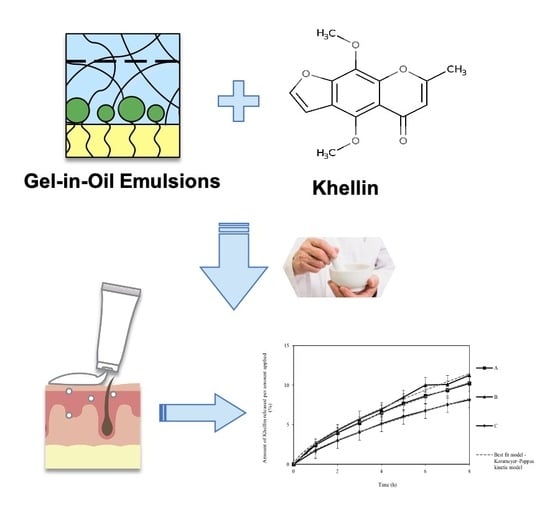
Development of Gel-in-Oil Emulsions for Khellin Topical Delivery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Emulsions Development
2.2.2. Physicochemical Characterization and Rheological Properties
Rotational and Dynamic Viscosity Measurements (Flow Curves)
Oscillatory Dynamic Test
Tackiness and Adhesion Test
Spreadability
2.2.3. Droplet Size Analysis
2.2.4. In Vitro Release Studies of KHE-Containing Gel-in-Oil Emulsions
2.2.5. In Vitro Permeation Studies of KHE-Containing Gel-in-Oil Emulsions
2.2.6. Quantification of KHE
2.2.7. Statistical Analysis
3. Results and Discussion
3.1. Structural Analysis of Emulsions
3.2. Droplet Size Analysis
3.3. KHE-Containing Emulsions: Homogenization and Dispersion Methods
3.4. In Vitro KHE Release
3.5. In Vitro KHE Permeation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Vallerand, I.A.; Lewinson, R.T.; Parsons, L.M.; Hardin, J.; Haber, R.M.; Lowerison, M.W.; Barnabe, C.; Patten, S.B. Vitiligo and major depressive disorder: A bidirectional population-based cohort study. J. Am. Acad. Dermatol. 2019, 80, 1371–1379. [Google Scholar] [CrossRef]
- Shivasaraun, U.V.; Sureshkumar, R.; Karthika, C.; Puttappa, N. Flavonoids as adjuvant in psoralen based photochemotherapy in the management of vitiligo/leucoderma. Med. Hypotheses 2018, 121, 26–30. [Google Scholar] [CrossRef]
- Marconi, B.; Mancini, F.; Colombo, P.; Allegra, F.; Giordano, F.; Gazzaniga, A.; Orecchia, G.; Santi, P. Distribution of khellin in excised human skin following iontophoresis and passive dermal transport. J. Control. Release 1999, 60, 261–268. [Google Scholar] [CrossRef]
- Ortel, B.; Tanew, A.; Hönigsmann, H. Treatment of vitiligo with khellin and ultraviolet A. J. Am. Acad. Dermatol. 1988, 18, 693–701. [Google Scholar] [CrossRef]
- Mahmoud, A.; Hassan, M.; Zubair, U. Khellin. Anal. Profiles Drug Subs. 1981, 9, 371–396. [Google Scholar]
- Abu-Hashem, A.A.; El-Shazly, M. Synthesis, reactions and biological activities of furochromones: A review. Eur. J. Med. Chem. 2015, 90, 633–665. [Google Scholar] [CrossRef] [PubMed]
- Beyazit, N.; Kaya, K.; Şenel, P.; Özdemir, A.D.; Gölcü, A. Crystal structure and DNA binding properties of khellin oxime. J. Mol. Struct. 2019, 1197, 450–457. [Google Scholar] [CrossRef]
- Radi, A. Voltammetric study of khellin at a DNA-coated carbon paste electrode. Anal. Chim. Acta 1999, 386, 63–68. [Google Scholar] [CrossRef]
- Niccolai, N.; Bovalini, L.; Martelli, P. The mechanisms of interaction between furanochromones and dna: A heteronuclear overhauser effect study on the khellin-thymidine model system. Biophys. Chem. 1986, 24, 217–220. [Google Scholar] [CrossRef]
- Vedaldi, D.; Caffieri, S.; Dall’Acqua, F.; Andreassi, L.; Bovalini, L. Khellin, a naturally occurring furochromone, used for the photochemotherapy of skin diseases: Mechanism of action. Ed. Sci. 1988, 43, 333–346. [Google Scholar]
- Orecchia, G.; Sangalli Me Gazzaniga, A.; Giordano, F. Topical photochemotherapy of vitiligo with a new khellin formulation. J. Dermatol. Treatm. 1998, 9, 65–69. [Google Scholar] [CrossRef]
