. J. Nanoparticle Res. 2020, 22, 1–9. [Google Scholar] [CrossRef]
- Beber, T.C.; de Andrade, D.F.; dos Santos Chaves, P.; Pohlmann, A.R.; Guterres, S.S.; Ruver Beck, R.C. Cationic Polymeric Nanocapsules as a Strategy to Target Dexamethasone to Viable Epidermis: Skin Penetration and Permeation Studies. J. Nanosci. Nanotechnol. 2016, 16, 1331–1338. [Google Scholar] [CrossRef]
- Fontana, M.C.; Beckenkamp, A.; Buffon, A.; Beck, R.C.R. Controlled release of raloxifene by nanoencapsulation: Effect on in vitro antiproliferative activity of human breast cancer cells. Int. J. Nanomed. 2014, 9, 2979–2991. [Google Scholar] [CrossRef] [Green Version]
- Chaves, P.S.; Dos Santos, J.; Pohlmann, A.R.; Guterres, S.S.; Beck, R.C.R.; Dos Santos, J.; Pohlmann, A.R.; Guterres, S.S. Sublingual tablets containing spray-dried carvedilol-loaded nanocapsules: Development of an innovative nanomedicine. Pharm. Dev. Technol. 2020, 25, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- Rongthong, T.; Sungthongjeen, S.; Siepmann, F.; Siepmann, J.; Pongjanyakul, T. Eudragit RL-based film coatings: How to minimize sticking and adjust drug release using MAS. Eur. J. Pharm. Biopharm. 2020, 148, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.B.; Shah, J.; Jacob, S.; Al-Dhubiab, B.E.; Patel, V.; Sreeharsha, N.; Shinu, P. Development of mucoadhesive buccal film for rizatriptan: In vitro and in vivo evaluation. Pharmaceutics 2021, 13, 728. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.S.; Meena, A.; Parikh, T.; Serajuddin, A.T.M. Investigation of thermal and viscoelastic properties of polymers relevant to hot melt extrusion—I: Polyvinylpyrrolidone and related polymers. J. Excip. Food Chem. 2014, 5, 32–45. [Google Scholar]
- Sawant, K.P.; Fule, R.; Maniruzzaman, M.; Amin, P.D. Extended release delivery system of metoprolol succinate using hot-melt extrusion: Effect of release modifier on methacrylic acid copolymer. Drug Deliv. Transl. Res. 2018, 8, 1679–1693. [Google Scholar] [CrossRef] [PubMed]
- Ditzinger, F.; Scherer, U.; Schönenberger, M.; Holm, R.; Kuentz, M. Modified Polymer Matrix in Pharmaceutical Hot Melt Extrusion by Molecular Interactions with a Carboxylic Coformer. Mol. Pharm. 2019, 16, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Xu, L.; Gao, R.; Luo, Y.; Tang, X. Evaluation of polymer carriers with regard to the bioavailability enhancement of bifendate solid dispersions prepared by hot-melt extrusion. Drug Dev. Ind. Pharm. 2012, 38, 735–743. [Google Scholar] [CrossRef]
- Sathigari, S.K.; Radhakrishnan, V.K.; Davis, V.A.; Parsons, D.L.; Babu, R.J. Amorphous-State Characterization of Efavirenz—Polymer Hot-Melt Extrusion Systems for Dissolution Enhancement. J. Pharm. Sci. 2012, 101, 3456–3464. [Google Scholar] [CrossRef]
- Liu, J.; Cao, F.; Zhang, C.; Ping, Q. Use of polymer combinations in the preparation of solid dispersions of a thermally unstable drug by hot-melt extrusion. Acta Pharm. Sin. B 2013, 3, 263–272. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Nollenberger, K.; Albers, J.; Craig, D.; Qi, S. Microstructure of an immiscible polymer blend and its stabilization effect on amorphous solid dispersions. Mol. Pharm. 2013, 10, 2767–2780. [Google Scholar] [CrossRef]
- Vigh, T.; Drávavölgyi, G.; Sóti, P.L.; Pataki, H.; Igricz, T.; Wagner, I.; Vajna, B.; Madarász, J.; Marosi, G.; Nagy, Z.K. Predicting final product properties of melt extruded solid dispersions from process parameters using Raman spectrometry. J. Pharm. Biomed. Anal. 2014, 98, 166–177. [Google Scholar] [CrossRef]
- Yun, F.; Kang, A.; Shan, J.; Zhao, X.; Bi, X.; Li, J.; Di, L. Preparation of osthole-polymer solid dispersions by hot-melt extrusion for dissolution and bioavailability enhancement. Int. J. Pharm. 2014, 465, 436–443. [Google Scholar] [CrossRef]
- Zhang, Y.; Luo, R.; Chen, Y.; Ke, X.; Hu, D.; Han, M. Application of carrier and plasticizer to improve the dissolution and bioavailability of poorly water-soluble baicalein by hot melt extrusion. AAPS PharmSciTech 2014, 15, 560–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Z.; Nollenberger, K.; Albers, J.; Craig, D.; Qi, S. Molecular indicators of surface and bulk instability of hot melt extruded amorphous solid dispersions. Pharm. Res. 2015, 32, 1210–1228. [Google Scholar] [CrossRef] [PubMed]
- Ashour, E.A.; Majumdar, S.; Alsheteli, A.; Alshehri, S.; Alsulays, B.; Feng, X.; Gryczke, A.; Kolter, K.; Langley, N.; Repka, M.A. Hot melt extrusion as an approach to improve solubility, permeability and oral absorption of a psychoactive natural product, piperine. J. Pharm. Pharmacol. 2016, 68, 989–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Tian, Y.; Jones, D.S.; Andrews, G.P. Optimising Drug Solubilisation in Amorphous Polymer Dispersions: Rational Selection of Hot-melt Extrusion Processing Parameters. AAPS PharmSciTech 2016, 17, 200–213. [Google Scholar] [CrossRef] [PubMed]
- Piccinni, P.; Tian, Y.; McNaughton, A.; Fraser, J.; Brown, S.; Jones, D.S.; Li, S.; Andrews, G.P. Solubility parameter-based screening methods for early-stage formulation development of itraconazole amorphous solid dispersions. J. Pharm. Pharmacol. 2016, 68, 705–720. [Google Scholar] [CrossRef] [PubMed]
- Yani, Y.; Kanaujia, P.; Chow, P.S.; Tan, R.B.H. Effect of API-Polymer Miscibility and Interaction on the Stabilization of Amorphous Solid Dispersion: A Molecular Simulation Study. Ind. Eng. Chem. Res. 2017, 56, 12698–12707. [Google Scholar] [CrossRef]
- Haser, A.; Cao, T.; Lubach, J.W.; Zhang, F. In Situ Salt Formation during Melt Extrusion for Improved Chemical Stability and Dissolution Performance of a Meloxicam-Copovidone Amorphous Solid Dispersion. Mol. Pharm. 2018, 15, 1226–1237. [Google Scholar] [CrossRef]
- Lin, X.; Su, L.; Li, N.; Hu, Y.; Tang, G.; Liu, L.; Li, H.; Yang, Z. Understanding the mechanism of dissolution enhancement for poorly water-soluble drugs by solid dispersions containing Eudragit® E PO. J. Drug Deliv. Sci. Technol. 2018, 48, 328–337. [Google Scholar] [CrossRef]
- Pinho, L.A.G.; Lima, S.G.B.; Malaquias, L.F.B.; de Pires, F.Q.; Sá-Barreto, L.L.; Cardozo-Filho, L.; Gratieri, T.; Gelfuso, G.M.; Cunha-Filho, M. Improvements of theobromine pharmaceutical properties using solid dispersions prepared with newfound technologies. Chem. Eng. Res. Des. 2018, 132, 1193–1201. [Google Scholar] [CrossRef]
- Pinho, L.A.G.; Souza, S.G.; Marreto, R.N.; Sa-Barreto, L.L.; Gratieri, T.; Gelfuso, G.M.; Cunha-Filho, M. Dissolution enhancement in cocoa extract, combining hydrophilic polymers through hot-melt extrusion. Pharmaceutics 2018, 10, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, W.; Zhu, W.; Zhang, X.; Xu, Y.; Di, L. Application of the combination of ball-milling and hot-melt extrusion in the development of an amorphous solid dispersion of a poorly water-soluble drug with high melting point. RSC Adv. 2019, 9, 22263–22273. [Google Scholar] [CrossRef] [Green Version]
- Sahoo, R.N.; De, A.; Kataria, V.; Mallick, S. Solvent-free hot melt extrusion technique in improving mesalamine release for better management of inflammatory bowel disease. Indian J. Pharm. Educ. Res. 2019, 53, S554–S562. [Google Scholar] [CrossRef] [Green Version]
