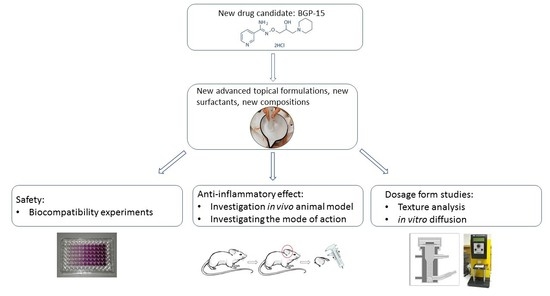
Nicotinic Amidoxime Derivate BGP-15, Topical Dosage Formulation and Anti-Inflammatory Effect
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Animals
2.3. Formulation of Ointments
2.4. Texture Analyzing Studies
2.5. In Vitro Release
2.6. Biocompatibility Experiments
2.7. Inflammation Model Induced by Allyl-Isothiocyanate (AITC)
2.8. Antioxidant Assay-Superoxide Dismutase (SOD) Assay
2.9. Total Antioxidant Capacity (TAC)
2.10. Luciferase Assay
2.11. Statistical Analysis
3. Results
3.1. Texture Analyzing Studies
3.2. In Vitro Release
3.3. MTT Assay
3.4. AITC Induced Inflammation Model
3.5. Antioxidant Assay-Superoxide Dismutase (SOD) Assay
3.6. Total Antioxidant Capacity
3.7. Luciferase Assay
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Literáti-Nagy, B.; Kulcsár, E.; Literáti-Nagy, Z.; Buday, B.; Péterfai, E.; Horváth, T.; Tory, K.; Kolonics, A.; Fleming, A.; Mandl, J.; et al. Improvement of insulin sensitivity by a novel drug, BGP-15, in insulin-resistant patients: A proof of concept randomized double-blind clinical trial. Horm. Metab. Res. 2009, 41, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Bárdos, G.; Móricz, K.; Jaszlits, L.; Rabloczky, G.; Tory, K.; Rácz, I.; Bernáth, S.; Sümegi, B.; Farkas, B.; Literáti-Nagy, B.; et al. BGP-15, a hydroximic acid derivative, protects against cisplatin- or taxol-induced peripheral neuropathy in rats. Toxicol. Appl. Pharmacol. 2003, 190, 9–16. [Google Scholar] [CrossRef]
- Racz, I.; Tory, K.; Gallyas, F.; Berente, Z.; Osz, E.; Jaszlits, L.; Bernath, S.; Sumegi, B.; Rabloczky, G.; Literati-Nagy, P. BGP-15—A novel poly(ADP-ribose) polymerase inhibitor—Protects against nephrotoxicity of cisplatin without compromising its antitumor activity. Biochem. Pharmacol. 2002, 63, 1099–1111. [Google Scholar] [CrossRef]
- Lampé, N.; Priksz, D.; Erdei, T.; Bombicz, M.; Kiss, R.; Varga, B.; Zsuga, J.; Szerafin, T.; Csanádi, Z.; Balla, G.; et al. Negative Inotropic Effect of BGP-15 on the Human Right Atrial Myocardium. J. Clin. Med. 2020, 9, 1434. [Google Scholar] [CrossRef]
- Sarszegi, Z.; Bognar, E.; Gaszner, B.; Kónyi, A.; Gallyas, F.; Sumegi, B.; Berente, Z. BGP-15, a PARP-inhibitor, prevents imatinib-induced cardiotoxicity by activating Akt and suppressing JNK and p38 MAP kinases. Mol. Cell. Biochem. 2012, 365, 129–137. [Google Scholar] [CrossRef]
- Chung, J.; Nguyen, A.K.; Henstridge, D.C.; Holmes, A.G.; Chan, M.H.S.; Mesa, J.L.; Lancaster, G.I.; Southgate, R.J.; Bruce, C.R.; Duffy, S.J.; et al. HSP72 protects against obesity-induced insulin resistance. Proc. Natl. Acad. Sci. USA 2008, 105, 1739–1744. [Google Scholar] [CrossRef] [Green Version]
- Literáti-Nagy, B.; Tory, K.; Peitl, B.; Bajza, Á.; Korányi, L.; Literáti-Nagy, Z.; Hooper, P.L.; Vígh, L.; Szilvássy, Z. Improvement of insulin sensitivity by a novel drug candidate, BGP-15, in different animal studies. Metab. Syndr. Relat. Disord. 2014, 12, 125–131. [Google Scholar] [CrossRef] [Green Version]
- Literáti-Nagy, B.; Péterfai, É.; Kulcsár, E.; Literáti-Nagy, Z.; Buday, B.; Tory, K.; Mandl, J.; Sümegi, B.; Fleming, A.; Roth, J.; et al. Beneficial effect of the insulin sensitizer (HSP inducer) BGP-15 on olanzapine-induced metabolic disorders. Brain Res. Bull. 2010, 83, 340–344. [Google Scholar] [CrossRef]