- Grimes, P.E.; Minus, H.R.; Chakrabarti, S.G. Determination of optimal topical photochemotherapy for vitiligo. J. Am. Acad Dermatol. 1982, 7, 771–778. [Google Scholar] [CrossRef]
- Goyal, R.; Macri, L.K.; Kaplan, H.M.; Kohn, J. Nanoparticles and nanofibers for topical drug delivery. J. Control. Release 2016, 240, 77–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Güngör, S.; Erdal, M.S.; Aksu, B. New Formulation Strategies in Topical Antifungal Therapy. J. Cosmet Dermatol. Sci. Appl. 2013, 3, 56–65. [Google Scholar] [CrossRef] [Green Version]
- Bicho, J.; Marto, J.; Salgado, A.; Raposo, S.; Simões, S.; Margarida, H. Lipid Nanocarriers for Ketoconazole Topical Delivery. Gavin. J. Derm. Res. Ther. 2016, 2016, 7. [Google Scholar]
- Rodrigues, M.; Ezzedine, K.; Hamzavi, I.; Pandya, A.G.; Harris, J.E. New discoveries in the pathogenesis and classification of vitiligo. J. Am. Acad. Derm 2017, 77, 1–13. [Google Scholar] [CrossRef]
- Langer, R. Drug delivery and targeting. Nature 1998, 392, 6. [Google Scholar]
- Helm, M.F.; Farah, J.B.; Carvalho, M.; Farah, F.S.; Farah, R.S. Compounded Topical Medications for Diseases of the Skin: A Long Tradition Still Relevant Today. North. Am. J. Med. Sci. 2017, 10, 3. [Google Scholar]
- Mikula, R.J. Emulsion Characterization. In Emulsions; Schramm, L.L., Ed.; American Chemical Society: Washington, DC, USA, 1992; pp. 79–129. [Google Scholar]
- Edser, C. Three new vegetable-derived surfactants from Noveon Consumer Specialties. Focus Surfactants 2010, 7, 2. [Google Scholar]
- Edser, C. Seppic’s ecological emulsion for the skin & the planet. Focus Surfactants 2016, 2011, 5. [Google Scholar]
- Dickinson, E. Emulsion gels: The structuring of soft solids with protein-stabilized oil droplets. Food Hydrocolloid. 2012, 28, 224–241. [Google Scholar] [CrossRef]
- Energy efficiency: Cold process emulsifiers. Focus on Surfactants. 2011, 5, 4.
- Assessing Tackiness and Adhesion Using a Pull away Test on a Rotational Rheometer. Available online: https://cdn.technologynetworks.com/TN/Resources/PDF/AN150527AssessingTackinessPullAway.pdf (accessed on 22 April 2020).
- Djiobie Tchienou, G.E.; Tsatsop Tsague, R.K.; Mbam Pega, T.F.; Bama, V.; Bamseck, A.; Dongmo Sokeng, S.; Ngassoum, M.B. Multi-Response Optimization in the Formulation of a Topical Cream from Natural Ingredients. Cosmetics 2018, 5, 7. [Google Scholar] [CrossRef] [Green Version]
- BS 1993. Methods for determination of particle size distribution. Part 4, Guide to microscope and image analysis methods. In British Standards; BSI: London, UK, 1993. [Google Scholar]
- Costa, P.; Lobo, J.M.S. Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef]
- Ampucci, S.; Burgalassi, S.; Chetoni, P.; Monti, D. Cutaneous Permeation and Penetration of Sunscreens: Formulation Strategies and In Vitro Methods. Cosmetics 2018, 5, 1. [Google Scholar] [CrossRef] [Green Version]
- ICH, ICH Q2B Validation of Analytical Procedures: Methodology; European Agency for the Evaluation of Medicinal Products, International Commission on Harmonisation: London, UK, 1996.