- Shadambikar, G.; Kipping, T.; Di-Gallo, N.; Elia, A.G.; Knüttel, A.N.; Treffer, D.; Repka, M.A. Vacuum compression molding as a screening tool to investigate carrier suitability for hot-melt extrusion formulations. Pharmaceutics 2020, 12, 1019. [Google Scholar] [CrossRef]
- Tian, Y.; Jacobs, E.; Jones, D.S.; McCoy, C.P.; Wu, H.; Andrews, G.P. The design and development of high drug loading amorphous solid dispersion for hot-melt extrusion platform. Int. J. Pharm. 2020, 586, 119545. [Google Scholar] [CrossRef]
- Wang, W.; Li, M.; Yang, Q.; Liu, Q.; Ye, M.; Yang, G. The Opposed Effects of Polyvinylpyrrolidone K30 on Dissolution and Precipitation for Indomethacin Supersaturating Drug Delivery Systems. AAPS PharmSciTech 2020, 21, 107. [Google Scholar] [CrossRef] [PubMed]
- Lang, B.; Liu, S.; McGinity, J.W.; Williams, R.O. Effect of hydrophilic additives on the dissolution and pharmacokinetic properties of itraconazole-enteric polymer hot-melt extruded amorphous solid dispersions. Drug Dev. Ind. Pharm. 2016, 42, 429–445. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Zemlyanov, D.; Chen, X.; Su, Z.; Nie, H.; Lubach, J.W.; Smith, D.; Byrn, S.; Pinal, R. Acid-base interactions in amorphous solid dispersions of lumefantrine prepared by spray-drying and hot-melt extrusion using X-ray photoelectron spectroscopy. Int. J. Pharm. 2016, 514, 456–464. [Google Scholar] [CrossRef]
- Monschke, M.; Wagner, K.G. Amorphous solid dispersions of weak bases with pH-dependent soluble polymers to overcome limited bioavailability due to gastric pH variability – An in-vitro approach. Int. J. Pharm. 2019, 564, 162–170. [Google Scholar] [CrossRef]
- Mathers, A.; Hassouna, F.; Malinová, L.; Merna, J.; Růžička, K.; Fulem, M. Impact of Hot-Melt Extrusion Processing Conditions on Physicochemical Properties of Amorphous Solid Dispersions Containing Thermally Labile Acrylic Copolymer. J. Pharm. Sci. 2020, 109, 1008–1019. [Google Scholar] [CrossRef] [PubMed]
- Monschke, M.; Kayser, K.; Wagner, K.G. Influence of Particle Size and Drug Load on Amorphous Solid Dispersions Containing pH-Dependent Soluble Polymers and the Weak Base Ketoconazole. AAPS PharmSciTech 2021, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Alshetaili, A.; Almutairy, B.K.; Alshehri, S.M.; Repka, M.A. Development and Characterization of Sustained-Released Donepezil Hydrochloride Solid Dispersions Using Hot Melt Extrusion Technology. Pharmaceutics 2021, 13, 213. [Google Scholar] [CrossRef] [PubMed]
- Abu-Diak, O.A.; Jones, D.S.; Andrews, G.P. An investigation into the dissolution properties of celecoxib melt extrudates: Understanding the role of polymer type and concentration in stabilizing supersaturated drug concentrations. Mol. Pharm. 2011, 8, 1362–1371. [Google Scholar] [CrossRef] [PubMed]
- Sarode, A.L.; Sandhu, H.; Shah, N.; Malick, W.; Zia, H. Hot melt extrusion (HME) for amorphous solid dispersions: Predictive tools for processing and impact of drug-polymer interactions on supersaturation. Eur. J. Pharm. Sci. 2013, 48, 371–384. [Google Scholar] [CrossRef]
- Maniruzzaman, M.; Morgan, D.J.; Mendham, A.P.; Pang, J.; Snowden, M.J.; Douroumis, D. Drug-polymer intermolecular interactions in hot-melt extruded solid dispersions. Int. J. Pharm. 2013, 443, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Maniruzzaman, M.; Bonnefille, M.; Aranyos, A.; Snowden, M.J.; Douroumis, D. An in-vivo and in-vitro taste masking evaluation of bitter melt-extruded drugs. J. Pharm. Pharmacol. 2014, 66, 323–337. [Google Scholar] [CrossRef]
- Maniruzzaman, M.; Douroumis, D. An in-vitro-in-vivo taste assessment of bitter drug: Comparative electronic tongues study. J. Pharm. Pharmacol. 2015, 67, 43–55. [Google Scholar] [CrossRef] [Green Version]
- Maniruzzaman, M.; Snowden, M.J.; Bradely, M.S.; Douroumis, D. Studies of intermolecular interactions in solid dispersions using advanced surface chemical analysis. RSC Adv. 2015, 5, 74212–74219. [Google Scholar] [CrossRef] [Green Version]
- Fan, W.; Zhu, W.; Zhang, X.; Di, L. The Preparation of Curcumin Sustained-Release Solid Dispersion by Hot Melt Extrusion—Ⅰ. Optimization of the Formulation. J. Pharm. Sci. 2020, 109, 1242–1252. [Google Scholar] [CrossRef]
- Fan, W.; Zhang, X.; Zhu, W.; Di, L. The Preparation of Curcumin Sustained-Release Solid Dispersion by Hot-Melt Extrusion—Ⅱ. Optimization of Preparation Process and Evaluation In Vitro and In Vivo. J. Pharm. Sci. 2020, 109, 1253–1260. [Google Scholar] [CrossRef]
- Gryczke, A.; Schminke, S.; Maniruzzaman, M.; Beck, J.; Douroumis, D. Development and evaluation of orally disintegrating tablets (ODTs) containing Ibuprofen granules prepared by hot melt extrusion. Colloids Surfaces B Biointerfaces 2011, 86, 275–284. [Google Scholar] [CrossRef]
- Jijun, F.; Lishuang, X.; Xiaoli, W.; Shu, Z.; Xiaoguang, T.; Xingna, Z.; Haibing, H.; Xing, T. Nimodipine (NM) tablets with high dissolution containing NM solid dispersions prepared by hot-melt extrusion. Drug Dev. Ind. Pharm. 2011, 37, 934–944. [Google Scholar] [CrossRef] [PubMed]
- Kindermann, C.; Matthée, K.; Sievert, F.; Breitkreutz, J. Electrolyte-Stimulated biphasic dissolution profile and stability enhancement for tablets containing drug-Polyelectrolyte complexes. Pharm. Res. 2012, 29, 2710–2721. [Google Scholar] [CrossRef]
- Alshehri, S.M.; Park, J.B.; Alsulays, B.B.; Tiwari, R.V.; Almutairy, B.; Alshetaili, A.S.; Morott, J.; Shah, S.; Kulkarni, V.; Majumdar, S.; et al. Mefenamic acid taste-masked oral disintegrating tablets with enhanced solubility via molecular interaction produced by hot melt extrusion technology. J. Drug Deliv. Sci. Technol. 2015, 27, 18–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claeys, B.; Vandeputte, R.; De Geest, B.G.; Remon, J.P.; Vervaet, C. PH-independent immediate release polymethacrylate formulations-An observational study. Drug Dev. Ind. Pharm. 2016, 42, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Alshetaili, A.S.; Almutairy, B.K.; Tiwari, R.V.; Morott, J.T.; Alshehri, S.M.; Feng, X.; Alsulays, B.B.; Park, J.B.; Zhang, F.; Repka, M.A. Preparation and Evaluation of Hot-Melt Extruded Patient-Centric Ketoprofen Mini-Tablets. Curr. Drug Deliv. 2016, 13, 730–741. [Google Scholar] [CrossRef]
- Grymonpré, W.; Verstraete, G.; Van Bockstal, P.J.; Van Renterghem, J.; Rombouts, P.; De Beer, T.; Remon, J.P.; Vervaet, C. In-line monitoring of compaction properties on a rotary tablet press during tablet manufacturing of hot-melt extruded amorphous solid dispersions. Int. J. Pharm. 2017, 517, 348–358. [Google Scholar] [CrossRef] [Green Version]
- Nukala, P.K.; Palekar, S.; Patki, M.; Fu, Y.; Patel, K. Multi-dose oral abuse deterrent formulation of loperamide using hot melt extrusion. Int. J. Pharm. 2019, 569, 118629. [Google Scholar] [CrossRef]
- Feng, Z.; Li, M.; Wang, W. Improvement of dissolution and tabletability of carbamazepine solid dispersions with high drug loading prepared by hot-melt extrusion. Pharmazie 2019, 74, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Bennett, R.C.; Keen, J.M.; Bi, Y.; Porter, S.; Dürig, T.; McGinity, J.W. Investigation of the interactions of enteric and hydrophilic polymers to enhance dissolution of griseofulvin following hot melt extrusion processing. J. Pharm. Pharmacol. 2015, 67, 918–938. [Google Scholar] [CrossRef]