- Literati-Nagy, Z.; Tory, K.; Literáti-Nagy, B.; Bajza, Á.; Vígh, L.; Vígh, L.; Mandl, J.; Szilvássy, Z. Synergetic insulin sensitizing effect of rimonabant and BGP-15 in zucker-obes rats. Pathol. Oncol. Res. 2013, 19, 571–575. [Google Scholar] [CrossRef]
- Brykczynska, U.; Geigges, M.; Wiedemann, S.J.; Dror, E.; Böni-Schnetzler, M.; Hess, C.; Donath, M.Y.; Paro, R. Distinct Transcriptional Responses across Tissue-Resident Macrophages to Short-Term and Long-Term Metabolic Challenge. Cell Rep. 2020, 30, 1627–1643.e7. [Google Scholar] [CrossRef]
- Pető, Á.; Kósa, D.; Fehér, P.; Ujhelyi, Z.; Sinka, D.; Vecsernyés, M.; Szilvássy, Z.; Juhász, B.; Csanádi, Z.; Vígh, L.; et al. Pharmacological overview of the BGP-15 chemical agent as a new drug candidate for the treatment of symptoms of metabolic syndrome. Molecules 2020, 25, 429. [Google Scholar] [CrossRef] [Green Version]
- Farkas, B.; Magyarlaki, M.; Csete, B.; Nemeth, J.; Rabloczky, G.; Bernath, S.; Literáti Nagy, P.; Sümegi, B. Reduction of acute photodamage in skin by topical application of a novel PARP inhibitor. Biochem. Pharmacol. 2002, 63, 921–932. [Google Scholar] [CrossRef]
- Roohnikan, M.; Laszlo, E.; Babity, S.; Brambilla, D. A snapshot of transdermal and topical drug delivery research in Canada. Pharmaceutics 2019, 11, 256. [Google Scholar] [CrossRef]
- Jain, K.K. An Overview of Drug Delivery Systems. In Drug Delivery Systems; Humana: New York, NY, USA, 2020; Volume 2059, pp. 1–54. ISBN 9781493997985. [Google Scholar]
- Som, I.; Bhatia, K.; Yasir, M. Status of surfactants as penetration enhancers in transdermal drug delivery. J. Pharm. Bioallied Sci. 2012, 4, 2–9. [Google Scholar] [CrossRef]
- Arellano, A.; Santoyo, S.; Martın, C.; Ygartuá, P. Influence of Propylene Glycol and Isopropyl Myristate on the in vitro Percutaneous Penetration of Diclofenac Sodium from Carbopol Gels. Eur. J. Pharm. Sci. 1999, 7, 129–135. [Google Scholar] [CrossRef]
- Csizmazia, E.; Eros, G.; Berkesi, O.; Berkó, S.; Szabó-Révész, P.; Csányi, E. Penetration enhancer effect of sucrose laurate and Transcutol on ibuprofen. J. Drug Deliv. Sci. Technol. 2011, 21, 411–415. [Google Scholar] [CrossRef]
- Srirod, S.; Tewtrakul, S. Anti-inflammatory and wound healing effects of cream containing Curcuma mangga extract. J. Ethnopharmacol. 2019, 238, 111828. [Google Scholar] [CrossRef]
- D’Arpino, S.; Corbrion-Archer, V.; Marty, J.P.; Lantieri, L.; Vincent, C.M.; Astier, A.; Paul, M. Influence of vehicles on the in vitro percutaneous absorption of piroxicam to optimise the formulation of patch tests in dermatology. Drug Dev. Res. 2003, 58, 283–290. [Google Scholar] [CrossRef]
- Karataş, A.; Yüksel, N.; Baykara, T. Improved solubility and dissolution rate of piroxicam using gelucire 44/14 and labrasol. Farmaco 2005, 60, 777–782. [Google Scholar] [CrossRef]