- Gore, E.; Picard, C.; Savary, G. Spreading behavior of cosmetic emulsions: Impact of the oil phase. Biotribology 2018, 16, 17–24. [Google Scholar] [CrossRef]
- Siddig, M.A.; Radiman, S.; Jan, L.S.; Muniandy, S.V. Rheological behaviours of the hexagonal and lamellar phases of glucopone (APG) surfactant. Colloids Surf. Physicochem. Eng. Asp. 2006, 276, 15–21. [Google Scholar] [CrossRef]
- Pal, R. Effect of droplet size on the rheology of emulsions. AICHE J. 1996, 42, 3181–3190. [Google Scholar] [CrossRef]
- Rousseau, D. Fat crystals and emulsion stability—A review. Food Res. Int. 2000, 33, 3–14. [Google Scholar] [CrossRef]
- Ushikubo, F.Y.; Cunha, R.L. Stability mechanisms of liquid water-in-oil emulsions. Food Hydrocoll. 2012, 34, 145–153. [Google Scholar] [CrossRef]
- Cyprien, G.; Ludwik, L. Theory of Tackiness. Phys. Rev. Lett. 1999, 82, 936–939. [Google Scholar]
- Arias, E.M.; Guiró, P.; Rodriguez-Abreu, C.; Solans, C.; Escribano-Ferrer, E.; García-Celma, M.J. Cubic liquid crystalline structures in diluted, concentrated and highly concentrated emulsions for topical application: Influence on drug release and human skin permeation. Int. J. Pharm. 2019, 569, 118531. [Google Scholar] [CrossRef] [PubMed]
- Chambin, O.; Karbowiak, T.; Djebili, L.; Jannin, V.; Champion, D.; Pourcelot, Y.; Cayot, P. Influence of drug polarity upon the solid-state structure and release properties of self-emulsifying drug delivery systems in relation with water affinity. Colloids Surf. B Biointerfaces 2009, 71, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Marto, J.; Ruivo, E.; Lucas, S.D.; Gonçalves, L.M.; Simões, S.; Gouveia, L.F.; Felix, R.; Moreira, R.; Ribeiro, H.M.; Almeida, A.J. Starch nanocapsules containing a novel neutrophil elastase inhibitor with improved pharmaceutical performance. Eur. J. Pharm. Biopharm. 2018, 127, 1–11. [Google Scholar] [CrossRef]
- Mateus, D.; Marto, J.; Trindade, P.; Gonçalves, H.; Salgado, A.; Machado, P.; Melo-Gouveia, A.; Ribeiro, H.M.; Almeida, A.J. Improved Morphine-Loaded Hydrogels for Wound-Related Pain Relief. Pharmaceutics 2019, 11, 76. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, Y.; Petkar, K.C.; Sawant, K.K. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int. J. Pharm. 2010, 401, 93–102. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, Z. Phase transition and release kinetics of polyphenols encapsulated lyotropic liquid crystals. Int J. Pharm. 2019, 565, 283–293. [Google Scholar] [CrossRef]
- Dave, V.; Yadav, R.B.; Kushwaha, K.; Yadav, S.; Sharma, S.; Agrawal, U. Lipid-polymer hybrid nanoparticles: Development & statistical optimization of norfloxacin for topical drug delivery system. Bioact. Mater. 2017, 2, 269–280. [Google Scholar]
- Marto, J.; Duarte, A.; Simões, S.; Gonçalves, L.M.; Gouveia, L.F.; Almeida, A.J.; Ribeiro, H.M. Starch-based Pickering emulsions as platforms for topical antibiotic delivery: In vitro and in vivo studies. Polymers 2019, 11, 108. [Google Scholar] [CrossRef] [Green Version]