- Almutairy, B.K.; Alshetaili, A.S.; Ashour, E.A.; Patil, H.; Tiwari, R.V.; Alshehri, S.M.; Repka, M.A. Development of a floating drug delivery system with superior buoyancy in gastric fluid using hot-melt extrusion coupled with pressurized CO2. Pharmazie 2016, 71, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Partheniadis, I.; Karantzalis, A.E.; Shah, R.R.; Al-Zoubi, N.; Nikolakakis, I. Influence of compression at elevated temperature on the compactibility of thermo-mechanically processed polymers. Chem. Eng. Res. Des. 2020, 156, 64–75. [Google Scholar] [CrossRef]
- Kindermann, C.; Matthée, K.; Strohmeyer, J.; Sievert, F.; Breitkreutz, J. Tailor-made release triggering from hot-melt extruded complexes of basic polyelectrolyte and poorly water-soluble drugs. Eur. J. Pharm. Biopharm. 2011, 79, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Majumdar, S.; Deng, W.; Mohammed, N.N.; Chittiboyina, A.G.; Raman, V.; Shah, S.; Repka, M.A. Development and characterization of taste masked Efavirenz pellets utilizing hot melt extrusion. J. Drug Deliv. Sci. Technol. 2013, 23, 157–163. [Google Scholar] [CrossRef]
- Sharma, V.J.; Amin, P.D. Development of extended release matrices of rifampicin using hot melt extrusion technique. J. Appl. Pharm. Sci. 2013, 3, 30–38. [Google Scholar] [CrossRef]
- Patwardhan, K.; Asgarzadeh, F.; Dassinger, T.; Albers, J.; Repka, M.A. A quality by design approach to understand formulation and process variability in pharmaceutical melt extrusion processes. J. Pharm. Pharmacol. 2015, 67, 673–684. [Google Scholar] [CrossRef]
- Li, S.; Yu, T.; Tian, Y.; McCoy, C.P.; Jones, D.S.; Andrews, G.P. Mechanochemical synthesis of pharmaceutical cocrystal suspensions via hot melt extrusion: Feasibility studies and physicochemical characterization. Mol. Pharm. 2016, 13, 3054–3068. [Google Scholar] [CrossRef] [Green Version]
- Tiwari, R.V.; Polk, A.N.; Patil, H.; Ye, X.; Pimparade, M.B.; Repka, M.A. Rat Palatability Study for Taste Assessment of Caffeine Citrate Formulation Prepared via Hot-Melt Extrusion Technology. AAPS PharmSciTech 2017, 18, 341–348. [Google Scholar] [CrossRef]
- Desai, D.; Sandhu, H.; Shah, N.; Malick, W.; Zia, H.; Phuapradit, W.; Vaka, S.R.K. Selection of Solid-State Plasticizers as Processing Aids for Hot-Melt Extrusion. J. Pharm. Sci. 2018, 107, 372–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hörmann, T.R.; Jäger, N.; Funke, A.; Mürb, R.K.; Khinast, J.G.; Paudel, A. Formulation performance and processability window for manufacturing a dual-polymer amorphous solid dispersion via hot-melt extrusion and strand pelletization. Int. J. Pharm. 2018, 553, 408–421. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Hu, Y.; Tang, G.; Dong, M.; Liu, Q.; Lin, X. Development of ibuprofen dry suspensions by hot melt extrusion: Characterization, physical stability and pharmacokinetic studies. J. Drug Deliv. Sci. Technol. 2019, 54, 101313. [Google Scholar] [CrossRef]
- Yan, G.; Liang, Q.; Wen, X.; Peng, J.; Deng, R.; Lv, L.; Ji, M.; Deng, X.; Wu, L.; Feng, X.; et al. Preparation, characterization, and pharmacokinetics of tilmicosin taste-masked formulation via hot-melt extrusion technology. Colloids Surfaces B Biointerfaces 2020, 196, 111293. [Google Scholar] [CrossRef] [PubMed]
- Hörmann, T.R.; Rehrl, J.; Scheibelhofer, O.; Schaden, L.M.; Funke, A.; Makert, C.; Khinast, J.G. Sensitivity of a continuous hot-melt extrusion and strand pelletization line to control actions and composition variation. Int. J. Pharm. 2019, 566, 239–253. [Google Scholar] [CrossRef]
- Gue, E.; Willart, J.F.; Muschert, S.; Danede, F.; Delcourt, E.; Descamps, M.; Siepmann, J. Accelerated ketoprofen release from polymeric matrices: Importance of the homogeneity/heterogeneity of excipient distribution. Int. J. Pharm. 2013, 457, 298–307. [Google Scholar] [CrossRef]
- Thakkar, R.; Komanduri, N.; Dudhipala, N.; Tripathi, S.; Repka, M.A.; Majumdar, S. Development and optimization of hot-melt extruded moxifloxacin hydrochloride inserts, for ocular applications, using the design of experiments. Int. J. Pharm. 2021, 603, 120676. [Google Scholar] [CrossRef]
- Bialleck, S.; Rein, H. Preparation of starch-based pellets by hot-melt extrusion. Eur. J. Pharm. Biopharm. 2011, 79, 440–448. [Google Scholar] [CrossRef]
- Vynckier, A.K.; De Beer, M.; Monteyne, T.; Voorspoels, J.; De Beer, T.; Remon, J.P.; Vervaet, C. Enteric protection of naproxen in a fixed-dose combination product produced by hot-melt co-extrusion. Int. J. Pharm. 2015, 491, 243–249. [Google Scholar] [CrossRef] [Green Version]
- Palem, C.R.; Kumar Battu, S.; Maddineni, S.; Gannu, R.; Repka, M.A.; Yamsani, M.R. Oral transmucosal delivery of domperidone from immediate release films produced via hot-melt extrusion technology. Pharm. Dev. Technol. 2013, 18, 186–195. [Google Scholar] [CrossRef]
- Speer, I.; Preis, M.; Breitkreutz, J. Prolonged drug release properties for orodispersible films by combining hot-melt extrusion and solvent casting methods. Eur. J. Pharm. Biopharm. 2018, 129, 66–73. [Google Scholar] [CrossRef]
- Saerens, L.; Vervaet, C.; Remon, J.P.; De Beer, T. Visualization and process understanding of material behavior in the extrusion barrel during a hot-melt extrusion process using raman spectroscopy. Anal. Chem. 2013, 85, 5420–5429. [Google Scholar] [CrossRef]
- Bounartzi, M.; Panagopoulou, A.; Kantiranis, N.; Malamataris, S.; Nikolakakis, I. Effect of plasticiser type on the hot melt extrusion of venlafaxine hydrochloride. J. Pharm. Pharmacol. 2014, 66, 297–308. [Google Scholar] [CrossRef]
- Tiwari, R.; Agarwal, S.K.; Murthy, R.S.R.; Tiwari, S. Formulation and evaluation of sustained release extrudes prepared via novel hot melt extrusion technique. J. Pharm. Innov. 2014, 9, 246–258. [Google Scholar] [CrossRef]
- Malode, V.N.; Paradkar, A.; Devarajan, P.V. Controlled release floating multiparticulates of metoprolol succinate by hot melt extrusion. Int. J. Pharm. 2015, 491, 345–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avgerinos, T.; Kantiranis, N.; Panagopoulou, A.; Malamataris, S.; Kachrimanis, K.; Nikolakakis, I. Mechanical properties and drug release of venlafaxine HCl solid mini matrices prepared by hot-melt extrusion and hot or ambient compression. Drug Dev. Ind. Pharm. 2018, 44, 338–348. [Google Scholar] [CrossRef]
- Cassidy, C.M.; Tunney, M.M.; Caldwell, D.L.; Andrews, G.P.; Donnelly, R.F. Development of novel oral formulations prepared via hot melt extrusion for targeted delivery of photosensitizer to the colon. Photochem. Photobiol. 2011, 87, 867–876. [Google Scholar] [CrossRef]
- Simons, F.J.; Wagner, K.G. Modeling, design and manufacture of innovative floating gastroretentive drug delivery systems based on hot-melt extruded tubes. Eur. J. Pharm. Biopharm. 2019, 137, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Vo, A.Q.; Feng, X.; Morott, J.T.; Pimparade, M.B.; Tiwari, R.V.; Zhang, F.; Repka, M.A. A novel floating controlled release drug delivery system prepared by hot-melt extrusion. Eur. J. Pharm. Biopharm. 2016, 98, 108–121. [Google Scholar] [CrossRef] [Green Version]