- Fehér, P.; Ujhelyi, Z.; Váradi, J.; Fenyvesi, F.; Róka, E.; Juhász, B.; Varga, B.; Bombicz, M.; Priksz, D.; Bácskay, I.; et al. Efficacy of pre- and post-treatment by topical formulations containing dissolved and suspended Silybum marianum against UVB-induced oxidative stress in guinea pig and on HaCaT keratinocytes. Molecules 2016, 21, 1269. [Google Scholar] [CrossRef] [Green Version]
- Józsa, L.; Ujhelyi, Z.; Vasvári, G.; Sinka, D.; Nemes, D.; Fenyvesi, F.; Váradi, J.; Vecsernyés, M.; Szabó, J.; Kalló, G.; et al. Formulation of creams containing spirulina platensis powder with different nonionic surfactants for the treatment of acne vulgaris. Molecules 2020, 25, 4856. [Google Scholar] [CrossRef]
- Suarato, G.; Spanò, R.; Bertorelli, R.; Diaspro, A.; Athanassiou, A.; Surdo, S. 3D-Printed, Pocket-Size Diffusion Cells for Skin Permeation Investigation. Proceedings 2018, 2, 945. [Google Scholar] [CrossRef] [Green Version]
- Samaha, D.; Shehayeb, R.; Kyriacos, S. Modeling and comparison of dissolution profiles of diltiazem modified-release formulations. Dissolution Technol. 2009, 16, 41–46. [Google Scholar] [CrossRef]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm.-Drug Res. 2010, 67, 217–223. [Google Scholar]
- Costa, P.; Sousa Lobo, J.M. Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef]
- Ujhelyi, Z.; Fenyvesi, F.; Váradi, J.; Fehér, P.; Kiss, T.; Veszelka, S.; Deli, M.; Vecsernyés, M.; Bácskay, I. Evaluation of cytotoxicity of surfactants used in self-micro emulsifying drug delivery systems and their effects on paracellular transport in Caco-2 cell monolayer. Eur. J. Pharm. Sci. 2012, 47, 564–573. [Google Scholar] [CrossRef]
- Kósa, D.; Peto, Á.; Fenyvesi, F.; Váradi, J.; Vecsernyés, M.; Gonda, S.; Vasas, G.; Fehér, P.; Bácskay, I.; Ujhelyi, Z. Formulation of novel liquid crystal (Lc) formulations with skin-permeation-enhancing abilities of plantago lanceolata (pl) extract and their assessment on hacat cells. Molecules 2021, 26, 1023. [Google Scholar] [CrossRef]
- Újhelyi, J.; Újhelyi, Z.; Szalai, A.; László, J.F.; Cayasso, M.; Vecsernyés, M.; Pórszász, R. Analgesic and anti-inflammatory effectiveness of sitagliptin and vildagliptin in mice. Regul. Pept. 2014, 194–195, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Bánvölgyi, Á.; Pozsgai, G.; Brain, S.D.; Helyes, Z.S.; Szolcsányi, J.; Ghosh, M.; Melegh, B.; Pintér, E. Mustard oil induces a transient receptor potential vanilloid 1 receptor-independent neurogenic inflammation and a non-neurogenic cellular inflammatory component in mice. Neuroscience 2004, 125, 449–459. [Google Scholar] [CrossRef]
- Carlson, R.P.; O’neill-Davis, L.; Chang, J.; Lewis, A.J. Modulation of Mouse Ear Edema by Cyclooxygenase and Fipoxygenase Inhibitors and other Pharmacologic Agents; Birkhäuser Verlag: Basel, Switzerland, 1985; Volume 17. [Google Scholar]
- Sun, Y.; Oberley, L.W.; Li, Y. A simple method for clinical assay of superoxide dismutase. Clin. Chem. 1988, 34, 497–500. [Google Scholar] [CrossRef]
