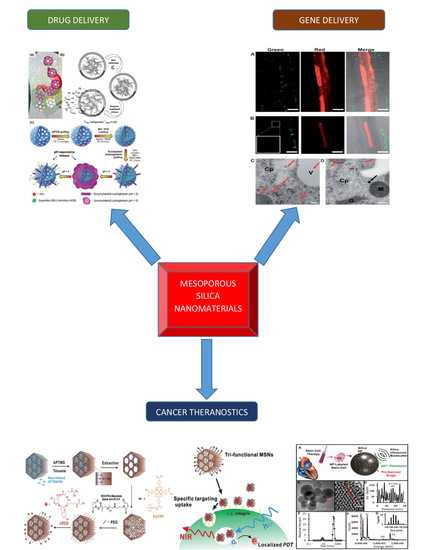
Mesoporous Silica Nanomaterials: Versatile Nanocarriers for Cancer Theranostics and Drug and Gene Delivery
Abstract
:1. Introduction
2. Cancer Therapy Using Silica Nanomaterials
2.1. Detection and Diagnosis of Cancer
2.2. Imaging Contrast Agents Using Silica Nanomaterials
2.3. Silica Chips Mesoporous Nanomaterials
3. Comprehensive Cancer Theranostics Using a Tri-Functionalized Silica Nanomaterial
4. Mesoporous Silica Nanomaterials in Theranostic Stem Cell Therapy
5. Brain Cancer Theranostics using Mesoporous Silica Nanomaterials
6. Mesoporous Silica Nanomaterials for Plant Gene Delivery
7. Intracellular Delivery of Nucleic Acids via Mesoporous Silica Nanomaterials
7.1. pDNA Delivery
7.2. siRNA Delivery
7.3. Co-Delivery of Nucleic Acids and Drugs
8. Oral Drug Delivery Using Mesoporous Silica Nanomaterials
9. Conclusions and Future Perspective
Funding
Acknowledgments
Conflicts of Interest
References
- Anand, P.; Kunnumakara, A.B.; Sundaram, C.; Harikumar, K.B.; Tharakan, S.T.; Lai, O.S.; Sung, B.; Aggarwal, B.B. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 2008, 25, 2097–2116. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulos, D.; Li, F.P.; Hunter, D.J. What causes cancer? Sci. Am. 1996, 275, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, M.; Fedele, S.; Russo, L.L. The World Cancer Report and the burden of oral cancer. Eur. J. Cancer Prev. 2004, 13, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Heath, J.R.; Davis, M.E. Nanotechnology and cancer. Annu. Rev. Med. 2008, 59, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Gillet, J.-P.; Gottesman, M.M. Mechanisms of multidrug resistance in cancer. In Multi-Drug Resistance in Cancer; Springer: New York, NY, USA, 2010; pp. 47–76. [Google Scholar]
- Ryu, J.-W.; Kim, Y.S. A case of advanced malignant pleural mesothelioma treatment with chemotherapy and photodynamic therapy. Tuberc. Respir. Dis. 2015, 78, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Triesscheijn, M.; Baas, P.; Schellens, J.H.; Stewart, F.A. Photodynamic therapy in oncology. Oncologist 2006, 11, 1034–1044. [Google Scholar] [CrossRef]
- Tinkle, S.; McNeil, S.E.; Mühlebach, S.; Bawa, R.; Borchard, G.; Barenholz, Y.C.; Tamarkin, L.; Desai, N. Nanomedicines: Addressing the scientific and regulatory gap. Ann. N. Y. Acad. Sci. 2014, 1313, 35–56. [Google Scholar] [CrossRef]
- Rosenholm, J.M.; Mamaeva, V.; Sahlgren, C.; Lindén, M. Nanoparticles in targeted cancer therapy: Mesoporous silica nanoparticles entering preclinical development stage. Nanomedicine 2012, 7, 111–120. [Google Scholar] [CrossRef]
- Loo, C.; Lowery, A.; Halas, N.; West, J.; Drezek, R. Immunotargeted nanoshells for integrated cancer imaging and therapy. Nano Lett. 2005, 5, 709–711. [Google Scholar] [CrossRef]
- Dickerson, E.B.; Dreaden, E.C.; Huang, X.; El-Sayed, I.H.; Chu, H.; Pushpanketh, S.; McDonald, J.F.; El-Sayed, M.A. Gold nanorod assisted near-infrared plasmonic photothermal therapy (PPTT) of squamous cell carcinoma in mice. Cancer Lett. 2008, 269, 57–66. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.; Liong, M.; Zink, J.I.; Tamanoi, F. Mesoporous silica nanoparticles as a delivery system for hydrophobic anticancer drugs. Small 2007, 3, 1341–1346. [Google Scholar] [CrossRef]
- Lu, J.; Liong, M.; Li, Z.; Zink, J.I.; Tamanoi, F. Biocompatibility, biodistribution, and drug-delivery efficiency of mesoporous silica nanoparticles for cancer therapy in animals. Small 2010, 6, 1794–1805. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Li, Z.; Zink, J.I.; Tamanoi, F. In vivo tumor suppression efficacy of mesoporous silica nanoparticles-based drug-delivery system: Enhanced efficacy by folate modification. Nanomed. Nanotechnol. Biol. Med. 2012, 8, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Morse, D.E. Silicon biotechnology: Harnessing biological silica production to construct new materials. Trends Biotechnol. 1999, 17, 230–232. [Google Scholar] [CrossRef]
- Lee, C.H.; Cheng, S.H.; Wang, Y.J.; Chen, Y.C.; Chen, N.T.; Souris, J.; Chen, C.T.; Mou, C.Y.; Yang, C.S.; Lo, L.W. Near-infrared mesoporous silica nanoparticles for optical imaging: Characterization and in vivo biodistribution. Adv. Funct. Mater. 2009, 19, 215–222. [Google Scholar] [CrossRef]
- Guillet-Nicolas, R.; Laprise-Pelletier, M.; Nair, M.M.; Chevallier, P.; Lagueux, J.; Gossuin, Y.; Laurent, S.; Kleitz, F.; Fortin, M.-A. Manganese-impregnated mesoporous silica nanoparticles for signal enhancement in MRI cell labelling studies. Nanoscale 2013, 5, 11499–11511. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yin, Q.; Ji, X.; Zhang, S.; Chen, H.; Zheng, Y.; Sun, Y.; Qu, H.; Wang, Z.; Li, Y. Manganese oxide-based multifunctionalized mesoporous silica nanoparticles for pH-responsive MRI, ultrasonography and circumvention of MDR in cancer cells. Biomaterials 2012, 33, 7126–7137. [Google Scholar] [CrossRef] [PubMed]
- Brevet, D.; Gary-Bobo, M.; Raehm, L.; Richeter, S.; Hocine, O.; Amro, K.; Loock, B.; Couleaud, P.; Frochot, C.; Morère, A. Mannose-targeted mesoporous silica nanoparticles for photodynamic therapy. Chem. Commun. 2009, 1475–1477. [Google Scholar] [CrossRef]
- Ahmadi, E.; Dehghannejad, N.; Hashemikia, S.; Ghasemnejad, M.; Tabebordbar, H. Synthesis and surface modification of mesoporous silica nanoparticles and its application as carriers for sustained drug delivery. Drug Deliv. 2014, 21, 164–172. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Q.; Han, N.; Bai, L.; Li, J.; Liu, J.; Che, E.; Hu, L.; Zhang, Q.; Jiang, T. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 313–327. [Google Scholar] [CrossRef]