- Schittny, A.; Huwyler, J.; Puchkov, M. Mechanisms of increased bioavailability through amorphous solid dispersions: A review. Drug Deliv. 2020, 27, 110–127. [Google Scholar] [CrossRef]
- Zhang, J.; Han, R.; Chen, W.; Zhang, W.; Li, Y.; Ji, Y.; Chen, L.; Pan, H.; Yang, X.; Pan, W.; et al. Analysis of the literature and patents on solid dispersions from 1980 to 2015. Molecules 2018, 23, 1697. [Google Scholar] [CrossRef] [Green Version]
- Hancock, B.C.; Zografi, G. Characteristics and Significance of the Amorphous State in Pharmaceutical Systems. J. Pharm. Sci. 1997, 86, 1–12. [Google Scholar] [CrossRef]
- Deng, Y.; Shen, L.; Yang, Y.; Shen, J. Development of nanoparticle-based orodispersible palatable pediatric formulations. Int. J. Pharm. 2021, 596, 120206. [Google Scholar] [CrossRef]
- Foppoli, A.A.; Maroni, A.; Cerea, M.; Zema, L.; Gazzaniga, A. Dry coating of solid dosage forms: An overview of processes and applications. Drug Dev. Ind. Pharm. 2017, 43, 1919–1931. [Google Scholar] [CrossRef]
- Saeki, I.; Kondo, K.; Furukoshi, Y.; Watanabe, Y.; Niwa, T. Design of taste-masked swellable drug particles using dry-coating technology with mechanical curing. Eur. J. Pharm. Biopharm. 2021, 160, 9–22. [Google Scholar] [CrossRef]
- Laubach, J.; Joseph, M.; Brenza, T.; Gadhamshetty, V.; Sani, R.K. Exopolysaccharide and biopolymer-derived films as tools for transdermal drug delivery. J. Control. Release 2021, 329, 971–987. [Google Scholar] [CrossRef]
- Jacob, S.; Nair, A.B.; Patel, V.; Shah, J. 3D Printing Technologies: Recent Development and Emerging Applications in Various Drug Delivery Systems. AAPS PharmSciTech 2020, 21, 220. [Google Scholar] [CrossRef] [PubMed]
- Alhijjaj, M.; Belton, P.; Qi, S. An investigation into the use of polymer blends to improve the printability of and regulate drug release from pharmaceutical solid dispersions prepared via fused deposition modeling (FDM) 3D printing. Eur. J. Pharm. Biopharm. 2016, 108, 111–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadia, M.; Sośnicka, A.; Arafat, B.; Isreb, A.; Ahmed, W.; Kelarakis, A.; Alhnan, M.A. Adaptation of pharmaceutical excipients to FDM 3D printing for the fabrication of patient-tailored immediate release tablets. Int. J. Pharm. 2016, 513, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Arafat, B.; Qinna, N.; Cieszynska, M.; Forbes, R.T.; Alhnan, M.A. Tailored on demand anti-coagulant dosing: An in vitro and in vivo evaluation of 3D printed purpose-designed oral dosage forms. Eur. J. Pharm. Biopharm. 2018, 128, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Nasereddin, J.M.; Wellner, N.; Alhijjaj, M.; Belton, P.; Qi, S. Development of a Simple Mechanical Screening Method for Predicting the Feedability of a Pharmaceutical FDM 3D Printing Filament. Pharm. Res. 2018, 35, 151. [Google Scholar] [CrossRef] [Green Version]
- Sadia, M.; Arafat, B.; Ahmed, W.; Forbes, R.T.; Alhnan, M.A. Channelled tablets: An innovative approach to accelerating drug release from 3D printed tablets. J. Control. Release 2018, 269, 355–363. [Google Scholar] [CrossRef]
- Sadia, M.; Isreb, A.; Abbadi, I.; Isreb, M.; Aziz, D.; Selo, A.; Timmins, P.; Alhnan, M.A. From ‘fixed dose combinations’ to ‘a dynamic dose combiner’: 3D printed bi-layer antihypertensive tablets. Eur. J. Pharm. Sci. 2018, 123, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Gültekin, H.E.; Tort, S.; Acartürk, F. An Effective Technology for the Development of Immediate Release Solid Dosage Forms Containing Low-Dose Drug: Fused Deposition Modeling 3D Printing. Pharm. Res. 2019, 36, 128. [Google Scholar] [CrossRef] [PubMed]
- Ilyés, K.; Kovács, N.K.; Balogh, A.; Borbás, E.; Farkas, B.; Casian, T.; Marosi, G.; Tomuță, I.; Nagy, Z.K. The applicability of pharmaceutical polymeric blends for the fused deposition modelling (FDM) 3D technique: Material considerations–printability–process modulation, with consecutive effects on in vitro release, stability and degradation. Eur. J. Pharm. Sci. 2019, 129, 110–123. [Google Scholar] [CrossRef] [PubMed]
- Fanous, M.; Bitar, M.; Gold, S.; Sobczuk, A.; Hirsch, S.; Ogorka, J.; Imanidis, G. Development of immediate release 3D-printed dosage forms for a poorly water-soluble drug by fused deposition modeling: Study of morphology, solid state and dissolution. Int. J. Pharm. 2021, 599, 120417. [Google Scholar] [CrossRef] [PubMed]
- Than, Y.M.; Titapiwatanakun, V. Tailoring immediate release FDM 3D printed tablets using a quality by design (QbD) approach. Int. J. Pharm. 2021, 599, 120402. [Google Scholar] [CrossRef]
- Linares, V.; Casas, M.; Caraballo, I. Printfills: 3D printed systems combining fused deposition modeling and injection volume filling. Application to colon-specific drug delivery. Eur. J. Pharm. Biopharm. 2019, 134, 138–143. [Google Scholar] [CrossRef]
- Goyanes, A.; Chang, H.; Sedough, D.; Hatton, G.B.; Wang, J.; Buanz, A.; Gaisford, S.; Basit, A.W. Fabrication of controlled-release budesonide tablets via desktop (FDM) 3D printing. Int. J. Pharm. 2015, 496, 414–420. [Google Scholar] [CrossRef]
- Zhang, J.; Feng, X.; Patil, H.; Tiwari, R.V.; Repka, M.A. Coupling 3D printing with hot-melt extrusion to produce controlled-release tablets. Int. J. Pharm. 2017, 519, 186–197. [Google Scholar] [CrossRef]
- Okwuosa, T.C.; Pereira, B.C.; Arafat, B.; Cieszynska, M.; Isreb, A.; Alhnan, M.A. Fabricating a Shell-Core Delayed Release Tablet Using Dual FDM 3D Printing for Patient-Centred Therapy. Pharm. Res. 2017, 34, 427–437. [Google Scholar] [CrossRef]
- Nober, C.; Manini, G.; Carlier, E.; Raquez, J.M.; Benali, S.; Dubois, P.; Amighi, K.; Goole, J. Feasibility study into the potential use of fused-deposition modeling to manufacture 3D-printed enteric capsules in compounding pharmacies. Int. J. Pharm. 2019, 569, 118581. [Google Scholar] [CrossRef] [PubMed]
- Keikhosravi, N.; Mirdamadian, S.Z.; Varshosaz, J.; Taheri, A. Preparation and characterization of polypills containing aspirin and simvastatin using 3D printing technology for the prevention of cardiovascular diseases. Drug Dev. Ind. Pharm. 2020, 46, 1665–1675. [Google Scholar] [CrossRef] [PubMed]
- Gioumouxouzis, C.I.; Baklavaridis, A.; Katsamenis, O.L.; Markopoulou, C.K.; Bouropoulos, N.; Tzetzis, D.; Fatouros, D.G. A 3D printed bilayer oral solid dosage form combining metformin for prolonged and glimepiride for immediate drug delivery. Eur. J. Pharm. Sci. 2018, 120, 40–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korte, C.; Quodbach, J. Formulation development and process analysis of drug-loaded filaments manufactured via hot-melt extrusion for 3D-printing of medicines. Pharm. Dev. Technol. 2018, 23, 1117–1127. [Google Scholar] [CrossRef]
- Korte, C.; Quodbach, J. 3D-Printed Network Structures as Controlled-Release Drug Delivery Systems: Dose Adjustment, API Release Analysis and Prediction. AAPS PharmSciTech 2018, 19, 3333–3342. [Google Scholar] [CrossRef]