- Szabados-Furjesi, P.; Pajtas, D.; Barta, A.; Csepanyi, E.; Kiss-Szikszai, A.; Tosaki, A.; Bak, I. Synthesis, in vitro biological evaluation, and oxidative transformation of new flavonol derivatives: The possible role of the phenyl-N,N-dimethylamino group. Molecules 2018, 23, 3161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eder, K.; Vizler, C.; Kusz, E.; Karcagi, I.; Glavinas, H.; Balogh, G.E.; Vigh, L.; Duda, E.; Gyorfy, Z. The role of lipopolysaccharide moieties in macrophage response to Escherichia coli. Biochem. Biophys. Res. Commun. 2009, 389, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Csepanyi, E.; Szabados-Furjesi, P.; Kiss-Szikszai, A.; Frensemeier, L.M.; Karst, U.; Lekli, I.; Haines, D.D.; Tosaki, A.; Bak, I. Antioxidant properties and oxidative transformation of different chromone derivatives. Molecules 2017, 22, 588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sumegi, K.; Fekete, K.; Antus, C.; Debreceni, B.; Hocsak, E.; Gallyas, F.; Sumegi, B.; Szabo, A. BGP-15 protects against oxidative stress- or lipopolysaccharide-induced mitochondrial destabilization and reduces mitochondrial production of reactive oxygen species. PLoS ONE 2017, 12, e0169372. [Google Scholar] [CrossRef] [Green Version]
- Crul, T.; Toth, N.; Piotto, S.; Literati-Nagy, P.; Tory, K.; Haldimann, P.; Kalmar, B.; Greensmith, L.; Torok, Z.; Balogh, G.; et al. Hydroximic Acid Derivatives: Pleiotropic Hsp Co-Inducers Restoring Homeostasis and Robustness. Curr. Pharm. Des. 2013, 19, 309–346. [Google Scholar] [CrossRef]
- Giansanti, V.; Donà, F.; Tillhon, M.; Scovassi, A.I. PARP inhibitors: New tools to protect from inflammation. Biochem. Pharmacol. 2010, 80, 1869–1877. [Google Scholar] [CrossRef]
- Peralta-Leal, A.; Rodríguez-Vargas, J.M.; Aguilar-Quesada, R.; Rodríguez, M.I.; Linares, J.L.; de Almodóvar, M.R.; Oliver, F.J. PARP inhibitors: New partners in the therapy of cancer and inflammatory diseases. Free Radic. Biol. Med. 2009, 47, 13–26. [Google Scholar] [CrossRef]
- Wachal, Z.; Szilágyi, A.; Takács, B.; Szabó, A.M.; Priksz, D.; Bombicz, M.; Szilvássy, J.; Juhász, B.; Szilvássy, Z.; Varga, B. Improved Survival and Retinal Function of Aging ZDF Rats in Long-Term, Uncontrolled Diabetes by BGP-15 Treatment. Front. Pharmacol. 2021, 12, 580. [Google Scholar] [CrossRef]
- Nagy, G.; Szarka, A.; Lotz, G.; Dóczi, J.; Wunderlich, L.; Kiss, A.; Jemnitz, K.; Veres, Z.; Bánhegyi, G.; Schaff, Z.; et al. BGP-15 inhibits caspase-independent programmed cell death in acetaminophen-induced liver injury. Toxicol. Appl. Pharmacol. 2010, 243, 96–103. [Google Scholar] [CrossRef]
- Wachal, Z.; Bombicz, M.; Priksz, D.; Hegedűs, C.; Kovács, D.; Szabó, A.M.; Kiss, R.; Németh, J.; Juhász, B.; Szilvássy, Z.; et al. Retinoprotection by BGP-15, a hydroximic acid derivative, in a type ii diabetic rat model compared to glibenclamide, metformin, and pioglitazone. Int. J. Mol. Sci. 2020, 21, 2124. [Google Scholar] [CrossRef] [Green Version]
- Csizmazia, E.; Eróős, G.; Berkesi, O.; Berk, S.; Szab-Révész, P.; Csnyi, E. Ibuprofen penetration enhance by sucrose ester examined by ATR-FTIR in vivo. Pharm. Dev. Technol. 2012, 17, 125–128. [Google Scholar] [CrossRef]
- Malingré, M.M.; Schellens, J.H.M.; Tellingen, O.; Van Ouwehand, M.; Bardelmeijer, H.A.; Rosing, H.; Koopman, F.J.; Schot, M.E.; Huinink, W.W.T.B.; Beijnen, J.H. The co-solvent Cremophor EL limits absorption of orally administered paclitaxel in cancer patients. Br. J. Cancer 2001, 85, 1472–1477. [Google Scholar] [CrossRef]