| Chemical Name | Function | Concentration (%, w/w) | ||
|---|---|---|---|---|
| Aqueous phase | A | B | C | |
| Water | Solvent | Qs100 | Qs100 | Qs100 |
| Polyacrylate-13; polyisobutene; polysorbate 20; sorbitan isostearate; water 1 | Emulsifier, Polymer | 3.0 | 3.0 | 3.0 |
| Oil phase | ||||
| Octyldodecanol; octyldodecyl xyloside, PEG-30 Dipolyhydroxystearate 2 | Surfactant/ Emulsifier | 3.0 | 3.0 | 3.0 |
| Isohexadecane | Emollient | 2.0 | - | - |
| C21-28 alkane | Emollient | - | 2.0 | - |
| C18-21 alkane | Emollient | - | - | 2.0 |
| Emulsion | Peak Normal Force (N) | Time for Force to Reduce by 90% of Peak (s) | Area under Force Time Curve (N.s) | Diameter of Spread Area (mm) |
|---|---|---|---|---|
| A | −2.15 ± 0.034 | −0.215 ± 0.0034 | 2.58 ± 0.12 | 48.3 ± 0.6 |
| B | −1.95 ± 0.035 | −0.195 ± 0.0035 | 2.27 ± 0.10 | 47.6 ± 0.4 |
| C | −2.22 ± 0.039 | −0.222 ± 0.0039 | 2.68 ± 0.14 | 46.7 ± 1.4 |
| Emulsions | Droplet Size Distribution (μm) | |||
|---|---|---|---|---|
| d(0.1) | d(0.5) | d(0.9) | Span | |
| A | 2.00 ± 0.06 | 2.50 ± 0.07 | 3.08 ± 0.18 | 0.47 ± 0.20 |
| B | 1.70 ± 0.16 | 2.19 ± 0.17 | 2.76 ± 0.11 | 0.62 ± 0.14 |
| C | 1.66 ± 0.03 | 2.17 ± 0.06 | 2.79 ± 0.12 | 0.67 ± 0.13 |
| A+KHE | 2.51 ± 0.07 | 3.28 ± 0.08 | 4.33 ± 0.13 | 0.46 ± 0.15 |
| B+KHE | 2.48 ± 0.02 | 4.28 ± 0.03 | 5.76 ± 0.05 | 0.58 ± 0.09 |
| C+KHE | 2.38 ± 0.06 | 3.42 ± 0.08 | 5.16 ± 0.10 | 0.62 ± 0.15 |
| Emulsion | Model | K | R2 Adjusted | AIC |
|---|---|---|---|---|
| A | Zero-Order | 1.564 ± 0.15 | 0.884 | 18.171 |
| First-Order | 0.017 ± 0.00 | 0.906 | 16.522 | |
| Higuchi | 3.734 ± 0.37 | 0.927 | 14.451 | |
| Korsmeyer–Peppas | 2.705 ± 0.29 | 0.98 | 4.630 | |
| n: 0.69 ± 0.013 | ||||
| B | Zero-Order | 1.420 ± 0.19 | 0.883 | 16.089 |
| First-Order | 0.015 ± 0.00 | 0.905 | 14.468 | |
| Higuchi | 3.395 ± 0.47 | 0.946 | 10.016 | |
| Korsmeyer–Peppas | 2.524 ± 0.45 | 0.997 | −17.263 | |
| n: 0.68 ± 0.032 | ||||
| C | Zero-order | 1.123 ± 0.16 | 0.914 | 9.425 |
| First-Order | 0.012 ± 0.00 | 0.928 | 7.872 | |
| Higuchi | 2.674 ± 0.40 | 0.925 | 9.131 | |
| Korsmeyer–Peppas | 1.860 ± 0.53 | 0.997 | −14.845 | |
| n: 0.73 ± 0.08 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, J.; Gonçalves, R.; Barreto, M.; Dias, C.; Carvalho, F.; Almeida, A.J.; Ribeiro, H.M.; Marto, J. Development of Gel-in-Oil Emulsions for Khellin Topical Delivery. Pharmaceutics 2020, 12, 398. https://doi.org/10.3390/pharmaceutics12050398
Pereira J, Gonçalves R, Barreto M, Dias C, Carvalho F, Almeida AJ, Ribeiro HM, Marto J. Development of Gel-in-Oil Emulsions for Khellin Topical Delivery. Pharmaceutics. 2020; 12(5):398. https://doi.org/10.3390/pharmaceutics12050398
Chicago/Turabian StylePereira, Joana, Rita Gonçalves, Margarida Barreto, Clarisse Dias, Fátima Carvalho, António J. Almeida, Helena Margarida Ribeiro, and Joana Marto. 2020. "Development of Gel-in-Oil Emulsions for Khellin Topical Delivery" Pharmaceutics 12, no. 5: 398. https://doi.org/10.3390/pharmaceutics12050398