- Xu, P.; Li, J.; Meda, A.; Osei-Yeboah, F.; Peterson, M.L.; Repka, M.; Zhan, X. Development of a quantitative method to evaluate the printability of filaments for fused deposition modeling 3D printing. Int. J. Pharm. 2020, 588, 119760. [Google Scholar] [CrossRef]
- Beck, R.C.R.; Chaves, P.S.; Goyanes, A.; Vukosavljevic, B.; Buanz, A.; Windbergs, M.; Basit, A.W.; Gaisford, S. 3D printed tablets loaded with polymeric nanocapsules: An innovative approach to produce customized drug delivery systems. Int. J. Pharm. 2017, 528, 268–279. [Google Scholar] [CrossRef]
- Kempin, W.; Franz, C.; Koster, L.C.; Schneider, F.; Bogdahn, M.; Weitschies, W.; Seidlitz, A. Assessment of different polymers and drug loads for fused deposition modeling of drug loaded implants. Eur. J. Pharm. Biopharm. 2017, 115, 84–93. [Google Scholar] [CrossRef]
- Ilyés, K.; Balogh, A.; Casian, T.; Igricz, T.; Borbás, E.; Démuth, B.; Vass, P.; Menyhárt, L.; Kovács, N.K.; Marosi, G.; et al. 3D floating tablets: Appropriate 3D design from the perspective of different in vitro dissolution testing methodologies. Int. J. Pharm. 2019, 567, 118433. [Google Scholar] [CrossRef]
- Chaudhari, V.S.; Malakar, T.K.; Murty, U.S.; Banerjee, S. Extruded filaments derived 3D printed medicated skin patch to mitigate destructive pulmonary tuberculosis: Design to delivery. Expert Opin. Drug Deliv. 2020, 18, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Berg, S.; Krause, J.; Björkbom, A.; Walter, K.; Harun, S.; Granfeldt, A.; Janzén, D.; Nunes, S.F.; Antonsson, M.; Van Zuydam, N.; et al. In Vitro and In Vivo Evaluation of 3D Printed Capsules with Pressure Triggered Release Mechanism for Oral Peptide Delivery. J. Pharm. Sci. 2021, 110, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Krause, J.; Bogdahn, M.; Schneider, F.; Koziolek, M.; Weitschies, W. Design and characterization of a novel 3D printed pressure-controlled drug delivery system. Eur. J. Pharm. Sci. 2019, 140, 105060. [Google Scholar] [CrossRef] [PubMed]
- Pietrzak, K.; Isreb, A.; Alhnan, M.A. A flexible-dose dispenser for immediate and extended release 3D printed tablets. Eur. J. Pharm. Biopharm. 2015, 96, 380–387. [Google Scholar] [CrossRef]
- Öblom, H.; Zhang, J.; Pimparade, M.; Speer, I.; Preis, M.; Repka, M.; Sandler, N. 3D-Printed Isoniazid Tablets for the Treatment and Prevention of Tuberculosis — Personalized Dosing and Drug Release. AAPS PharmSciTech 2019, 20, 52. [Google Scholar] [CrossRef] [Green Version]
- Okwuosa, T.C.; Soares, C.; Gollwitzer, V.; Habashy, R.; Timmins, P.; Alhnan, M.A. On demand manufacturing of patient-specific liquid capsules via co-ordinated 3D printing and liquid dispensing. Eur. J. Pharm. Sci. 2018, 118, 134–143. [Google Scholar] [CrossRef] [Green Version]
- Shi, K.; Slavage, J.P.; Maniruzzaman, M.; Nokhodchi, A. Role of release modifiers to modulate drug release from fused deposition modelling (FDM) 3D printed tablets. Int. J. Pharm. 2021, 597, 120315. [Google Scholar] [CrossRef] [PubMed]
- Melocchi, A.; Parietti, F.; Maroni, A.; Foppoli, A.; Gazzaniga, A.; Zema, L. Hot-melt extruded fi laments based on pharmaceutical grade polymers for 3D printing by fused deposition modeling. Int. J. Pharm. 2016, 509, 255–263. [Google Scholar] [CrossRef]
- Gioumouxouzis, C.I.; Chatzitaki, A.T.; Karavasili, C.; Katsamenis, O.L.; Tzetzis, D.; Mystiridou, E.; Bouropoulos, N.; Fatouros, D.G. Controlled Release of 5-Fluorouracil from Alginate Beads Encapsulated in 3D Printed pH-Responsive Solid Dosage Forms. AAPS PharmSciTech 2018, 19, 3362–3375. [Google Scholar] [CrossRef] [Green Version]
- Melocchi, A.; Uboldi, M.; Inverardi, N.; Briatico-Vangosa, F.; Baldi, F.; Pandini, S.; Scalet, G.; Auricchio, F.; Cerea, M.; Foppoli, A.; et al. Expandable drug delivery system for gastric retention based on shape memory polymers: Development via 4D printing and extrusion. Int. J. Pharm. 2019, 571, 118700. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, J.C.; Ko, J.Y.; Lee, S.H.; Kim, N.A.; Jeong, S.H. 3D-printed tablets using a single-step hot-melt pneumatic process for poorly soluble drugs. Int. J. Pharm. 2021, 595, 120257. [Google Scholar] [CrossRef]
- Musazzi, U.M.; Ortenzi, M.A.; Gennari, C.G.M.; Casiraghi, A.; Minghetti, P.; Cilurzo, F. Design of pressure-sensitive adhesive suitable for the preparation of transdermal patches by hot-melt printing. Int. J. Pharm. 2020, 586, 119607. [Google Scholar] [CrossRef] [PubMed]
- Kuzminska, M.; Pereira, B.C.; Habashy, R.; Peak, M.; Isreb, M.; Gough, T.D.; Isreb, A.; Alhnan, M.A. Solvent-free temperature-facilitated direct extrusion 3D printing for pharmaceuticals d. Int. J. Phamaceutics 2021, 598, 120305. [Google Scholar] [CrossRef]
- Fina, F.; Goyanes, A.; Gaisford, S.; Basit, A.W. Selective laser sintering (SLS) 3D printing of medicines. Int. J. Pharm. 2017, 529, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Fina, F.; Goyanes, A.; Madla, C.M.; Awad, A.; Trenfield, S.J.; Kuek, J.M.; Patel, P.; Gaisford, S.; Basit, A.W. 3D printing of drug-loaded gyroid lattices using selective laser sintering. Int. J. Pharm. 2018, 547, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Fuenmayor, E.; Forde, M.; Healy, A.V.; Devine, D.M.; Lyons, J.G.; McConville, C.; Major, I. Material considerations for fused-filament fabrication of solid dosage forms. Pharmaceutics 2018, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Tabriz, A.G.; Scoutaris, N.; Gong, Y.; Hui, H.-W.; Kumar, S.; Douroumis, D. Investigation on hot melt extrusion and prediction on 3D printability of pharmaceutical grade polymers. Int. J. Pharm. 2021, 604, 120755. [Google Scholar] [CrossRef] [PubMed]
- Moseson, D.E.; Jordan, M.A.; Shah, D.D.; Corum, I.D.; Alvarenga, B.R.; Taylor, L.S. Application and limitations of thermogravimetric analysis to delineate the hot melt extrusion chemical stability processing window. Int. J. Pharm. 2020, 590, 119916. [Google Scholar] [CrossRef] [PubMed]
- Fanous, M.; Gold, S.; Hirsch, S.; Ogorka, J.; Imanidis, G. Development of immediate release (IR) 3D-printed oral dosage forms with focus on industrial relevance. Eur. J. Pharm. Sci. 2020, 155, 105558. [Google Scholar] [CrossRef] [PubMed]
- Giridhar, G.; Manepalli, R.R.K.N.; Apparao, G. Confocal Raman Spectroscopy. Spectrosc. Methods Nanomater. Charact. 2017, 2, 141–161. [Google Scholar] [CrossRef]




| Eudragit | Substituents | pH-Dependent Solubility | Molecular Weight (g/mol) | Glass Transition Temperature (°C) | Availability |
|---|---|---|---|---|---|
| Eudragit E PO | R1, R3 = CH3, R2 = CH2CH2N(CH3)2, R4 = CH3, C4H9 | Gastric fluid up pH 5.0 | 47,000 | 48 | Powder with amine like odor |
| Eudragit E 100 | R1, R3 = CH3, R2 = CH2CH2N(CH3)2, R4 = CH3, C4H9 | Gastric fluid up pH 5.0 | 47,000 | 48 | Granules |
| Eudragit RL PO | R1 = H, CH3, R2 = CH3, C2H5, R3 = CH3, R4 = CH2CH2N(CH3)3+ Cl− | Insoluble, high permeability | 32,000 | 70 | White powder with a faint amine like odor |
| Eudragit RL100 | R1 = H, CH3, R2 = CH3, C2H5, R3 = CH3, R4 = CH2CH2N(CH3)3+ Cl− | Insoluble, high permeability | 32,000 | 70 | Colorless, clear to cloudy granules with a faint amine like odor |
| Eudragit RS PO | R1 = H, CH3, R2 = CH3, C2H5, R3 = CH3, R4 = CH2CH2N(CH3)3+ Cl− | Insoluble, low permeability | 32,000 | 64 | White powder with a faint amine like odor |
