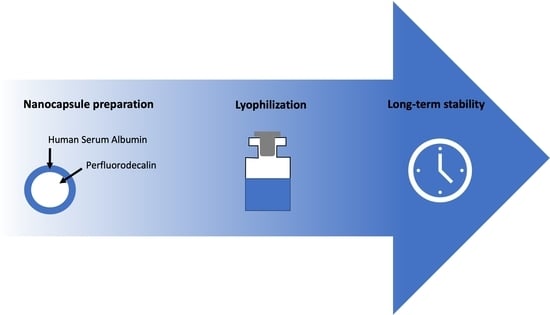
Development of a Lyophilization Process for Long-Term Storage of Albumin-Based Perfluorodecalin-Filled Artificial Oxygen Carriers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Nanocapsule Preparation
2.3. Determination of Nanocapsule Diameter and Stability
2.4. Glass Transition Temperature
2.5. Freeze–Thaw Cycles
2.6. Lyophilization
2.7. Long-Term Storage of the Lyophilized Product
2.8. Determination of the Residual Moisture
2.9. Oxygen Capacity
2.10. Statistical Methods
2.10.1. Design of Experiments (DoE)
2.10.2. Mean Values and Standard Deviation
3. Results
3.1. Nanocapsule Preparation, Characterization, and Stability
3.2. Freeze-Thaw Cycles
3.3. Glass Transition Temperature
3.4. Development of a Lyophilization Process
3.4.1. Basic Lyophilization Process
3.4.2. Design of Experiments—Shelf Temperature, Trehalose Content, and Volume of Nanocapsule Suspension
3.4.3. Adjustment of Trehalose Content and Volume of Nanocapsule Suspension
3.5. Long-Term Storage of the Lyophilized Product
3.6. Increase of the Vial Filling Volume
3.7. Oxygen Capacity
4. Discussion
4.1. Nanocapsule Preparation, Characterization, and Stability
4.2. Freeze–Thaw Cycles
4.3. Glass Transition Temperature
4.4. Development of the Lyophilization Process
4.4.1. Design of Experiments—Shelf Temperature, Trehalose Content, and Volume of the Nanocapsule Suspension
4.4.2. Adjustment of the Trehalose Content and the Nanocapsule Suspension Volume
4.5. Long-Term Storage of the Lyophilized Product
4.6. Increase of the Batch Volume
4.7. Oxygen Capacity
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chandler, T.; Hiller, J.; Peine, S.; Stargardt, T. Blood donation and donors: Insights from a large German teaching hospital (2008–2017). Vox Sang. 2020, 115, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Goodnough, L.T.; Panigrahi, A.K. Blood transfusion therapy. Med. Clin. N. Am. 2017, 101, 431–447. [Google Scholar] [CrossRef] [PubMed]
- Ferenz, K.B.; Steinbicker, A.U. Artificial oxygen carriers—Past, present, and future—A review of the most innovative and clinically relevant concepts. J. Pharmacol. Exp. Ther. 2019, 369, 300–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambert, E.; Janjic, J.M. Quality by design approach identifies critical parameters driving oxygen delivery performance in vitro for perfluorocarbon based artificial oxygen carriers. Sci. Rep. 2021, 11, 5569. [Google Scholar] [CrossRef] [PubMed]
- He, X.M.; Carter, D.C. Atomic structure and chemistry of human serum albumin. Nature 1993, 364, 362. [Google Scholar] [CrossRef] [Green Version]
- Elzoghby, A.O.; Samy, W.M.; Elgindy, N.A. Albumin-based nanoparticles as potential controlled release drug delivery systems. J. Control. Release 2012, 157, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Damascelli, B.; Cantù, G.; Mattavelli, F.; Tamplenizza, P.; Bidoli, P.; Leo, E.; Dosio, F.; Cerrotta, A.M.; Di Tolla, G.; Frigerio, L.F.; et al. Intraarterial chemotherapy with polyoxyethylated castor oil free paclitaxel, incorporated in albumin nanoparticles (ABI-007). Cancer 2001, 92, 2592–2602. [Google Scholar] [CrossRef] [Green Version]
- Kundranda, M.N.; Niu, J. Albumin-bound paclitaxel in solid tumors: Clinical development and future directions. Drug Des. Dev. Ther. 2015, 9, 3767–3777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riess, J.G. Understanding the fundamentals of perfluorocarbons and perfluorocarbon emulsions relevant to in vivo oxygen delivery. Artif. Cells Blood Substit. Immobil. Biotechnol. 2005, 33, 47–63. [Google Scholar] [CrossRef]