- Okur, N.Ü.; Yavasoglu, A.; Karasulu, H.Y. Preparation and evaluation of microemulsion formulations of naproxen for dermal delivery. Chem. Pharm. Bull. 2014, 62, 135–143. [Google Scholar] [CrossRef] [Green Version]
- Shafiq, S.; Shakeel, F. Effect of labrasol on self-nanoemulsification efficiency of ramipril nanoemulsion. Pharmazie 2009, 64, 812–817. [Google Scholar] [CrossRef]










| Composition | CMP 1 | CMP 2 | CMP 3 | CMP 4 | CMP 5 |
|---|---|---|---|---|---|
| Transcutol (1.4 g) | + | + | + | + | + |
| Emulsifier (3 g) | |||||
| Labrasol | + | − | − | − | − |
| Cremophor A6:A25 | − | + | − | − | − |
| SP50 | − | − | + | − | − |
| SP70 | − | − | − | + | − |
| PS750 | − | − | − | − | + |
| BGP-15 (10 g) | + | + | + | + | + |
| Cetostearyl alcohol (4.6 g) | + | + | + | + | + |
| Stearic acid (10 g) | + | + | + | + | + |
| Glycerol (5 g) | + | + | + | + | + |
| IPM (5 g) | + | + | + | + | + |
| Propylene glycol (5 g) | + | + | + | + | + |
| Purified water (ad 100.0 g) | + | + | + | + | + |
| Model | Equations [24,25] | Graphic | |
|---|---|---|---|
| Zero-order | (2) | The graphic of the drug-dissolved fraction versus time is linear. | |
| First-order | (3) | The graphic of the decimal logarithm of the released amount of drug versus time is linear. | |
| Kinetic Model | ||
|---|---|---|
| Composition | Zero | First |
| CMP 1. | 0.8549 | 0.8122 |
| CMP 2. | 0.7900 | 0.6249 |
| CMP 3. | 0.6465 | 0.1589 |
| CMP 4. | 0.7095 | 0.3765 |
| CMP 5. | 0.6502 | 0.1699 |
| Composition | Release Rate (k) (μg/cm2 × √min) | Diffusion Coefficient (D × 10−4; cm2/min) |
|---|---|---|
| CMP 1. | 279.49 | 3.81 |
| CMP 2. | 123.39 | 0.972 |
| CMP 3. | 593.64 | 17.00 |
| CMP 4. | 402.12 | 6.48 |
| CMP 5. | 551.53 | 14.1 |
| Composition | f1 | f2 |
|---|---|---|
| CMP 4. vs. CMP 3. | 34.19 | 49.06 |
| CMP 4. vs. CMP 5. | 28.98 | 54.19 |
| CMP 4. vs. CMP 1. | 35.59 | 56.54 |
| CMP 4. vs. CMP 2. | 70.49 | 42.66 |
| CMP 5. vs. CMP 1. | 54.26 | 40.49 |
| CMP 1. vs. CMP 2. | 54.18 | 56.47 |
| CMP 5. vs. CMP 2. | 79.04 | 32.78 |
| CMP 3. vs. CMP 2. | 80.58 | 30.71 |
| CMP 3. vs. CMP 1. | 57.61 | 37.62 |
| CMP 3. vs. CMP 5. | 7.33 | 80.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pető, Á.; Kósa, D.; Haimhoffer, Á.; Fehér, P.; Ujhelyi, Z.; Sinka, D.; Fenyvesi, F.; Váradi, J.; Vecsernyés, M.; Gyöngyösi, A.; et al. Nicotinic Amidoxime Derivate BGP-15, Topical Dosage Formulation and Anti-Inflammatory Effect. Pharmaceutics 2021, 13, 2037. https://doi.org/10.3390/pharmaceutics13122037
Pető Á, Kósa D, Haimhoffer Á, Fehér P, Ujhelyi Z, Sinka D, Fenyvesi F, Váradi J, Vecsernyés M, Gyöngyösi A, et al. Nicotinic Amidoxime Derivate BGP-15, Topical Dosage Formulation and Anti-Inflammatory Effect. Pharmaceutics. 2021; 13(12):2037. https://doi.org/10.3390/pharmaceutics13122037
Chicago/Turabian StylePető, Ágota, Dóra Kósa, Ádám Haimhoffer, Pálma Fehér, Zoltán Ujhelyi, Dávid Sinka, Ferenc Fenyvesi, Judit Váradi, Miklós Vecsernyés, Alexandra Gyöngyösi, and et al. 2021. "Nicotinic Amidoxime Derivate BGP-15, Topical Dosage Formulation and Anti-Inflammatory Effect" Pharmaceutics 13, no. 12: 2037. https://doi.org/10.3390/pharmaceutics13122037