| Eudragit RS100 | R1 = H, CH3, R2 = CH3, C2H5, R3 = CH3, R4 = CH2CH2N(CH3)3+ Cl− | Insoluble, low permeability | 32,000 | 64 | Colorless granule with a faint amine like odor |
| Eudragit L100 | R1, R3 = CH3, R2 = H, R4 = CH3 | Above pH 6.0 | 125,000 | 150 | Solid powder with a faint characteristic odor |
| Eudragit L100-55 | R1, R3 = H, CH3, R2 = H, R4 = CH3, C2H5 | Above pH 5.5 | 320,000 | 110 | White powder with a faint characteristic odor |
| Eudragit S100 | R1, R3 = CH3, R2 = H, R4 = CH3 | Above pH 7.0 | 125,000 | 150 | White powder with a faint characteristic odor |
| Eudragit FS 30D | R1 = H, R2 = H, CH3, R3 = CH3, R4 = CH3 | Above pH 7.0 | 280,000 | 48 | Aqueous dispersion 30%, Milky-white liquid of low viscosity with a faint characteristic odor |
| Eudragit Type | Extrusion Temperature (°C) | Polymer Role | Drug | Release Data $ | Reference |
|---|---|---|---|---|---|
| Eudragit E | 130 | Polymeric matrix | Fenofibrate | ≅70% in 90′ (drug:polymer); ≅100%, 15′ (drug:polymer:MA) | [49] |
| Eudragit E PO | 180 | Polymeric matrix | Bifendate | ≅90% in 30′ | [50] |
| 120 | Polymeric matrix | Efavirenz | 96% in 30′ | [51] | |
| 165 and 185 | Polymeric matrix | Carbamazepine | 100% in 20′ | [52] | |
| 150 | Polymeric matrix | Felodipine | ≅37% in 40′ (10% drug); ≅11% in 40′ (30% drug); ≅12% in 40′ (50% drug); ≅15% in 40′ (70% drug) | [53] | |
| 110–150 | Polymeric matrix | Spironolactone | > 95%, 60′ | [54] | |
| 85 | Polymeric matrix | Osthole | 43% in 30′ (drug: polymer, 1:3), 81% in 30′ (drug: polymer, 1:6); and 84% in 30′ (drug: polymer, 1:9) | [55] | |
| 160 | Polymeric matrix | Baicalein | 90%, 90′ | [56] | |
| 5 °C higher than the melting point of the individual drugs | Polymeric matrix | Carbamazepine, celecoxib, felodipine, fenofibrate | * | [57] | |
| 110 | Polymeric matrix | Piperine | ≅20% in 120′ | [58] | |
| 110–150 | Polymeric matrix | Felodipine | * | [59] | |
| 170 # | Polymeric matrix | Itraconazole | * | [60] | |
| 90 | Polymeric matrix | Ibuprofen | 85% in 5′ | [61] | |
| 110–140 | pH modification agent | Meloxican | * | [62] | |
| 130 | Polymeric matrix/Taste-masker agent | Isoniazid | 100% in 5′ (20% drug); 100% in 15′ (30% drug) | [33] | |
| 90–180 | Polymeric matrix | Bifendate, felodipine and ibuprofen | 100% in 15′ (1% BIF); 100% in 15′ (0.7% FEL); >90% in 15′ (1.5% FEL); 100% in 10′ (4% IBU); 100% in 10′ (10% IBU); | [63] | |
| 150 | Polymeric matrix | Theobromine | >80% in 10′ | [64] | |
| 150–160 | Polymeric matrix | Cocoa extract/Theobromine | ≅80% in 30′ (EPO); ≅86% in 30′(EPO: Sol); ≅85% in 30′ (EPO:PVP); ≅80% in 30′ (EPO:Sol:PVP) | [65] | |
| 160 | Polymeric matrix | Resveratrol | ≅85% in 20′ | [66] | |
| 80–150 | Polymeric matrix | Mesalamine | >97% in 60′ | [67] | |
| 160 | Polymeric matrix | Indomethacin | ≅84% in 15′ | [68] | |
| 65–120 | Polymeric matrix | Ibuprofen, indhometacin and naproxen | * | [69] | |
| 140 | Polymeric matrix | Indomethacin | ≅54% in 5′ (drug:EPO, 4:1); ≅28% in 5′(drug:EPO: PVP, 4:1:0.01); <22% in 60′ (drug:EPO: PVP, 4:1:0.05 and 4:1:1) | [70] | |
| Eudragit L100-55 | 160 | Polymeric matrix | Itraconazole | 18% in 2 h | [71] |
| 130 | Polymeric matrix | Lumefantrine | * | [72] | |
| 100–150 | Polymeric matrix | Nevirapine | <5% in pH 1 (milled and pellet); ≅30% (milled) and ≅10% (pellet) in pH 5.5; ≅90% (milled) and ≅70% (pellet) in pH 6.8 | [73] | |
| 90–170 | Polymeric matrix | Ibuprofen | ≅90% in 60′, PBS pH 6.8 | [74] | |
| 100–140 | Polymeric matrix | Ketoconazole | ** | [75] | |
| Eudragit RS PO | 150 | Polymeric matrix | Donepezil hydrochloride | ≅30% in 10 h | [76] |
| Eudragit 4155F | 170 | Polymeric matrix | Celecoxib | 100.67% in 72 h (drug:polymer, 1:9); 53.37% in 72 h (drug:polymer, 3:7) | [77] |
| Eudragit E PO | *** | Polymeric matrix | Indomethacin, itraconazole and griseofulvin | 109.8% in SGF (IND:polymer, 30:70) | [78] |
| Eudragit L100 | * | ||||
| Eudragit L100-55 | 74.5% in SIF (IND:polymer, 30:70); 1.9% in SGF and 20.1% in SIF (ITZ:polymer, 30:70); 94.7% in SIF (GSF: polymer, 30:70) | ||||
| Eudragit L100 | 130–165 | Polymeric matrix | Propranolol HCl and diphenhydramine HCl | * | [79] |
| Eudragit L100-55 | 100–115 | ||||
| Eudragit L100 | 100–155 | Polymeric matrix/Taste-masker agent | Cetirizine HCl and verapamil HCl | >70% in 2 h (cetirizine); >80% in 2 h (verapamil) | [80] |
| Eudragit L100-55 | |||||
| Eudragit L100 | 100–155 | Polymeric matrix/Taste-masker agent | Propranolol | * | [81] |
| Eudragit L100-55 | |||||
| Eudragit L100 | 100–155 | Polymeric matrix | Cetirizine HCl and verapamil HCl | * | [82] |
| Eudragit L100-55 | |||||
| Eudragit RL PO | 90–140 | Polymeric matrix | Metropolol | * | [37] |
| Eudragit RS PO | |||||
| Eudragit RL PO/RS PO | 135–150 | Polymeric matrix | Curcumin | ≅90% in 12 h | [83] |
| 135–150 | Polymeric matrix | Curcumin | Varying between ≅70% and >90% in 12 h, depending on the extrusion temperature, screw speed, cooling rate and particle size. | [84] |
| Eudragit Type | Extrusion Temperature (°C) | Polymer Role | Drug | Release Data $ | Technique of Tablets Obtantion | Reference |
|---|---|---|---|---|---|---|
| Eudragit E PO | 140 | Polymeric matrix | Ibuprofen | ≅65% in 120′ (drug: 25%); ≅95% in 120′ (drug:40%) | Compression | [85] |
| 80–130 | Polymeric matrix | Nimodipine | 80% in 10′ | Compression | [86] | |
| 90–125 | Polymeric matrix | Naproxen | 73% in 12 h, and 100% in 24 h (98.5% polyelectrolyte complex); 80% in 2 h (70% polyelectrolyte complex) | Compression | [87] | |
| 100–120 | Polymeric matrix | Ibuprofen and celecoxib | ≅100% in 15′ (pH 1) and in 60′ (pH 3) | Injection molding | [29] | |
| 110 | Polymeric matrix | Mefenamic acid | >80% in 5′ | Compression | [88] | |
| 90 | Polymeric matrix | Ibuprofen | ≅100% in 20′ (pH 1); ≅100% in 40′ (pH 3); <10% in 60′ (pH 5 and 7) | Injection molding | [89] | |
| 100–120 | Polymeric matrix | Ketoprofen | 100% in 20′ | Pelletization | [90] | |
| 120–140 | Polymeric matrix | Celecoxib | * | Compression | [91] | |
| 150 | Polymeric matrix | Loperamide | >85% in 15′ (single unit); <2% in 45′ (multiple unit) | Compression | [92] | |
| 140 | Polymeric matrix | Carbamazepine | >85% in 10′ (drug:polymer, 2:1 and 4:1); >85% in 20′ (drug:polymer, 1:1) | Compression | [93] | |
| Eudragit L100-55 | 170–180 | Polymeric matrix | Griseofulvin | <5% in pH 1.2; ≅36% in pH 6.8 (drug:polymer:TEC); ≅42% in pH 6.8 (drug:polymer:K12:TEC); ≅60% in pH 6.8 (drug:polymer:S630:TEC); ≅66% in pH 6.8 (drug:polymer:S630:ATBC, <45 μm); ≅66% in pH 6.8 (drug:polymer:S630:ATBC, <250 μm); | Compression | [94] |
| Eudragit RL PO | 90–165 | Polymeric matrix | Acetaminophen | 86.5% in 3 h | Pelletization | [95] |
| Eudragit E PO/RL PO/RS PO | 150 | Polymeric matrix | Metoprolol tartrate and hydrochlorothiazide | MT = 100% in 60′ (FaSSGF); <60% in 30′ (FaSSGF + 20% ethanol); HCT ≤ 20% in 30′ (FaSSGF); >50% in 30′ (FaSSGF + 20% ethanol); multitablets, MT < 7% (FaSSGF) | Compression | [7] |
| Eudragit L100-55 | 90–140 | Polymeric matrix | ** | * | Compression | [96] |
| Eudragit RS PO | 80–125 |