- Vallet-Regi, M.; Ramila, A.; Del Real, R.; Pérez-Pariente, J. A new property of MCM-41: Drug delivery system. Chem. Mater. 2001, 13, 308–311. [Google Scholar] [CrossRef]
- Heikkilä, T.; Salonen, J.; Tuura, J.; Hamdy, M.; Mul, G.; Kumar, N.; Salmi, T.; Murzin, D.Y.; Laitinen, L.; Kaukonen, A. Mesoporous silica material TUD-1 as a drug delivery system. Int. J. Pharm. 2007, 331, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Song, S.-W.; Hidajat, K.; Kawi, S. Functionalized SBA-15 materials as carriers for controlled drug delivery: Influence of surface properties on matrix− drug interactions. Langmuir 2005, 21, 9568–9575. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Fan, C.; Lu, H.; Kan, A.T.; Tomson, M.B. Synthesis of crystalline-phase silica-based calcium phosphonate nanomaterials and their transport in carbonate and sandstone porous media. Ind. Eng. Chem. Res. 2011, 50, 1819–1830. [Google Scholar] [CrossRef]
- Aghaei, H.; Nourbakhsh, A.A.; Karbasi, S.; JavadKalbasi, R.; Rafienia, M.; Nourbakhsh, N.; Bonakdar, S.; Mackenzie, K.J. Investigation on bioactivity and cytotoxicity of mesoporous nano-composite MCM-48/hydroxyapatite for ibuprofen drug delivery. Ceram. Int. 2014, 40, 7355–7362. [Google Scholar] [CrossRef]
- Colilla, M.; Manzano, M.; Vallet-Regí, M. Recent advances in ceramic implants as drug delivery systems for biomedical applications. Int. J. Nanomed. 2008, 3, 403. [Google Scholar]
- Huang, X.; Young, N.P.; Townley, H.E. Characterization and comparison of mesoporous silica particles for optimized drug delivery. Nanomater. Nanotechnol. 2014, 4. [Google Scholar] [CrossRef]
- Tang, F.; Li, L.; Chen, D. Mesoporous silica nanoparticles: Synthesis, biocompatibility and drug delivery. Adv. Mater. 2012, 24, 1504–1534. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Li, J.; Qiao, S.; Hao, Z.; Tian, H.; Ma, C.; He, C. Synthesis and hydrophobic adsorption properties of microporous/mesoporous hybrid materials. J. Hazardous Mater. 2009, 164, 1205–1212. [Google Scholar] [CrossRef] [Green Version]
- Watermann, A.; Brieger, J. Mesoporous silica nanoparticles as drug delivery vehicles in cancer. Nanomaterials 2017, 7, 189. [Google Scholar] [CrossRef]
- Liberman, A.; Martinez, H.P.; Ta, C.N.; Barback, C.V.; Mattrey, R.F.; Kono, Y.; Blair, S.L.; Trogler, W.C.; Kummel, A.C.; Wu, Z. Hollow silica and silica-boron nano/microparticles for contrast-enhanced ultrasound to detect small tumors. Biomaterials 2012, 33, 5124–5129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsushita, H.; Mizukami, S.; Sugihara, F.; Nakanishi, Y.; Yoshioka, Y.; Kikuchi, K. Multifunctional core–shell silica nanoparticles for highly sensitive 19F magnetic resonance imaging. Angew. Chem. 2014, 126, 1026–1029. [Google Scholar] [CrossRef]
- Bouamrani, A.; Hu, Y.; Tasciotti, E.; Li, L.; Chiappini, C.; Liu, X.; Ferrari, M. Mesoporous silica chips for selective enrichment and stabilization of low molecular weight proteome. Proteomics 2010, 10, 496–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, F.; Zhang, B.; Zeng, S.; Lin, G.; Tian, J.; Yang, C.; Wang, K.; Xu, G.; Yong, K.-T. Folic acid-conjugated organically modified silica nanoparticles for enhanced targeted delivery in cancer cells and tumor in vivo. J. Mater. Chem. B 2015, 3, 6081–6093. [Google Scholar] [CrossRef]
- Gazouli, M.; Lyberopoulou, A.; Pericleous, P.; Rizos, S.; Aravantinos, G.; Nikiteas, N.; Anagnou, N.P.; Efstathopoulos, E.P. Development of a quantum-dot-labelled magnetic immunoassay method for circulating colorectal cancer cell detection. World J. Gastroenterol. 2012, 18, 4419. [Google Scholar] [CrossRef]
- Zheng, T.; Pierre-Pierre, N.; Yan, X.; Huo, Q.; Almodovar, A.J.; Valerio, F.; Rivera-Ramirez, I.; Griffith, E.; Decker, D.D.; Chen, S. Gold nanoparticle-enabled blood test for early stage cancer detection and risk assessment. ACS Appl. Mater. Interfaces 2015, 7, 6819–6827. [Google Scholar] [CrossRef]
- Wu, X.; Wu, M.; Zhao, J.X. Recent development of silica nanoparticles as delivery vectors for cancer imaging and therapy. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 297–312. [Google Scholar] [CrossRef] [Green Version]
- Cai, W.; Gao, T.; Hong, H.; Sun, J. Applications of gold nanoparticles in cancer nanotechnology. Nanotechnol. Sci. Appl. 2008, 1, 17. [Google Scholar] [CrossRef]
- Peng, C.-W.; Li, Y. Application of quantum dots-based biotechnology in cancer diagnosis: Current status and future perspectives. J. Nanomater. 2010, 2010, 5. [Google Scholar] [CrossRef]
- Jasanoff, A. MRI contrast agents for functional molecular imaging of brain activity. Curr. Opin. Neurobiol. 2007, 17, 593–600. [Google Scholar] [CrossRef] [Green Version]
- Martinez, H.P.; Kono, Y.; Blair, S.L.; Sandoval, S.; Wang-Rodriguez, J.; Mattrey, R.F.; Kummel, A.C.; Trogler, W.C. Hard shell gas-filled contrast enhancement particles for colour Doppler ultrasound imaging of tumors. MedChemComm 2010, 1, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Milgroom, A.; Intrator, M.; Madhavan, K.; Mazzaro, L.; Shandas, R.; Liu, B.; Park, D. Mesoporous silica nanoparticles as a breast-cancer targeting ultrasound contrast agent. Colloids Surfaces B Biointerfaces 2014, 116, 652–657. [Google Scholar] [CrossRef] [Green Version]
- Le Trequesser, Q.; Seznec, H.; Delville, M.-H. Functionalized nanomaterials: Their use as contrast agents in bioimaging: Mono-and multimodal approaches. Nanotechnol. Rev. 2013, 2, 125–169. [Google Scholar] [CrossRef]