- Jägers, J.; Wrobeln, A.; Ferenz, K.B. Perfluorocarbon-based oxygen carriers: From physics to physiology. Pflug. Arch. 2021, 473, 139–150. [Google Scholar] [CrossRef] [PubMed]
- LoNostro, P.; Choi, S.-M.; Ku, C.-Y.; Chen, S.-H. Fluorinated microemulsions: A study of the phase behavior and structure. J. Phys. Chem. B 1999, 103, 5347–5352. [Google Scholar] [CrossRef]
- Lowe, K.C. Blood substitutes: From chemistry to clinic. J. Mater. Chem. 2006, 16, 4189–4196. [Google Scholar] [CrossRef]
- Wrobeln, A.; Laudien, J.; Groß-Heitfeld, C.; Linders, J.; Mayer, C.; Wilde, B.; Knoll, T.; Naglav, D.; Kirsch, M.; Ferenz, K.B. Albumin-derived perfluorocarbon-based artificial oxygen carriers: A physico-chemical characterization and first in vivo evaluation of biocompatibility. Eur. J. Pharm. Biopharm. 2017, 115, 52–64. [Google Scholar] [CrossRef]
- Wrobeln, A.; Schlüter, K.D.; Linders, J.; Zähres, M.; Mayer, C.; Kirsch, M.; Ferenz, K.B. Functionality of albumin-derived perfluorocarbon-based artificial oxygen carriers in the Langendorff-heart. Artif. Cells Nanomed. Biotechnol. 2017, 45, 723–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wrobeln, A.; Jägers, J.; Quinting, T.; Schreiber, T.; Kirsch, M.; Fandrey, J.; Ferenz, K.B. Albumin-derived perfluorocarbon-based artificial oxygen carriers can avoid hypoxic tissue damage in massive hemodilution. Sci. Rep. 2020, 10, 11950. [Google Scholar] [CrossRef]
- Kratz, F. Albumin as a drug carrier: Design of prodrugs, drug conjugates and nanoparticles. J. Control. Release 2008, 132, 171–183. [Google Scholar] [CrossRef]
- Lambert, E.; Gorantla, V.S.; Janjic, J.M. Pharmaceutical design and development of perfluorocarbon nanocolloids for oxygen delivery in regenerative medicine. Nanomedicine 2019, 14, 2697–2712. [Google Scholar] [CrossRef] [PubMed]
- Abdelwahed, W.; Degobert, G.; Stainmesse, S.; Fessi, H. Freeze-drying of Nanoparticles: Formulation, Process and Storage Considerations. Adv. Drug Deliv. Rev. 2006, 58, 1688–1713. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Wang, Z.; Zhou, Y.T.; Grayburn, P.A. Optimization of the size distribution and myocardial contrast effect of perfluorocarbon-filled albumin microbubbles by lyophilization under continuous negative pressure. J. Am. Soc. Echocardiogr. 2000, 13, 748–753. [Google Scholar] [CrossRef]
- Pisani, E.; Tsapis, N.; Paris, J.; Nicolas, V.; Cattel, L.; Fattal, E. Polymeric nano/microcapsules of liquid perfluorocarbons for ultrasonic imaging: Physical characterization. Langmuir 2006, 22, 4397–4402. [Google Scholar] [CrossRef]
- Ball, P.A. Intravenous in-line filters: Filtering the evidence. Curr. Opin. Clin. Nutr. Metab. Care 2003, 6, 319–325. [Google Scholar] [CrossRef]
- Wiedeman, M.P. Dimensions of blood vessels from distributing artery to collecting vein. Circ. Res. 1963, 12, 375–378. [Google Scholar] [CrossRef] [Green Version]
- Franks, F. Freeze-drying of bioproducts: Putting principles into practice. Eur. J. Pharm. Biopharm. 1998, 45, 221–229. [Google Scholar] [CrossRef]
- Anhorn, M.G.; Mahler, H.-C.; Langer, K. Freeze-drying of human serum albumin (HSA) nanoparticles with different excipients. Int. J. Pharm. 2008, 363, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, W.H.; Fernandes, P.M.; Taforo, T. Formulation for Lipophilic IL-2 Proteins. U.S. Patent 4992271, 12 February 1991. [Google Scholar]