| Eudragit Type | Extrusion Temperature (°C) | Polymer Role | Drug | Pharmaceutical Form | Release Data $ | Reference |
|---|---|---|---|---|---|---|
| Eudragit E PO | 25–125 | Polymeric matrix | Furosemide and naproxen | Polyelectrolyte complexes | 18% in 2 h, water; 100% in 30′, if NaCl 0.15M is added at the start of release study; No release up to 1 h and 100% in 2 h, if NaCl 0.15 M is added after 1 h; >60% in 2 h, if NaCl 0.002 M is added at the start; and <10% in 30′, 20% in 1 h and 100% in 2 h if NaCl 0.002 M is added after 30′ and NaCl 0.15 M after 1 h | [97] |
| 70–110 | Polymeric matrix/Taste-masker agent | Efavirenz | Pellet | 90% in 30′ (10%, 25% and 50% of drug); <70% in 60′ (60% and 70% of drug) | [98] | |
| 110 | Polymeric matrix | Rifampicin | Pellet | 100% in 10′ | [99] | |
| 90–130 | Polymeric matrix | Ibuprofen | Extrudates | ≅70% in 1 h in pH 1.2 and 100% in 2 h in pH 6.8 (30% and 50% drug); ≅20% in 1 h in pH 1.2 and < 60% in 2 h in pH 6.8 (70% drug) | [100] | |
| 92 | Polymeric matrix | Ibuprofen | Cocrystal suspension | 11.64% in 3 h | [101] | |
| 130 | Polymeric matrix/Taste-masker agent | Caffeine citrate | Extrudate | <3.5% in 30” in artificial saliva; ≅99% in 12 h in water | [102] | |
| 105–120 | Polymeric matrix | Indomethacin | nd | * | [103] | |
| 120–140 | Polymeric matrix | Nimodipine | Pellet | 100% in 30′ (90% EPO; EPO:HPMC 2:1 and 2:3); 85% in 30′, (EPO:HPMC, 1:1) | [104] | |
| 120 | Polymeric matrix | Ibuprofen | Dry suspension | 90% in 5′ | [105] | |
| 135–145 | Polymeric matrix/Taste-masker agent | Tilmicosin | Extrudates | <2% in 30″ in artificial saliva; >80% in 30′ in 0.1 M HCl | [106] | |
| Eudragit E100 | 140 | Polymeric matrix | Nimodipine | Pellet | 85% in 30′ | [107] |
| Eudragit E100 PO | 85–130 | Polymeric matrix | Ketoprofen | Extrudates | 100% in 30′ (drug:polymer, 10:90, 30:70, 50:50); ≅80% in 2 h (drug:polymer:PVP, 30:50:20); ≅60% in 2 h (drug:polymer:PVPVA, 30:50:20); >80% in 2 h (drug:polymer:HPMC 30:50:20); | [108] |
| Eudragit FS 100 | 90 | Polymeric matrix | Moxifloxacin hydrochloride | Ocular insert | >70% in 24 h | [109] |
| Eudragit L100 | 35–78 | Release modifier | Acetaminophen, ibuprofen, phenazon and tramadol-HCl | Pellet | 100% in 1 h | [110] |
| Eudragit L100-55 | 100–125 | Polymeric matrix | Esomeprazole and naproxen | Fixed-dose combination extrudate | No drug release in 2 h in 0.1 N HCl, 100% in 12 h in pH 6.8 | [111] |
| Eudragit RL PO | 120–160 | Polymeric matrix | Domperidone | Film | 49% in 2 h | [112] |
| 120–135 | Polymeric matrix | Noscapine | Sustained release extrudate | 10.93% in 2 h in pH 1.2 and 22.25% in 24 h in pH 6.8 (formulation without CA); 13.68% in 2 h in pH 1.2 and 70.99% in 24 h in pH 6.8 (with 10% CA); | [35] | |
| Eudragit RS | 20–160 | Polymeric matrix | Theophylline | Orodispersible film | 80% in > 120′ (particle size < 315 μm); ≅85% in 1000′ (500–715 μm); ≅50% in 1000′ (>1000 μm) | [113] |
| Eudragit RS PO | 70–140 | Polymeric matrix | Metropolol tartrate | Extrudates | * | [114] |
| 90–120 | Polymeric matrix | Venlafaxine HCl | Extrudates | * | [115] | |
| 45–150 | Polymeric matrix | Venlafaxine HCl | Extrudates | 72% to 95% in 8 h | [116] | |
| 40–128 | Polymeric matrix | Metropolol succinate | Floating multiparticulates | 100% in 12 h | [117] | |
| 90–100 | Polymeric matrix | Ibuprofen | Trandermal film | RS (100%) 21.6% in 24 h; RS:Suc (60:10) 21.8% in 24 h; RS:MC (60:10) 25.5% in 24 h; RS:MC (10:60) 99% in 24 h; RS:XG (60:10) 82.7% in 24 h; RS:XG (10:60) 94.4% in 24 h; RS: Pol (60:10) 42.9% in 24 h; RS:Gel (60:10) 58.2% in 24 h; RS:Gel (50:20) 98.1% in 4 h; | [11] | |
| 90–120 | Polymeric matrix | Velafaxine | Pellet | ≅35% in 2 h (citric acid 10%); ≅50% in 2 h (citric acid 20%); ≅70% in 2 h (Lutrol 10%); ≅90% in 2 h (Lutrol 20%); | [118] | |
| Eudragit S100 | 120 | Polymeric matrix | 5-Aminolevulinic acid hexyl-ester | Extrudates | <5% in 2 h in 0.1 M HCl, 21% in 6 h in pH 7.4 | [119] |
| Methylene blue | No drug release in 2 h in 0.1 M HCl, 31% in 6 h in pH 7.4 | |||||
| Meso-tetra porphine tetra tosylate | No drug release in 2 h in 0.1 M HCl, 50% in 6 h in pH 7.4 | |||||
| 100–145 | Polymeric matrix | Ibuprofen | Pellet | 2.5% EC ≤ 18% in 6 h; 100% in 12 h (pellet 3 mm); 5% EC ≤ 18% in 6 h; 100% in 24 h (3 mm) | [9] | |
| Ketoprofen | 2.5% EC ≤ 20% in 6 h (1, 2 and 3 mm); 100% in 12 h (1 mm); 100% in 14 h (2 mm); 100% in 16 h (3 mm); 5% EC ≤ 20% in 6 h; 100% in 14 h (1 mm); 100% in 16 h (2 mm); 100% in 22 h (3 mm); | |||||
| Eudragit E PO/RS PO | 120–140 | Polymeric matrix | Metformin | Floating tubes | Sustained ** | [120] |
| Eudragit L100 | Polymeric matrix | Metropolol succinate | Extended release delivery system | <50% in 20 h | [48] | |
| Eudragit S100 | ||||||
| Eudragit L100/L100-55 | Polymeric matrix/Release modifier | <3% in 2 h in 0.1 N HCl, 100% in 24 h in pH 6.8 | ||||
| Eudragit S100/L100-55 (28.2% + 23.1%) | <3% in 2 h in 0.1 N HCl, ≅30% in 24 h in pH 6.8 | |||||
| Eudragit S100/L100-55 (23.1% + 28.2%) | <3% in 2 h in 0.1 N HCl, ≅70% in 24 h in pH 6.8 | |||||
| Eudragit S100/L100-55 (25.6% + 25.6%) | <3% in 2 h in 0.1 N HCl, ≅80% in 24 h in pH 6.8 | |||||
| Eudragit L100/P303 | <40% in 2 h in 0.1 N HCl, 100% in 11 h in pH 6.8 | |||||
| Eudragit S100/P303 | <40% in 2 h in 0.1 N HCl, 100% in 15 h in pH 6.8 | |||||
| Eudragit RL PO | 10–110 | Polymeric matrix | Theophylline | Floating pellet | * | [121] |
| Eudragit RS PO | Ranging between 24% to 96.2% in 18 h *** | |||||
| Eudragit RL PO | 140–150 | Polymeric matrix | Carbamazepine and theophylline | Extrudates | ≅85% in 8 h (10% Theo); ≅100% in 1 h (30% Theo); >90% in 12 h (10% CB); ≅90% in 8 h (30% CB) | [38] |
| Eudragit RS PO | ≅20% in 24 h (10% Theo); ≅70% in 12 h (30% Theo); ≅40% in 12 h (10% CB); ≅70% in 12 h (30% CB) | |||||
| Eudragit RL PO/RS PO (30:60) | ≅20% in 24 h (10% Theo); ≅80% in 12 h (10% CB) | |||||
| Eudragit RL PO/RS PO (45:45) | ≅20% in 24 h (10% Theo); > 90% in 12 h (10% CB) | |||||
| Eudragit RL PO/RS PO (60:30) | ≅50% in 12 h (10% Theo); >90% in 12 h (10% CB) | |||||
| Eudragit RL PO/RS PO (24:46) | >90% in 8 h (30% Theo); ≅75% in 12 h (30% CB) | |||||
| Eudragit RL PO/RS PO (35:35) | >90% in 4 h (30% Theo); ≅80% in 12 h (30% CB) | |||||
| Eudragit RL PO/RS PO (46:24) | >90% in 4 h (30% Theo); ≅85% in 12 h (30% CB) |
| Eudragit Type | Nozzle Temperature (°C) | Polymer Role | Drug | Pharmaceutical Form | Release Data $ | Reference |
|---|---|---|---|---|---|---|
| Eudragit E PO | 150 | Polymeric matrix | Felodipine | Disc | 84.3% in 30′ (HCl pH 1.2); 100% in 6 h (PBS pH 6.8) | [130] |
| 135 | Polymeric matrix | 5-ASA, theophylline, captopril and prednisolone | Tablet | 85% in 30′ | [131] | |
| 135 | Polymeric matrix | Sodium warfarin | Tablet | >80% in 45′ | [132] | |
| 230 | Polymeric matrix | Acetaminophen | * | ** | [133] | |
| 135 | Polymeric matrix | Hydrochlorothiazide | Tablet | 100% in 60′ | [134] | |
| 135 | Polymeric matrix | Enalapril maleate and hydrochlorothiazide | Tablet | 100% in 60′ | [135] | |