- Aptekar, J.W.; Cassidy, M.C.; Johnson, A.C.; Barton, R.A.; Lee, M.; Ogier, A.C.; Vo, C.; Anahtar, M.N.; Ren, Y.; Bhatia, S.N. Silicon nanoparticles as hyperpolarized magnetic resonance imaging agents. ACS Nano 2009, 3, 4003–4008. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, M.; Chan, H.; Ross, B.; Bhattacharya, P.; Marcus, C.M. In vivo magnetic resonance imaging of hyperpolarized silicon particles. Nat. Nanotechnol. 2013, 8, 363. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Assmann, S.M. Mass spectrometry. An essential tool in proteome analysis. Plant Physiol. 2000, 123, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Panwar, N.; Tng, D.J.H.; Tjin, S.C.; Wang, K.; Yong, K.-T. The application of mesoporous silica nanoparticle family in cancer theranostics. Coord. Chem. Rev. 2016, 319, 86–109. [Google Scholar] [CrossRef]
- Imai, K.; Ichibangase, T.; Saitoh, R.; Hoshikawa, Y. A proteomics study on human breast cancer cell lines by fluorogenic derivatization–liquid chromatography/tandem mass spectrometry. Biomed. Chromatogr. 2008, 22, 1304–1314. [Google Scholar] [CrossRef] [PubMed]
- Paulo, J.A.; Kadiyala, V.; Banks, P.A.; Steen, H.; Conwell, D.L. Mass spectrometry-based proteomics for translational research: A technical overview. Yale J. Biol. Med. 2012, 85, 59. [Google Scholar] [PubMed]
- Xie, F.; Liu, T.; Qian, W.-J.; Petyuk, V.A.; Smith, R.D. Liquid chromatography-mass spectrometry-based quantitative proteomics. J. Biol. Chem. 2011, 286, 25433–25449. [Google Scholar] [CrossRef]
- Wasinger, V.C.; Zeng, M.; Yau, Y. Current status and advances in quantitative proteomic mass spectrometry. Int. J. Proteom. 2013, 2013, 180605. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Feild, B.; FitzHugh, W.; Heidbrink, J.L.; Duff, J.W.; Heil, J.; Ruben, S.M.; He, T. Reference map for liquid chromatography–mass spectrometry-based quantitative proteomics. Anal. Biochem. 2009, 393, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Peng, Y.; Lin, K.; Shen, H.; Brousseau III, L.C.; Sakamoto, J.; Sun, T.; Ferrari, M. Surface engineering on mesoporous silica chips for enriching low molecular weight phosphorylated proteins. Nanoscale 2011, 3, 421–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jäger, T.; Szarvas, T.; Börgermann, C.; Schenck, M.; Schmid, K.; Rübben, H. Use of silicon chip technology to detect protein-based tumor markers in bladder cancer. Der Urologe. Ausg. A 2007, 46, 1152–1156. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Li, Y.; Hu, Y. Nanotechnologies in glycoproteomics. Clin. Proteom. 2014, 11, 21. [Google Scholar] [CrossRef]
- Sprintz, M.; Tasciotti, E.; Allegri, M.; Grattoni, A.; Driver, L.C.; Ferrari, M. Nanomedicine: Ushering in a new era of pain management. Eur. J. Pain Suppl. 2011, 5, 317–322. [Google Scholar] [CrossRef]
- Cheng, S.-H.; Lee, C.-H.; Chen, M.-C.; Souris, J.S.; Tseng, F.-G.; Yang, C.-S.; Mou, C.-Y.; Chen, C.-T.; Lo, L.-W. Tri-functionalization of mesoporous silica nanoparticles for comprehensive cancer theranostics—The trio of imaging, targeting and therapy. J. Mater. Chem. 2010, 20, 6149–6157. [Google Scholar] [CrossRef]
- Slowing, I.; Trewyn, B.G.; Lin, V.S.-Y. Effect of surface functionalization of MCM-41-type mesoporous silica nanoparticles on the endocytosis by human cancer cells. J. Am. Chem. Soc. 2006, 128, 14792–14793. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Cheng, S.-H.; Hsieh, C.-C.; Chen, N.-T.; Chu, C.-H.; Huang, C.-M.; Chou, P.-T.; Tseng, F.-G.; Yang, C.-S.; Mou, C.-Y.; Lo, L.-W. Well-defined mesoporous nanostructure modulates three-dimensional interface energy transfer for two-photon activated photodynamic therapy. Nano Today 2011, 6, 552–563. [Google Scholar] [CrossRef]
- George, J.C. Stem cell therapy in acute myocardial infarction: A review of clinical trials. Transl. Res. 2010, 155, 10–19. [Google Scholar] [CrossRef]
- Bolli, R.; Chugh, A.R.; D’Amario, D.; Loughran, J.H.; Stoddard, M.F.; Ikram, S.; Beache, G.M.; Wagner, S.G.; Leri, A.; Hosoda, T. Cardiac stem cells in patients with ischaemic cardiomyopathy (SCIPIO): Initial results of a randomised phase 1 trial. Lancet 2011, 378, 1847–1857. [Google Scholar] [CrossRef]
- Chong, J.J.; Yang, X.; Don, C.W.; Minami, E.; Liu, Y.-W.; Weyers, J.J.; Mahoney, W.M.; Van Biber, B.; Cook, S.M.; Palpant, N.J. Human embryonic-stem-cell-derived cardiomyocytes regenerate non-human primate hearts. Nature 2014, 510, 273. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Porcel, M.; Gheysens, O.; Chen, I.Y.; Wu, J.C.; Gambhir, S.S. Image-guided cardiac cell delivery using high-resolution small-animal ultrasound. Mol. Ther. 2005, 12, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Vunjak-Novakovic, G.; Lui, K.O.; Tandon, N.; Chien, K.R. Bioengineering heart muscle: A paradigm for regenerative medicine. Annu. Rev. Biomed. Eng. 2011, 13, 245–267. [Google Scholar] [CrossRef]
- Nguyen, P.K.; Lan, F.; Wang, Y.; Wu, J.C. Imaging: Guiding the clinical translation of cardiac stem cell therapy. Circ. Res. 2011, 109, 962–979. [Google Scholar] [CrossRef]
- De Vries, I.J.M.; Lesterhuis, W.J.; Barentsz, J.O.; Verdijk, P.; Van Krieken, J.H.; Boerman, O.C.; Oyen, W.J.; Bonenkamp, J.J.; Boezeman, J.B.; Adema, G.J. Magnetic resonance tracking of dendritic cells in melanoma patients for monitoring of cellular therapy. Nat. Biotechnol. 2005, 23, 1407. [Google Scholar] [CrossRef]
- Laflamme, M.A.; Chen, K.Y.; Naumova, A.V.; Muskheli, V.; Fugate, J.A.; Dupras, S.K.; Reinecke, H.; Xu, C.; Hassanipour, M.; Police, S. Cardiomyocytes derived from human embryonic stem cells in pro-survival factors enhance function of infarcted rat hearts. Nat. Biotechnol. 2007, 25, 1015. [Google Scholar] [CrossRef]
- Wilson, K.; Homan, K.; Emelianov, S. Biomedical photoacoustics beyond thermal expansion using triggered nanodroplet vaporization for contrast-enhanced imaging. Nat. Commun. 2012, 3, 618. [Google Scholar] [CrossRef] [Green Version]
