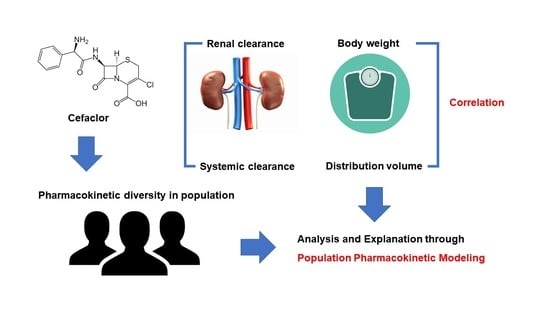
Population Pharmacokinetic Analysis of Cefaclor in Healthy Korean Subjects
Abstract
:1. Introduction
2. Subjects and Methods
2.1. Subjects
2.2. Sampling
2.3. Determination of Clinical Biochemistry Parameters
2.4. Determination of Plasma Cefaclor Concentrations
2.4.1. Chromatographic Conditions
2.4.2. Calibration Curve
2.4.3. Sample Preparation
2.4.4. Analytical Validation
2.5. Pharmacokinetic Analysis
2.6. Model Development
2.7. Model Evaluation
3. Results and Discussion
3.1. Study Design and Demographic Analysis
3.2. Determination of Plasma Cefaclor Concentrations
3.3. Pharmacokinetic Results by Non-Compartmental Analysis
3.4. Population Pharmacokinetic Model Analysis
CL/F = tvCL/F · ((CrCl/110.92) ^ dCL/FdCrCl) · exp(ŋCL/F)
Tlag = tvTlag
Ka = tvKa · exp(ŋKa)
3.5. Population Pharmacokinetic Model Evaluation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CrCl | Creatinine clearance |
| BSA | Body surface area |
| BMI | Body mass index |
| AST | Aspartate transaminase |
| ALP | Alkaline phosphatase |
| ALT | Alanine transaminase |
| HPLC | High–performance liquid chromatography |
| UV | Ultraviolet |
| SD | Standard deviation |
| NLME | Nonlinear mixed effects |
| AIC | Akaike’s information criterion |
| IIV | Inter–individual variability |
| OFV | Objective function value |
| SE | Standard error |
| RSE | Relative standard error |
References
- Arsalan, A.; Ahmad, I.; Ali, S.A. Cefaclor: Clinical, biochemical, analytical and stability aspects. Adv. Med. Biol. 2017, 123, 1–52. [Google Scholar]
- Takeuchi, O.; Hoshino, K.; Kawai, T.; Sanjo, H.; Takada, H.; Ogawa, T.; Takeda, K.; Akira, S. Differential Roles of TLR2 and TLR4 in Recognition of Gram-Negative and Gram-Positive Bacterial Cell Wall Components. Immunology 1999, 11, 443–451. [Google Scholar] [CrossRef] [Green Version]
- Paterson, D.L.; Doi, Y. Cefaclor, Cefprozil, and Loracarbef, Kucers the Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, 7th ed.; CRC Press: Boca Raton, FL, USA, 2017; pp. 376–382. [Google Scholar]
- Spyker, D.A.; Thomas, B.L.; Sande, M.A.; Bolton, W.K. Pharmacokinetics of Cefaclor and Cephalexin: Dosage Nomograms for Impaired Renal Function. Antimicrob. Agents Chemother. 1978, 14, 172–177. [Google Scholar] [CrossRef] [Green Version]
- Bloch, R.; Szwed, J.J.; Sloan, R.S.; Luft, F.C. Pharmacokinetics of Cefaclor in Normal Subjects and Patients with Chronic Renal Failure. Antimicrob. Agents Chemother. 1977, 12, 730–732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.H.; Huang, X.H.; Wang, K.; Li, J.; Zheng, Q.S. Population pharmacokinetics of cefaclor in healthy Chinese adult male volunteers. Chin. J. Clin. Pharmacol. Therapeut. 2012, 17, 659–665. [Google Scholar]
- Li, M.; Andrew, M.A.; Wang, J.; Salinger, D.H.; Vicini, P.; Grady, R.W.; Phillips, B.; Shen, D.D.; Anderson, G.D. Effects of Cranberry Juice on Pharmacokinetics of β-Lactam Antibiotics following Oral Administration. Antimicrob. Agents Chemother. 2009, 53, 2725–2732. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Han, E.; Lee, S.O.; Kim, D.-S. Antibiotic use in South Korea from 2007 to 2014: A health insurance database-generated time series analysis. PLoS ONE 2017, 12, e0177435. [Google Scholar] [CrossRef]