| 160–175 | Polymeric matrix | Pramipexole | Tablet | >90% in 60′ (EPO:Poliox N10); >90% in 90′ (EPO:Poliox N80, 50:50); >90% in 60′ (EPO:Poliox N80, 60:40); >90% in 25′ (EPO:Poliox N80, 70:30); | [136] | |
| 135–200 | Polymeric matrix | Carvedilol | Tablet | 80% in 11 h (Aff 15: EPO, 60:15) | [137] | |
| 200 | Taste-masking agent | Caffeine citrate | Donut shaped tablet | >80% in 60′ (10% infill); ≅75% in 120′ (50% infill); ≅50% in 120′ (100% infill) | [1] | |
| 160–165 | Polymeric matrix | Lumefantrine | Tablet | 90% in 30′ (65% infill); 78% in 30′ (80% infill); 69% in 30′ (100% infill) | [138] | |
| 200 | Polymeric matrix | Theophylline | Tablet | 85% in 50′ (10% drug); 85% in 30′ (30% drug); 85% in 48′ (60% drug) | [139] | |
| Eudragit FS30D | *** | Delaying release polymer | Theophylline | Printfill | 2.3% in 2 h (pH 1.2); 80% in 8 h (pH 7.5) | [140] |
| Eudragit L100 | 190 | Coating | Budesonide | Tablet | <5% in 2 h (0.1 N HCl); ≅45% in 5 h30′ (pH 5.6–7.4); ≅85% in 10 h (pH 6.5) | [141] |
| 200 | Polymeric matrix | Acetaminophen | Tablet | <10% in 24 h | [142] | |
| Eudragit L100-55 | 185 | Enteric polymer | Theophylline, budesonide and diclofenac | Tablet | 65% in 2 h in pH 1.2 and ≅100% in 150′ in pH 6.8 (0.17 mm shell); 75% in 2 h in pH 1.2 and ≅100% in 150′ in pH 6.8 (0.35 mm); <3% in 2 h in pH 1.2 and ≅100% in 360′ in pH 6.8 (0.52, 0.7 and 0.87 mm) | [143] |
| 167, 172 and 175 | Enteric polymer | Riboflavine-5′-phosphate | Capsule | 5% in 2 h in pH 1.2 and 87% in 45′ in pH 6.8 (layer height 100 μm); 5% in 2 h in pH 1.2 and 100% in 45′ in pH 6.8 (200 μm); 23% in 2 h in pH 1.2 and 100% in 45′ in pH 6.8 (300 μm) | [144] | |
| 178 | Polymeric matrix | Acetylsalicylic acid and simvastatin | Polypill | 0% (pH 1.2); 100% in 45′ (pH 6.8) | [145] | |
| Eudragit RL PO | 170 | Polymeric matrix | Metformin | Tablet | 100% in 8 h (single screw filament); 91.76% in 9 h (twin screw filament) | [146] |
| 180 | Polymeric matrix | Theophylline | Tablet | 85.93% in 2 h (ERL-PEG 10%); 10.66% in 2 h (ERL-SA 7%) | [147] | |
| 180 | Polymeric matrix | Theophylline | Tablet | >90% in 24 h (10%, 15%, 20%, 25% and 30% infill); 30% in 11 h (75% infill) | [148] | |
| 195 | Polymeric matrix | Theophylline | Caplet | 100% in 10 h (HPC:ERL:PEG:drug, 4:4:1:1); 100% in 4 h (HPC:ERL:PEG:drug, 5:3:1:1 and 6:2:1:1) | [34] | |
| 205–215 | Polymeric matrix | Indomethacin | * | ** | [149] | |
| Eudragit RL 100 | 170 | Polymeric matrix | Deflazacort | Tablet | ≅50% in 24 h (without mannitol); ≅70% in 24 h (mannitol); >80% in 24 h (mannitol and 50% infill) | [150] |
| Eudragit RS PO | 155 | Polymeric matrix | Quinine | Implant | 3.7% in 78 days | [151] |
| 180 | Polymeric matrix | Carvedilol | Floating tablet | Basket—≅90% in 24 h (C1); ≅65% in 24 h (C2); ≅60% in 24 h (C3 and C4); Paddle—≅95% in 24 h (C1); ≅65% in 24 h (C2); ≅70% in 24 h (C3); ≅60% in 24 h (C4); Tapped basket— ≅100% in 24 h (C1, C2, C3 and C4) | [152] | |
| 200 | Polymeric matrix | Quercetin | Patch | ≅9% in 70 h (drug:PVP40:ERS:TEC, 1:49:38:12); ≅7% in 24% (1:37:50:12); ≅12% in 24 h (1:25:62:12) | [153] | |
| 170 | Polymeric matrix | Octreotide | Capsule | No release in acid medium (0.1 M HCl); >80% in 30′ (PBS pH 6.8) | [154] | |
| Eudragit RS 100 | 160–180 | Polymeric matrix | Acetaminophen | Capsule | 85% in 8′ | [155] |
| Eudragit E | 140 | Polymeric matrix | Theophylline | Tablet | >90% above 40′ | [156] |
| Eudragit RL 100 | 170 | ≅80% in 18 h | ||||
| Eudragit RS 100 | 150 | ≅10% in 18 h | ||||
| Eudragit RL 100/RS 100 | 150 | ≅50% in 18 h | ||||
| Eudragit E PO | 175 | Polymeric matrix | Isoniazid | Tablet | 80% in 1000 min (EPO + HPC) | [157] |
| Eudragit L100 | 170 | 80% in 334′ (EL100 + HPC) | ||||
| Eudragit RL PO/RS PO | 165 | 100% in 200′ (ERS + ERL + PEO + TEC) | ||||
| Eudragit E PO | 135 | Polymeric matrix | Theophylline and dipyridamole | Capsule | >85% in 30′ | [158] |
| Eudragit RL | 170 | Theophylline | ≅50% in 2 h in pH 1.2 and ≅95% in 16 h in pH 6.8 (1.6 mm shell); ≅20% in 2 h in pH 1.2 and ≅ 75% in 16 h in pH 6.8 (2 mm); ≅10% in 2 h in pH 1.2 and ≅59% in 16 h in pH 6.8 (2.4 mm) | |||
| Eudragit RL PO | 178 | Release modifier | Ibuprofen | Tablet | ≅10% in 24 h | [159] |
| Eudragit RS PO | ≅7% in 24 h (20% ERS); ≅14% in 24 h (10% ERS) | |||||
| Eudragit L100-55/RL PO | 160 | Polymeric matrix | Furosemide | Disc | ** | [160] |
| Eudragit L100-55/S100 | 182 | Polymeric matrix | 5-Fluoracil | Tablet | L100-55:S100, 50:25 and 0:65—No release; 78:0—50% in 180′; 73:5—50% in 270′; 68:10—no release in SF pH 1.2 and SIF pH 6.5; In pH 7.4—40% in 120′ for both coated and non-coated; 100% (non-coated) and 80% (coated) in 9 h | [161] |
| Eudragit RL PO/RS PO | 200 | Coating | Allopurinol | Expandable gastroretentive devices | ≅100% in 300′ | [162] |
| Eudragit Type | Printing Tecnhique | °C Nozzle | Polymer Role | Drug | Pharmaceutical Form | Release Data $ | Reference |
|---|---|---|---|---|---|---|---|
| Eudragit E PO | Direct extrusion | 180 | Polymeric matrix | Dutasteride | Tablet | ≅100% in 40′ (tube); ≅100% in 120′ (pyramid); ≅80% in 120’ (cube); ≅70% in 120‘ (hemisphere) | [163] |
| Eudragit RL PO | Direct extrusion | 90 | Polymeric matrix | Ketoprofen and nicotine | Patch | 80% in 4 h (KP); 80% in 30′ (NT) | [164] |
| Eudragit RS PO | 20% in 4 h (KP); 60%, in 1 h (NT); | ||||||
| Eudragit RL PO/RS PO | 30% in 4 h (KP:ERL:ERS); 95%, in 1 h (NT:ERL:ERS) | ||||||
| Eudragit RL100 | Direct extrusion | 90 | Polymeric matrix | Theophylline | Tablet | ≅30% in 2 h in pH 1.2 and 80% in 12 h in pH 6.8 | [165] |
| Eudragit RS100 | 80 | ≅5% in 2 h in pH 1.2 and 25% in 12 h in pH 6.8 | |||||
| Eudragit RL100/RS100 | 95–110 | ≅25% in 2 h in pH 1.2 and 60% in 12 h in pH 6.8 (ERL:ERS, 75:25); ≅22% in 2 h in pH 1.2 and 55% in 12 h in pH 6.8 (ERL:ERS, 50:50); ≅15% in 2 h in pH 1.2 and 45% in 12 h in pH 6.8 (ERL:ERS, 25:75) | |||||
| Eudragit L100-55 | Selective laser sintering | - | Polymeric matrix | Acetaminophen | Printlet | 18% in 2 h; ≅60% in 6 h; ≅90% in 12 h (5% drug); 14% in 2 h; ≅60% in 6 h; ≅100% in 12 h (20% drug); 6% in 2 h; ≅60% in 6 h; ≅100% in 12 h (35% drug); | [166] |
| Eudragit L100-55 | Selective laser sintering | - | Polymeric matrix | Acetaminophen | Tablet | 17% in 2 h in HCl 0.1 M; and 100% in 12 h in pH 5.5 (cylindrical); 70% in 2 h (gyroid) | [167] |
| Eudragit RL | 95% in 24 h (cylindrical); 100% in 2 h (gyroid) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos, J.; da Silva, G.S.; Velho, M.C.; Beck, R.C.R. Eudragit®: A Versatile Family of Polymers for Hot Melt Extrusion and 3D Printing Processes in Pharmaceutics. Pharmaceutics 2021, 13, 1424. https://doi.org/10.3390/pharmaceutics13091424
dos Santos J, da Silva GS, Velho MC, Beck RCR. Eudragit®: A Versatile Family of Polymers for Hot Melt Extrusion and 3D Printing Processes in Pharmaceutics. Pharmaceutics. 2021; 13(9):1424. https://doi.org/10.3390/pharmaceutics13091424
Chicago/Turabian Styledos Santos, Juliana, Guilherme Silveira da Silva, Maiara Callegaro Velho, and Ruy Carlos Ruver Beck. 2021. "Eudragit®: A Versatile Family of Polymers for Hot Melt Extrusion and 3D Printing Processes in Pharmaceutics" Pharmaceutics 13, no. 9: 1424. https://doi.org/10.3390/pharmaceutics13091424