- Villanueva, F.S.; Jankowski, R.J.; Klibanov, S.; Pina, M.L.; Alber, S.M.; Watkins, S.C.; Brandenburger, G.H.; Wagner, W.R. Microbubbles targeted to intercellular adhesion molecule-1 bind to activated coronary artery endothelial cells. Circulation 1998, 98, 1–5. [Google Scholar] [CrossRef]
- Schutt, E.G.; Klein, D.H.; Mattrey, R.M.; Riess, J.G. Injectable microbubbles as contrast agents for diagnostic ultrasound imaging: The key role of perfluorochemicals. Angew. Chem. Int. Ed. 2003, 42, 3218–3235. [Google Scholar] [CrossRef] [PubMed]
- Klibanov, A.L. Ultrasound contrast materials in cardiovascular medicine: From perfusion assessment to molecular imaging. J. Cardiovasc. Transl. Res. 2013, 6, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Kuliszewski, M.A.; Fujii, H.; Liao, C.; Smith, A.H.; Xie, A.; Lindner, J.R.; Leong-Poi, H. Molecular imaging of endothelial progenitor cell engraftment using contrast-enhanced ultrasound and targeted microbubbles. Cardiovasc. Res. 2009, 83, 653–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, M.G.; Goodwill, P.W.; Neogy, A.; Yin, M.; Foster, F.S.; Schaffer, D.V.; Conolly, S.M. Biogenic gas nanostructures as ultrasonic molecular reporters. Nat. Nanotechnol. 2014, 9, 311. [Google Scholar] [CrossRef] [PubMed]
- Krupka, T.M.; Solorio, L.; Wilson, R.E.; Wu, H.; Azar, N.; Exner, A.A. Formulation and characterization of echogenic lipid− pluronic nanobubbles. Mol. Pharm. 2009, 7, 49–59. [Google Scholar] [CrossRef]
- Jokerst, J.V.; Khademi, C.; Gambhir, S.S. Intracellular aggregation of multimodal silica nanoparticles for ultrasound-guided stem cell implantation. Sci. Transl. Med. 2013, 5, 177ra135. [Google Scholar] [CrossRef]
- Casciaro, S.; Conversano, F.; Ragusa, A.; Malvindi, M.A.; Franchini, R.; Greco, A.; Pellegrino, T.; Gigli, G. Optimal enhancement configuration of silica nanoparticles for ultrasound imaging and automatic detection at conventional diagnostic frequencies. Investig. Radiol. 2010, 45, 715–724. [Google Scholar] [CrossRef]
- Liberman, A.; Wu, Z.; Barback, C.V.; Viveros, R.; Blair, S.L.; Ellies, L.G.; Vera, D.R.; Mattrey, R.F.; Kummel, A.C.; Trogler, W.C. Color doppler ultrasound and gamma imaging of intratumorally injected 500 nm iron–silica nanoshells. ACS Nano 2013, 7, 6367–6377. [Google Scholar] [CrossRef]
- Jokerst, J.V.; Thangaraj, M.; Kempen, P.J.; Sinclair, R.; Gambhir, S.S. Photoacoustic imaging of mesenchymal stem cells in living mice via silica-coated gold nanorods. ACS Nano 2012, 6, 5920–5930. [Google Scholar] [CrossRef]
- Ryu, J.C.; Davidson, B.P.; Xie, A.; Qi, Y.; Zha, D.; Belcik, J.T.; Caplan, E.S.; Woda, J.M.; Hedrick, C.C.; Hanna, R.N. Molecular imaging of the paracrine proangiogenic effects of progenitor cell therapy in limb ischemia. Circulation 2013, 127, 710–719. [Google Scholar] [CrossRef]
- Kokhuis, T.; Skachkov, I.; Naaijkens, B.; Juffermans, L.; Kamp, O.; Kooiman, K.; van der Steen, A.; Versluis, M.; de Jong, N. Intravital microscopy of localized stem cell delivery using microbubbles and acoustic radiation force. Biotechnol. Bioeng. 2015, 112, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Torney, F.; Trewyn, B.G.; Lin, V.S.-Y.; Wang, K. Mesoporous silica nanoparticles deliver DNA and chemicals into plants. Nat. Nanotechnol. 2007, 2, 295. [Google Scholar] [CrossRef] [PubMed]
- Slowing, I.I.; Trewyn, B.G.; Giri, S.; Lin, V.Y. Mesoporous silica nanoparticles for drug delivery and biosensing applications. Adv. Funct. Mater. 2007, 17, 1225–1236. [Google Scholar] [CrossRef]
- Slowing, I.I.; Trewyn, B.G.; Lin, V.S.-Y. Mesoporous silica nanoparticles for intracellular delivery of membrane-impermeable proteins. J. Am. Chem. Soc. 2007, 129, 8845–8849. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Barnes, J.C.; Bosoy, A.; Stoddart, J.F.; Zink, J.I. Mesoporous silica nanoparticles in biomedical applications. Chem. Soc. Rev. 2012, 41, 2590–2605. [Google Scholar] [CrossRef] [PubMed]
- Tarn, D.; Ashley, C.E.; Xue, M.; Carnes, E.C.; Zink, J.I.; Brinker, C.J. Mesoporous silica nanoparticle nanocarriers: Biofunctionality and biocompatibility. Acc. Chem. Res. 2013, 46, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Caltagirone, C.; Bettoschi, A.; Garau, A.; Montis, R. Silica-based nanoparticles: A versatile tool for the development of efficient imaging agents. Chem. Soc. Rev. 2015, 44, 4645–4671. [Google Scholar] [CrossRef] [PubMed]
- Kresge, C.; Leonowicz, M.; Roth, W.J.; Vartuli, J.; Beck, J. Ordered mesoporous molecular sieves synthesized by a liquid-crystal template mechanism. Nature 1992, 359, 710. [Google Scholar] [CrossRef]
- Chen, F.; Zhu, Y. Chitosan enclosed mesoporous silica nanoparticles as drug nano-carriers: Sensitive response to the narrow pH range. Microporous Mesoporous Mater. 2012, 150, 83–89. [Google Scholar] [CrossRef]
- Kempen, P.J.; Greasley, S.; Parker, K.A.; Campbell, J.L.; Chang, H.-Y.; Jones, J.R.; Sinclair, R.; Gambhir, S.S.; Jokerst, J.V. Theranostic mesoporous silica nanoparticles biodegrade after pro-survival drug delivery and ultrasound/magnetic resonance imaging of stem cells. Theranostics 2015, 5, 631. [Google Scholar] [CrossRef]
- Davis, M.E.; Hsieh, P.C.; Takahashi, T.; Song, Q.; Zhang, S.; Kamm, R.D.; Grodzinsky, A.J.; Anversa, P.; Lee, R.T. Local myocardial insulin-like growth factor 1 (IGF-1) delivery with biotinylated peptide nanofibers improves cell therapy for myocardial infarction. Proc. Natl. Acad. Sci. USA 2006, 103, 8155–8160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haider, H.K.; Jiang, S.; Idris, N.M.; Ashraf, M. IGF-1–overexpressing mesenchymal stem cells accelerate bone marrow stem cell mobilization via paracrine activation of SDF-1α/CXCR4 signaling to promote myocardial repair. Circ. Res. 2008, 103, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Rozhkova, E.A. Nanoscale materials for tackling brain cancer: Recent progress and outlook. Adv. Mater. 2011, 23, H136–H150. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, K.; Zhao, J.; Liu, X.; Bu, J.; Yan, X.; Huang, R. Multifunctional mesoporous silica-coated graphene nanosheet used for chemo-photothermal synergistic targeted therapy of glioma. J. Am. Chem. Soc. 2013, 135, 4799–4804. [Google Scholar] [CrossRef] [PubMed]