- El Edelbi, R.; Lindemalm, S.; Eksborg, S. Estimation of body surface area in various childhood ages–Validation of the Mosteller formula. Acta Paediatr. 2012, 101, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Hotta, M.; Li, Y.; Anme, T.; Ushijima, H. Risk factors for low Kaup index among children in rural ethnic minority areas of Yunnan, China. Pediatr. Int. 2005, 47, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Hermsen, E.D.; Maiefski, M.; Florescu, M.C.; Qiu, F.; Rupp, M.E.; Maiefski, M.M. Comparison of the Modification of Diet in Renal Disease and Cockcroft-Gault Equations for Dosing Antimicrobials. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2009, 29, 649–655. [Google Scholar] [CrossRef]
- Cho, H.Y.; Kang, H.A.; Kim, S.M.; Park, C.H.; Oh, I.J.; Lim, D.K.; Moon, J.-D.; Lee, Y.B. Bioequivalence of Kyongbocefaclor Capsule to Ceclor Capsule (Cefaclor 250 mg). J. Pharm. Investig. 2005, 35, 39–44. [Google Scholar]
- Jang, J.-H.; Jeong, S.-H.; Cho, H.-Y.; Lee, Y.-B. Population Pharmacokinetics of Cis-, Trans-, and Total Cefprozil in Healthy Male Koreans. Pharmaceutics 2019, 11, 531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeong, S.-H.; Jang, J.-H.; Cho, H.-Y.; Lee, Y.-B. Population Pharmacokinetic Analysis of Tiropramide in Healthy Korean Subjects. Pharmaceutics 2020, 12, 374. [Google Scholar] [CrossRef] [PubMed]
- Yun, M.H.; Kim, H.S.; Choi, Y.P.; Kwon, K.I. Bioequivalence of Cefaclor (250 mg) Capsule. Korean J. Clin. Pharm. 2002, 12, 71–75. [Google Scholar]
- Chun, S.K.; Nam, K.W.; Rew, J.H.; Kim, N.J.; Song, B.W.; Seo, S.H.; Lee, K. Bioequivalence Test of Dae Won WonclorR (Cefaclor 250mg) to CeclorR Capsules. J. Korean Soc. Health Syst. 2002, 19, 166–171. [Google Scholar]
- Kim, T.W.; Cao, Q.R.; Han, S.Y.; Song, O.K.; Sin, K.S.; Kang, S.H.; Lee, B.J. Bioequivalence of Cefaclor Monohydrate 250mg Capsules Using an Improved HPLC Analytical Method. Korean J. Clin. Pharm. 2005, 15, 21–26. [Google Scholar]
- Lode, H.; Stahlmann, R.; Koeppe, P. Comparative Pharmacokinetics of Cephalexin, Cefaclor, Cefadroxil, and CGP 9000. Antimicrob. Agents Chemother. 1979, 16, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Welling, P.G.; Dean, S.; Selen, A.; Kendall, M.J.; Wise, R. The pharmacokinetics of the oral cephalosporins cefaclor, cephradine and cephalexin. Int. J. Clin. Pharmacol. Biopharm. 1979, 17, 397–400. [Google Scholar]
- Barbhaiya, R.H.; Shukla, U.A.; Gleason, C.R.; Shyu, W.C.; Wilber, R.B.; Pittman, K.A. Comparison of cefprozil and cefaclor pharmacokinetics and tissue penetration. Antimicrob. Agents Chemother. 1990, 34, 1204–1209. [Google Scholar] [CrossRef] [Green Version]
- Barbhaiya, R.H.; Shukla, U.A.; Gleason, C.R.; Shyu, W.C.; Pittman, K.A. Comparison of the effects of food on the pharmacokinetics of cefprozil and cefaclor. Antimicrob. Agents Chemother. 1990, 34, 1210–1213. [Google Scholar] [CrossRef] [Green Version]