- Hawe, A.; Friess, W. Physicochemical characterization of the freezing behavior of mannitol-human serum albumin formulations. AAPS PharmSciTech 2006, 7, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Crowe, L.M.; Reid, D.S.; Crowe John, H. Is trehalose special for preserving dry biomaterials? Biophys. J. 1996, 71, 2087–2093. [Google Scholar] [CrossRef] [Green Version]
- Wang, W. Lyophilization and development of solid protein pharmaceuticals. Int. J. Pharm. 2000, 203, 1–60. [Google Scholar] [CrossRef]
- Meister, E.; Gieseler, H. Freeze-dry microscopy of protein/sugar mixtures: Drying behavior, interpretation of collapse temperatures and a comparison to corresponding glass transition data. J. Pharm. Sci. 2009, 98, 3072–3087. [Google Scholar] [CrossRef]
- Anderski, J.; Mahlert, L.; Sun, J.; Birnbaum, W.; Mulac, D.; Schreiber, S.; Herrmann, F.; Kuckling, D.; Langer, K. Light-responsive nanoparticles based on new polycarbonate polymers as innovative drug delivery systems for photosensitizers in PDT. Int. J. Pharm. 2019, 557, 182–191. [Google Scholar] [CrossRef]
- Pikal, M.J.; Shah, S. The collapse temperature in freeze drying: Dependence on measurement methodology and rate of water removal from the glassy phase. Int. J. Pharm. 1990, 62, 165–186. [Google Scholar] [CrossRef]
- Tang, X.; Pikal, M.J. Design of freeze-drying processes for pharmaceuticals: Practical advice. Pharm. Res. 2004, 21, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Kasper, J.C.; Winter, G.; Friess, W. Recent advances and further challenges in lyophilization. Eur. J. Pharm. Biopharm. 2013, 85, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Chung, N.-O.; Lee, M.K.; Lee, J. Mechanism of freeze-drying drug nanosuspensions. Int. J. Pharm. 2012, 437, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, R.L. Red blood cell storage and transfusion-related immunomodulation. Blood Transfus. 2010, 8, 26–30. [Google Scholar] [CrossRef]
- Wang, D.; Sun, J.; Solomon, S.B.; Klein, H.G.; Natanson, C. Transfusion of older stored blood and risk of death: A meta-analysis. Transfusion 2012, 52, 1184–1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Sample Number | Volume Nanocapsule Suspension [µL] | Volume Purified Water [µL] | Trehalose Content [mg/mL] |
|---|---|---|---|
| 1 | 100 | 900 | 30 to 150 |
| 2 | 333 | 667 | 60 |
| 3 | 500 | 500 | 60 |
| 4 | 750 | 250 | 60 |
| 5 | 1000 | 0 | 30 to 100 |
| 6 | 2500 | 0 | 60 |
| Lyophilization Step | Time [h:min] | Temperature [°C] | Pressure [mbar] |
|---|---|---|---|
| Freezing | 00:15 | 10 to −40 | Atm |
| Freezing | 00:30 | −40 | Atm |
| Primary drying | 00:01 | −40 to −34 | 0.05 |
| Primary drying | 14:00 | −34 | 0.05 |
| Secondary drying | 00:15 | −34 | 0.025 |
| Secondary drying | 00:15 | −34 to 0 | 0.025 |
| Secondary drying | 01:00 | 0 to 20 | 0.025 |
| Secondary drying | 05:00 | 20 | 0.025 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hester, S.; Ferenz, K.B.; Eitner, S.; Langer, K. Development of a Lyophilization Process for Long-Term Storage of Albumin-Based Perfluorodecalin-Filled Artificial Oxygen Carriers. Pharmaceutics 2021, 13, 584. https://doi.org/10.3390/pharmaceutics13040584
Hester S, Ferenz KB, Eitner S, Langer K. Development of a Lyophilization Process for Long-Term Storage of Albumin-Based Perfluorodecalin-Filled Artificial Oxygen Carriers. Pharmaceutics. 2021; 13(4):584. https://doi.org/10.3390/pharmaceutics13040584
Chicago/Turabian StyleHester, Sarah, Katja Bettina Ferenz, Susanne Eitner, and Klaus Langer. 2021. "Development of a Lyophilization Process for Long-Term Storage of Albumin-Based Perfluorodecalin-Filled Artificial Oxygen Carriers" Pharmaceutics 13, no. 4: 584. https://doi.org/10.3390/pharmaceutics13040584