- Sonali; Agrawal, P.; Singh, R.P.; Rajesh, C.V.; Singh, S.; Vijayakumar, M.R.; Pandey, B.L.; Muthu, M.S. Transferrin receptor-targeted vitamin E TPGS micelles for brain cancer therapy: Preparation, characterization and brain distribution in rats. Drug Deliv. 2016, 23, 1788–1798. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, P.; Singh, R.P.; Kumari, L.; Sharma, G.; Koch, B.; Rajesh, C.V.; Mehata, A.K.; Singh, S.; Pandey, B.L.; Muthu, M.S. TPGS-chitosan cross-linked targeted nanoparticles for effective brain cancer therapy. Mater. Sci. Eng. C 2017, 74, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Pinhão, M.S. Characterization of the Toxic Potential of Nanomaterials Using in vitro Cell Models. Ph.D. Thesis, Universidade de Lisboa, Lisboa, Portuguese, 2014. [Google Scholar]
- He, Q.; Shi, J. MSN Anti-Cancer Nanomedicines: Chemotherapy Enhancement, Overcoming of Drug Resistance, and Metastasis Inhibition. Adv. Mater. 2014, 26, 391–411. [Google Scholar] [CrossRef]
- Sonali; Singh, R.P.; Singh, N.; Sharma, G.; Vijayakumar, M.R.; Koch, B.; Singh, S.; Singh, U.; Dash, D.; Pandey, B.L. Transferrin liposomes of docetaxel for brain-targeted cancer applications: Formulation and brain theranostics. Drug Deliv. 2016, 23, 1261–1271. [Google Scholar] [CrossRef]
- Agrawal, P.; Singh, R.P.; Sharma, G.; Mehata, A.K.; Singh, S.; Rajesh, C.V.; Pandey, B.L.; Koch, B.; Muthu, M.S. Bioadhesive micelles of d-α-tocopherol polyethylene glycol succinate 1000: Synergism of chitosan and transferrin in targeted drug delivery. Colloids Surfaces B Biointerfaces 2017, 152, 277–288. [Google Scholar] [CrossRef]
- Mo, J.; He, L.; Ma, B.; Chen, T. Tailoring particle size of mesoporous silica nanosystem to antagonize glioblastoma and overcome blood–brain barrier. ACS Appl. Mater. Interfaces 2016, 8, 6811–6825. [Google Scholar] [CrossRef]
- Liu, D.; Lin, B.; Shao, W.; Zhu, Z.; Ji, T.; Yang, C. In vitro and in vivo studies on the transport of PEGylated silica nanoparticles across the blood–brain barrier. ACS Appl. Mater. Interfaces 2014, 6, 2131–2136. [Google Scholar] [CrossRef] [PubMed]
- Bertucci, A.; Prasetyanto, E.A.; Septiadi, D.; Manicardi, A.; Brognara, E.; Gambari, R.; Corradini, R.; De Cola, L. Combined Delivery of Temozolomide and Anti-miR221 PNA Using Mesoporous Silica Nanoparticles Induces Apoptosis in Resistant Glioma Cells. Small 2015, 11, 5687–5695. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.-W.; Hung, Y.; Hsiao, J.-K.; Yao, M.; Chung, T.-H.; Lin, Y.-S.; Wu, S.-H.; Hsu, S.-C.; Liu, H.-M.; Mou, C.-Y. Bifunctional magnetic silica nanoparticles for highly efficient human stem cell labeling. Nano Lett. 2007, 7, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-S.; Tsai, C.-P.; Huang, H.-Y.; Kuo, C.-T.; Hung, Y.; Huang, D.-M.; Chen, Y.-C.; Mou, C.-Y. Well-ordered mesoporous silica nanoparticles as cell markers. Chem. Mater. 2005, 17, 4570–4573. [Google Scholar] [CrossRef]
- Singh, N.; Karambelkar, A.; Gu, L.; Lin, K.; Miller, J.S.; Chen, C.S.; Sailor, M.J.; Bhatia, S.N. Bioresponsive mesoporous silica nanoparticles for triggered drug release. J. Am. Chem. Soc. 2011, 133, 19582–19585. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Huang, Q.; Li, C.; Bao, C.; Liu, Z.; Li, F.; Zhu, L. Anticancer drug release from a mesoporous silica based nanophotocage regulated by either a one-or two-photon process. J. Am. Chem. Soc. 2010, 132, 10645–10647. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Cheng, S.H.; Huang, I.P.; Souris, J.S.; Yang, C.S.; Mou, C.Y.; Lo, L.W. Intracellular pH-responsive mesoporous silica nanoparticles for the controlled release of anticancer chemotherapeutics. Angew. Chem. 2010, 122, 8390–8395. [Google Scholar] [CrossRef]
- Chen, Y.-P.; Chen, C.-T.; Hung, Y.; Chou, C.-M.; Liu, T.-P.; Liang, M.-R.; Chen, C.-T.; Mou, C.-Y. A new strategy for intracellular delivery of enzyme using mesoporous silica nanoparticles: Superoxide dismutase. J. Am. Chem. Soc. 2013, 135, 1516–1523. [Google Scholar] [CrossRef]
- Radu, D.R.; Lai, C.-Y.; Jeftinija, K.; Rowe, E.W.; Jeftinija, S.; Lin, V.S.-Y. A polyamidoamine dendrimer-capped mesoporous silica nanosphere-based gene transfection reagent. J. Am. Chem. Soc. 2004, 126, 13216–13217. [Google Scholar] [CrossRef]
- Ashley, C.E.; Carnes, E.C.; Epler, K.E.; Padilla, D.P.; Phillips, G.K.; Castillo, R.E.; Wilkinson, D.C.; Wilkinson, B.S.; Burgard, C.A.; Kalinich, R.M. Delivery of small interfering RNA by peptide-targeted mesoporous silica nanoparticle-supported lipid bilayers. ACS Nano 2012, 6, 2174–2188. [Google Scholar] [CrossRef]
- Xia, T.; Kovochich, M.; Liong, M.; Meng, H.; Kabehie, S.; George, S.; Zink, J.I.; Nel, A.E. Polyethyleneimine coating enhances the cellular uptake of mesoporous silica nanoparticles and allows safe delivery of siRNA and DNA constructs. ACS Nano 2009, 3, 3273–3286. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.L.; Lin, Y.S.; Lin, H.Y.; Hung, Y.; Lo, L.W.; Chen, Y.F.; Mou, C.Y. In vitro studies of functionalized mesoporous silica nanoparticles for photodynamic therapy. Adv. Mater. 2009, 21, 172–177. [Google Scholar] [CrossRef]