- Barbhaiya, R.H.; Shukla, U.A.; Gleason, C.R.; Shyu, W.C.; Wilber, R.B.; Martin, R.R.; Pittman, K.A. Phase I study of multiple-dose cefprozil and comparison with cefaclor. Antimicrob. Agents Chemother. 1990, 34, 1198–1203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- E Nix, D.; Symonds, W.T.; Hyatt, J.M.; Wilton, J.H.; Teal, M.A.; Reidenberg, P.; Affrime, M.B. Comparative pharmacokinetics of oral ceftibuten, cefixime, cefaclor, and cefuroxime axetil in healthy volunteers. Pharmacother. J. Hum. Pharmacol. Drug Ther. 1997, 17, 121–125. [Google Scholar]
- Granados-Soto, V.; Aguilar-Cota, M.E.; Reyes-Garcia, G.; Medina-Santillán, R.; Flores-Murrieta, F.J. Simple method for the deter-mination of cefaclor in human plasma samples by HPLC. J. Liq. Chromatogr. Relat. Technol. 2003, 26, 3315–3323. [Google Scholar] [CrossRef]
- Sourgens, H.; Derendorf, H.; Schifferer, H. Pharmacokinetic profile of cefaclor. Int. J. Clin. Pharmacol. Ther. 1997, 35, 374–380. [Google Scholar]
- Oguma, T.; Yamada, H.; Sawaki, M.; Narita, N. Pharmacokinetic analysis of the effects of different foods on absorption of cefaclor. Antimicrob. Agents Chemother. 1991, 35, 1729–1735. [Google Scholar] [CrossRef] [Green Version]
- Hanley, M.J.; Abernethy, D.R.; Greenblatt, D.J. Effect of Obesity on the Pharmacokinetics of Drugs in Humans. Clin. Pharmacokinet. 2010, 49, 71–87. [Google Scholar] [CrossRef]
- Li, M.; Anderson, G.D.; Phillips, B.R.; Kong, W.; Shen, D.D.; Wang, J. Interactions of Amoxicillin and Cefaclor with Human Renal Organic Anion and Peptide Transporters. Drug Metab. Dispos. 2006, 34, 547–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Physicochemical Parameters | Units | Median (Range) | Mean ± SD |
|---|---|---|---|
| Age | Year | 23 (19–26) | 23.00 ± 1.44 |
| Weight | kg | 66.05 (50.00–88.70) | 67.31 ± 8.46 |
| Height | cm | 172.0 (164.00–187.30) | 173.31 ± 6.22 |
| BSA * | m2 | 1.78 (1.51–2.10) | 1.80 ± 0.13 |
| BMI ** | kg/m2 | 21.78 (17.70–28.44) | 22.40 ± 2.44 |
| Albumin | g/dL | 4.90 (4.40–5.40) | 4.85 ± 0.23 |
| Total proteins | g/dL | 7.40 (6.70–8.20) | 7.38 ± 0.34 |
| BUN | mg/dL | 12.00 (7.70–21.80) | 12.54 ± 3.39 |
| Total bilirubin | mg/dL | 1.00 (0.51–2.11) | 1.04 ± 0.34 |
| Cholesterol | mg/dL | 158 (118–231) | 163.52 ± 29.70 |
| ALT | U/L | 15.00 (7.00–41.00) | 16.42 ± 6.70 |
| AST | U/L | 17.00 (6.00–28.00) | 17.29 ± 3.96 |
| ALP | U/L | 74.00 (44.00–105.00) | 73.92 ± 16.77 |
| Creatinine | mg/dL | 1.00 (0.70–1.30) | 0.97 ± 0.12 |
| CrCl *** | mL/min | 110.92 (67.50–170.42) | 114.97 ± 20.86 |
| Parameters | Units | Estimates |
|---|---|---|
| AUC0–t | h·µg/mL | 9.64 ± 2.40 |
| AUC0–∞ | h·µg/mL | 9.83 ± 2.41 |
| CL/F | mL/h | 27,188.46 ± 7771.88 |
| Cmax | μg/mL | 7.87 ± 2.20 |
| T1/2 | h | 0.68 ± 0.15 |
| Tmax | h | 0.80 ± 0.28 |
| V/F | mL | 26,116.39 ± 7820.88 |
| Model | Description | n–Parameter | −2LL | AIC | Δ−2LL | ΔAIC | Compared with |
|---|---|---|---|---|---|---|---|
| Absorption model | |||||||
| 01 | 1–compartment with first order (without Tlag) | 7 | 1626.01 | 1640.01 | − | − | − |
| 02 * | 1–compartment with first order (with Tlag) | 9 | 1019.51 | 1037.51 | −606.50 | −602.50 | 01 |
| Residual error model | |||||||
| 02 | Additive | 9 | 1019.51 | 1037.51 | 0 | 0 | 02 |
| 02–01 * | Proportional | 9 | 882.99 | 900.99 | −136.52 | −136.52 | 02 |
| 02–02 | Power | 9 | 1109.68 | 1127.68 | 90.17 | 90.17 | 02 |