- Yu, T.; Malugin, A.; Ghandehari, H. Impact of silica nanoparticle design on cellular toxicity and hemolytic activity. ACS Nano 2011, 5, 5717–5728. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Shi, J.; Zhu, M.; Chen, Y.; Chen, F. The three-stage in vitro degradation behavior of mesoporous silica in simulated body fluid. Microporous Mesoporous Mater. 2010, 131, 314–320. [Google Scholar] [CrossRef]
- Lee, C.W.; Mahendra, S.; Zodrow, K.; Li, D.; Tsai, Y.C.; Braam, J.; Alvarez, P.J. Developmental phytotoxicity of metal oxide nanoparticles to Arabidopsis thaliana. Environ. Toxicol. Chem. 2010, 29, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Slomberg, D.L.; Schoenfisch, M.H. Silica nanoparticle phytotoxicity to Arabidopsis thaliana. Environmental science & technology 2012, 46, 10247–10254. [Google Scholar]
- Parsons, J.G.; Lopez, M.L.; Gonzalez, C.M.; Peralta-Videa, J.R.; Gardea-Torresdey, J.L. Toxicity and biotransformation of uncoated and coated nickel hydroxide nanoparticles on mesquite plants. Environ. Toxicol. Chem. 2010, 29, 1146–1154. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.-P.; Kuang, L.-Y.; Huang, C.-A.; Jane, W.-N.; Hung, Y.; Yue-ie, C.H.; Mou, C.-Y. A simple plant gene delivery system using mesoporous silica nanoparticles as carriers. J. Mater. Chem. B 2013, 1, 5279–5287. [Google Scholar] [CrossRef]
- Villagarcia, H.; Dervishi, E.; de Silva, K.; Biris, A.S.; Khodakovskaya, M.V. Surface chemistry of carbon nanotubes impacts the growth and expression of water channel protein in tomato plants. Small 2012, 8, 2328–2334. [Google Scholar] [CrossRef]
- Lin, D.; Xing, B. Phytotoxicity of nanoparticles: Inhibition of seed germination and root growth. Environ. Pollut. 2007, 150, 243–250. [Google Scholar] [CrossRef]
- Kurepa, J.; Paunesku, T.; Vogt, S.; Arora, H.; Rabatic, B.M.; Lu, J.; Wanzer, M.B.; Woloschak, G.E.; Smalle, J.A. Uptake and distribution of ultrasmall anatase TiO2 Alizarin red S nanoconjugates in Arabidopsis thaliana. Nano Lett. 2010, 10, 2296–2302. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Chen, B.; Wang, Q.; Shi, X.; Xiao, Z.; Lin, J.; Fang, X. Carbon nanotubes as molecular transporters for walled plant cells. Nano Lett. 2009, 9, 1007–1010. [Google Scholar] [CrossRef] [PubMed]
- Serag, M.F.; Kaji, N.; Venturelli, E.; Okamoto, Y.; Terasaka, K.; Tokeshi, M.; Mizukami, H.; Braeckmans, K.; Bianco, A.; Baba, Y. Functional platform for controlled subcellular distribution of carbon nanotubes. ACS Nano 2011, 5, 9264–9270. [Google Scholar] [CrossRef] [PubMed]
- Etxeberria, E.; Gonzalez, P.; Baroja-Fernandez, E.; Romero, J.P. Fluid phase endocytic uptake of artificial nano-spheres and fluorescent quantum dots by sycamore cultured cells: Evidence for the distribution of solutes to different intracellular compartments. Plant Signal. Behav. 2006, 1, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Corredor, E.; Testillano, P.S.; Coronado, M.-J.; González-Melendi, P.; Fernández-Pacheco, R.; Marquina, C.; Ibarra, M.R.; de la Fuente, J.M.; Rubiales, D.; Pérez-de-Luque, A. Nanoparticle penetration and transport in living pumpkin plants: In situ subcellular identification. BMC Plant Biol. 2009, 9, 45. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Han, J.; Xiao, J.Q.; Jin, Y. Uptake, translocation, and accumulation of manufactured iron oxide nanoparticles by pumpkin plants. J. Environ. Monit. 2008, 10, 713–717. [Google Scholar] [CrossRef]
- Rico, C.M.; Majumdar, S.; Duarte-Gardea, M.; Peralta-Videa, J.R.; Gardea-Torresdey, J.L. Interaction of nanoparticles with edible plants and their possible implications in the food chain. J. Agric. Food Chem. 2011, 59, 3485–3498. [Google Scholar] [CrossRef]
- Nair, R.; Varghese, S.H.; Nair, B.G.; Maekawa, T.; Yoshida, Y.; Kumar, D.S. Nanoparticulate material delivery to plants. Plant Sci. 2010, 179, 154–163. [Google Scholar] [CrossRef]
- Martin-Ortigosa, S.; Valenstein, J.S.; Sun, W.; Moeller, L.; Fang, N.; Trewyn, B.G.; Lin, V.S.Y.; Wang, K. Parameters affecting the efficient delivery of mesoporous silica nanoparticle materials and gold nanorods into plant tissues by the biolistic method. Small 2012, 8, 413–422. [Google Scholar] [CrossRef]
- Martin-Ortigosa, S.; Valenstein, J.S.; Lin, V.S.Y.; Trewyn, B.G.; Wang, K. Gold functionalized mesoporous silica nanoparticle mediated protein and DNA codelivery to plant cells via the biolistic method. Adv. Funct. Mater. 2012, 22, 3576–3582. [Google Scholar] [CrossRef]
- Silva, A.T.; Nguyen, A.; Ye, C.; Verchot, J.; Moon, J.H. Conjugated polymer nanoparticles for effective siRNA delivery to tobacco BY-2 protoplasts. BMC Plant Biol. 2010, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wang, F.-H.; Wang, L.-L.; Xiao, S.-Y.; Tong, C.-Y.; Tang, D.-Y.; Liu, X.-M. Preparation of fluorescence starch-nanoparticle and its application as plant transgenic vehicle. J. Central South Univ. Technol. 2008, 15, 768–773. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, J.; Zhang, H.; Lu, M.; Qiu, D.; Wen, Y.; Kong, Q. Synthesis of water soluble quantum dots for monitoring carrier-DNA nanoparticles in plant cells. J. Nanosci. Nanotechnol. 2011, 11, 2208–2214. [Google Scholar] [CrossRef] [PubMed]
- Pasupathy, K.; Lin, S.; Hu, Q.; Luo, H.; Ke, P.C. Direct plant gene delivery with a poly (amidoamine) dendrimer. Biotechnol. J. Healthc. Nutr. Technol. 2008, 3, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, S.; Maitra, A.; Abdin, M.; Akmal, M.; Arora, I.; Samim, M. Calcium phosphate nanoparticle mediated genetic transformation in plants. J. Mater. Chem. 2012, 22, 3500–3507. [Google Scholar] [CrossRef]
- Fu, Y.-Q.; Li, L.-H.; Wang, P.-W.; Qu, J.; Fu, Y.-P.; Wang, H.; Sun, J.-R. Delivering DNA into plant cell by gene carriers of ZnS nanoparticles. Chem. Res. Chin. Univ. 2012, 28, 672–676. [Google Scholar]