| 02–03 | Mixed | 10 | 1493.82 | 1511.82 | 474.31 | 474.31 | 02 |
| 02–04 | Log additive | 9 | 1493.82 | 1511.82 | 474.31 | 474.31 | 02 |
| IIV model | |||||||
| 02–01–01 | Remove IIV V/F | 8 | 1772.84 | 1788.84 | 889.85 | 887.85 | 02–01 |
| 02–01–02 | Remove IIV CL/F | 8 | 1092.38 | 1108.38 | 209.39 | 207.39 | 02–01 |
| 02–01–03 | Remove IIV Ka | 8 | 1570.07 | 1586.07 | 687.08 | 685.08 | 02–01 |
| 02–01–04 * | Remove IIV Tlag | 8 | 859.92 | 875.92 | −23.07 | −25.07 | 02–01 |
| 02–01–05 | Remove IIV Tlag and CL/F | 7 | 1076.22 | 1090.22 | 193.23 | 189.23 | 02–01 |
| Model | Description | OFV | ΔOFV | n–Parameter | Compared with |
|---|---|---|---|---|---|
| 01 | Base model | 859.918 | − | 8 | − |
| 02 | Weight on CL/F | 857.838 | −2.080 | 9 | 01 |
| 03 | BSA on CL/F | 857.163 | −2.755 | 9 | 01 |
| 04 | BMI on V/F | 857.087 | −2.831 | 9 | 01 |
| 05 | Weight on V/F | 855.211 | −4.707 | 9 | 01 |
| 06 | CrCl on CL/F | 855.157 | −4.761 | 9 | 01 |
| 07 | CrCl and BSA on CL/F | 855.276 | 0.119 | 10 | 06 |
| 08 * | CrCl on CL/F and weight on V/F | 848.495 | −6.662 | 10 | 06 |
| Parameters | Units | Estimate | SE | RSE (%) | Shrinkage (%) | IIV (%) |
|---|---|---|---|---|---|---|
| tvV/F | mL | 22,593.260 | 790.037 | 3.50 | − | − |
| tvCL/F | mL/h | 27,166.883 | 981.584 | 3.61 | − | − |
| tvTlag | h | 0.245 | 0.001 | 0.60 | − | − |
| tvKa | 1/h | 5.203 | 0.938 | 18.02 | − | − |
| dCL/FdCrCl | − | 0.436 | 0.184 | 42.21 | − | − |
| dV/FdWeight | − | 0.581 | 0.183 | 31.54 | − | − |
| ω2V/F | − | 0.011 | 0.005 | 51.90 | 0.384 | 10.250 |
| ω2CL/F | − | 0.034 | 0.010 | 30.22 | 0.069 | 18.388 |
| ω2Ka | − | 0.971 | 0.297 | 30.55 | 0.079 | 98.534 |
| σ | − | 0.270 | 0.023 | 8.56 | − | − |
| Parameters | Units | Final Model | Bootstrapping | ||
|---|---|---|---|---|---|
| Estimate | 95% Confidence Interval | Median | 95% Confidence Interval | ||
| tvV/F | mL | 22,593.260 | 21,040.330–24,146.190 | 22,571.198 | 20,976.447–24,091.153 |
| tvCL/F | mL/h | 27,166.883 | 25,237.440–29,096.327 | 26,952.524 | 25,315.334–29,579.444 |
| tvTlag | h | 0.245 | 0.242–0.248 | 0.245 | 0.240–0.247 |
| tvKa | 1/h | 5.203 | 3.360–7.046 | 5.198 | 3.806–10.828 |
| dCL/FdCrCl | − | 0.436 | 0.074–0.798 | 0.436 | 0.125–0.870 |
| dV/FdWeight | − | 0.581 | 0.221–0.941 | 0.581 | 0.248–0.920 |
| ω2V/F | − | 0.011 | 0.000–0.021 | 0.009 | 0.000–0.023 |
| ω2CL/F | − | 0.034 | 0.014–0.054 | 0.031 | 0.010–0.052 |
| ω2Ka | − | 0.971 | 0.390–1.552 | 0.962 | 0.369–1.555 |
| σ | − | 0.270 | 0.225–0.316 | 0.268 | 0.215–0.311 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, S.-H.; Jang, J.-H.; Cho, H.-Y.; Lee, Y.-B. Population Pharmacokinetic Analysis of Cefaclor in Healthy Korean Subjects. Pharmaceutics 2021, 13, 754. https://doi.org/10.3390/pharmaceutics13050754
Jeong S-H, Jang J-H, Cho H-Y, Lee Y-B. Population Pharmacokinetic Analysis of Cefaclor in Healthy Korean Subjects. Pharmaceutics. 2021; 13(5):754. https://doi.org/10.3390/pharmaceutics13050754
Chicago/Turabian StyleJeong, Seung-Hyun, Ji-Hun Jang, Hea-Young Cho, and Yong-Bok Lee. 2021. "Population Pharmacokinetic Analysis of Cefaclor in Healthy Korean Subjects" Pharmaceutics 13, no. 5: 754. https://doi.org/10.3390/pharmaceutics13050754