- Giacca, M.; Zacchigna, S. Virus-mediated gene delivery for human gene therapy. J. Control. Release 2012, 161, 377–388. [Google Scholar] [CrossRef]
- Mishra, S.; Webster, P.; Davis, M.E. PEGylation significantly affects cellular uptake and intracellular trafficking of non-viral gene delivery particles. Eur. J. Cell Biol. 2004, 83, 97–111. [Google Scholar] [CrossRef]
- Kim, T.H.; Kim, M.; Eltohamy, M.; Yun, Y.R.; Jang, J.H.; Kim, H.W. Efficacy of mesoporous silica nanoparticles in delivering BMP-2 plasmid DNA for in vitro osteogenic stimulation of mesenchymal stem cells. J. Biomed. Mater. Res. Part A 2013, 101, 1651–1660. [Google Scholar] [CrossRef]
- He, C.-X.; Tabata, Y.; Gao, J.-Q. Non-viral gene delivery carrier and its three-dimensional transfection system. Int. J. Pharm. 2010, 386, 232–242. [Google Scholar] [CrossRef]
- Wong, J.K.; Mohseni, R.; Hamidieh, A.A.; MacLaren, R.E.; Habib, N.; Seifalian, A.M. Will nanotechnology bring new hope for gene delivery? Trends Biotechnol. 2017, 35, 434–451. [Google Scholar] [CrossRef] [PubMed]
- Aied, A.; Greiser, U.; Pandit, A.; Wang, W. Polymer gene delivery: Overcoming the obstacles. Drug Discov. Today 2013, 18, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Popat, A.; Karmakar, S.; Jambhrunkar, S.; Xu, C.; Yu, C. Curcumin-cyclodextrin encapsulated chitosan nanoconjugates with enhanced solubility and cell cytotoxicity. Colloids Surfaces B Biointerfaces 2014, 117, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Popat, A.; Ross, B.P.; Liu, J.; Jambhrunkar, S.; Kleitz, F.; Qiao, S.Z. Enzyme-responsive controlled release of covalently bound prodrug from functional mesoporous silica nanospheres. Angew. Chem. 2012, 124, 12654–12657. [Google Scholar] [CrossRef]
- Guillet-Nicolas, R.; Popat, A.; Bridot, J.L.; Monteith, G.; Qiao, S.Z.; Kleitz, F. pH-Responsive Nutraceutical-Mesoporous Silica Nanoconjugates with Enhanced Colloidal Stability. Angew. Chem. 2013, 125, 2374–2378. [Google Scholar] [CrossRef]
- Qin, F.; Zhou, Y.; Shi, J.; Zhang, Y. A DNA transporter based on mesoporous silica nanospheres mediated with polycation poly (allylamine hydrochloride) coating on mesopore surface. J. Biomed. Mater. Res. Part A 2009, 90, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Park, I.Y.; Kim, I.Y.; Yoo, M.K.; Choi, Y.J.; Cho, M.-H.; Cho, C.S. Mannosylated polyethylenimine coupled mesoporous silica nanoparticles for receptor-mediated gene delivery. Int. J. Pharm. 2008, 359, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Botella, P.; Corma, A.; Blesa, J.; Dong, L. Monodispersed mesoporous silica nanoparticles with very large pores for enhanced adsorption and release of DNA. J. Phys. Chem. B 2009, 113, 1796–1804. [Google Scholar] [CrossRef]
- Kim, M.-H.; Na, H.-K.; Kim, Y.-K.; Ryoo, S.-R.; Cho, H.S.; Lee, K.E.; Jeon, H.; Ryoo, R.; Min, D.-H. Facile synthesis of monodispersed mesoporous silica nanoparticles with ultralarge pores and their application in gene delivery. ACS Nano 2011, 5, 3568–3576. [Google Scholar] [CrossRef]
- Dengler, E.C.; Liu, J.; Kerwin, A.; Torres, S.; Olcott, C.M.; Bowman, B.N.; Armijo, L.; Gentry, K.; Wilkerson, J.; Wallace, J. Mesoporous silica-supported lipid bilayers (protocells) for DNA cargo delivery to the spinal cord. J. Control. Release 2013, 168, 209–224. [Google Scholar] [CrossRef] [Green Version]
- Brevet, D.; Hocine, O.; Delalande, A.; Raehm, L.; Charnay, C.; Midoux, P.; Durand, J.-O.; Pichon, C. Improved gene transfer with histidine-functionalized mesoporous silica nanoparticles. Int. J. Pharm. 2014, 471, 197–205. [Google Scholar] [CrossRef]
- Hom, C.; Lu, J.; Liong, M.; Luo, H.; Li, Z.; Zink, J.I.; Tamanoi, F. Mesoporous silica nanoparticles facilitate delivery of siRNA to shutdown signaling pathways in mammalian cells. Small 2010, 6, 1185–1190. [Google Scholar] [CrossRef] [PubMed]
- Na, H.K.; Kim, M.H.; Park, K.; Ryoo, S.R.; Lee, K.E.; Jeon, H.; Ryoo, R.; Hyeon, C.; Min, D.H. Efficient functional delivery of siRNA using mesoporous silica nanoparticles with ultralarge pores. Small 2012, 8, 1752–1761. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, T.; Li, L.; Wang, C.; Su, Z.; Li, J. Multifunctional fluorescent-magnetic polyethyleneimine functionalized Fe 3 O 4–mesoporous silica yolk–shell nanocapsules for siRNA delivery. Chem. Commun. 2012, 48, 8706–8708. [Google Scholar]
- Hartono, S.B.; Gu, W.; Kleitz, F.; Liu, J.; He, L.; Middelberg, A.P.; Yu, C.; Lu, G.Q.; Qiao, S.Z. Poly-L-lysine functionalized large pore cubic mesostructured silica nanoparticles as biocompatible carriers for gene delivery. ACS Nano 2012, 6, 2104–2117. [Google Scholar] [CrossRef]
- Li, X.; Chen, Y.; Wang, M.; Ma, Y.; Xia, W.; Gu, H. A mesoporous silica nanoparticle–PEI–fusogenic peptide system for siRNA delivery in cancer therapy. Biomaterials 2013, 34, 1391–1401. [Google Scholar] [CrossRef]
- Wang, M.; Li, X.; Ma, Y.; Gu, H. Endosomal escape kinetics of mesoporous silica-based system for efficient siRNA delivery. Int. J. Pharm. 2013, 448, 51–57. [Google Scholar] [CrossRef]
- Lin, D.; Cheng, Q.; Jiang, Q.; Huang, Y.; Yang, Z.; Han, S.; Zhao, Y.; Guo, S.; Liang, Z.; Dong, A. Intracellular cleavable poly (2-dimethylaminoethyl methacrylate) functionalized mesoporous silica nanoparticles for efficient siRNA delivery in vitro and in vivo. Nanoscale 2013, 5, 4291–4301. [Google Scholar] [CrossRef]
- Shen, J.; Kim, H.-C.; Su, H.; Wang, F.; Wolfram, J.; Kirui, D.; Mai, J.; Mu, C.; Ji, L.-N.; Mao, Z.-W. Cyclodextrin and polyethylenimine functionalized mesoporous silica nanoparticles for delivery of siRNA cancer therapeutics. Theranostics 2014, 4, 487. [Google Scholar] [CrossRef]
- Du, X.; Xiong, L.; Dai, S.; Kleitz, F.; Qiao, S.Z. Intracellular Microenvironment-Responsive Dendrimer-Like Mesoporous Nanohybrids for Traceable, Effective, and Safe Gene Delivery. Adv. Funct. Mater. 2014, 24, 7627–7637. [Google Scholar] [CrossRef]
- Chen, Y.; Gu, H.; Zhang, D.S.-Z.; Li, F.; Liu, T.; Xia, W. Highly effective inhibition of lung cancer growth and metastasis by systemic delivery of siRNA via multimodal mesoporous silica-based nanocarrier. Biomaterials 2014, 35, 10058–10069. [Google Scholar] [CrossRef] [PubMed]
- Hartono, S.B.; Yu, M.; Gu, W.; Yang, J.; Strounina, E.; Wang, X.; Qiao, S.; Yu, C. Synthesis of multi-functional large pore mesoporous silica nanoparticles as gene carriers. Nanotechnology 2014, 25, 055701. [Google Scholar] [CrossRef] [PubMed]
- Finlay, J.; Roberts, C.M.; Dong, J.; Zink, J.I.; Tamanoi, F.; Glackin, C.A. Mesoporous silica nanoparticle delivery of chemically modified siRNA against TWIST1 leads to reduced tumor burden. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 1657–1666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, L.; Bi, J.; Tang, Y.; Qiao, S.Z. Magnetic core–shell silica nanoparticles with large radial mesopores for siRNA delivery. Small 2016, 12, 4735–4742. [Google Scholar] [CrossRef] [PubMed]
- Möller, K.; Müller, K.; Engelke, H.; Bräuchle, C.; Wagner, E.; Bein, T. Highly efficient siRNA delivery from core–shell mesoporous silica nanoparticles with multifunctional polymer caps. Nanoscale 2016, 8, 4007–4019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhattarai, S.R.; Muthuswamy, E.; Wani, A.; Brichacek, M.; Castañeda, A.L.; Brock, S.L.; Oupicky, D. Enhanced gene and siRNA delivery by polycation-modified mesoporous silica nanoparticles loaded with chloroquine. Pharm. Res. 2010, 27, 2556–2568. [Google Scholar] [CrossRef]
- Chen, A.M.; Zhang, M.; Wei, D.; Stueber, D.; Taratula, O.; Minko, T.; He, H. Co-delivery of doxorubicin and Bcl-2 siRNA by mesoporous silica nanoparticles enhances the efficacy of chemotherapy in multidrug-resistant cancer cells. Small 2009, 5, 2673–2677. [Google Scholar] [CrossRef]
- Taratula, O.; Garbuzenko, O.B.; Chen, A.M.; Minko, T. Innovative strategy for treatment of lung cancer: Targeted nanotechnology-based inhalation co-delivery of anticancer drugs and siRNA. J. Drug Target. 2011, 19, 900–914. [Google Scholar] [CrossRef]
- Ma, X.; Teh, C.; Zhang, Q.; Borah, P.; Choong, C.; Korzh, V.; Zhao, Y. Redox-responsive mesoporous silica nanoparticles: A physiologically sensitive codelivery vehicle for siRNA and doxorubicin. Antioxid. Redox Signal. 2014, 21, 707–722. [Google Scholar] [CrossRef]
- Ma, X.; Zhao, Y.; Ng, K.W.; Zhao, Y. Integrated hollow mesoporous silica nanoparticles for target drug/siRNA co-delivery. Chem. A Eur. J. 2013, 19, 15593–15603. [Google Scholar] [CrossRef]
- Zhou, X.; Chen, L.; Nie, W.; Wang, W.; Qin, M.; Mo, X.; Wang, H.; He, C. Dual-responsive mesoporous silica nanoparticles mediated codelivery of doxorubicin and Bcl-2 SiRNA for targeted treatment of breast cancer. J. Phys. Chem. C 2016, 120, 22375–22387. [Google Scholar] [CrossRef]
- Meng, H.; Liong, M.; Xia, T.; Li, Z.; Ji, Z.; Zink, J.I.; Nel, A.E. Engineered design of mesoporous silica nanoparticles to deliver doxorubicin and P-glycoprotein siRNA to overcome drug resistance in a cancer cell line. ACS Nano 2010, 4, 4539–4550. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Mai, W.X.; Zhang, H.; Xue, M.; Xia, T.; Lin, S.; Wang, X.; Zhao, Y.; Ji, Z.; Zink, J.I. Codelivery of an optimal drug/siRNA combination using mesoporous silica nanoparticles to overcome drug resistance in breast cancer in vitro and in vivo. ACS Nano 2013, 7, 994–1005. [Google Scholar] [CrossRef] [PubMed]
- Kar, M.; Tiwari, N.; Tiwari, M.; Lahiri, M.; Gupta, S.S. Poly-L-Arginine Grafted Silica Mesoporous Nanoparticles for Enhanced Cellular Uptake and their Application in DNA Delivery and Controlled Drug Release. Part. Part. Syst. Charact. 2013, 30, 166–179. [Google Scholar] [CrossRef]
- Edwards, D.A.; Hanes, J.; Caponetti, G.; Hrkach, J.; Ben-Jebria, A.; Eskew, M.L.; Mintzes, J.; Deaver, D.; Lotan, N.; Langer, R. Large porous particles for pulmonary drug delivery. Science 1997, 276, 1868–1872. [Google Scholar] [CrossRef] [PubMed]
- Mitragotri, S.; Blankschtein, D.; Langer, R. Ultrasound-mediated transdermal protein delivery. Science 1995, 269, 850–853. [Google Scholar] [CrossRef] [PubMed]
- Mitragotri, S.; Burke, P.A.; Langer, R. Overcoming the challenges in administering biopharmaceuticals: Formulation and delivery strategies. Nat. Rev. Drug Discov. 2014, 13, 655. [Google Scholar] [CrossRef] [PubMed]
- Barua, S.; Mitragotri, S. Challenges associated with penetration of nanoparticles across cell and tissue barriers: A review of current status and future prospects. Nano Today 2014, 9, 223–243. [Google Scholar] [CrossRef] [Green Version]
- Mekaru, H.; Lu, J.; Tamanoi, F. Development of mesoporous silica-based nanoparticles with controlled release capability for cancer therapy. Adv. Drug Deliv. Rev. 2015, 95, 40–49. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Bennett, A.E. Synthesis, toxicology and potential of ordered mesoporous materials in nanomedicine. Nanomedicine 2011, 6, 867–877. [Google Scholar] [CrossRef]
- Zhang, R.X.; Ahmed, T.; Li, L.Y.; Li, J.; Abbasi, A.Z.; Wu, X.Y. Design of nanocarriers for nanoscale drug delivery to enhance cancer treatment using hybrid polymer and lipid building blocks. Nanoscale 2017, 9, 1334–1355. [Google Scholar] [CrossRef] [PubMed]
- Conniot, J.; Silva, J.M.; Fernandes, J.G.; Silva, L.C.; Gaspar, R.; Brocchini, S.; Florindo, H.F.; Barata, T.S. Cancer immunotherapy: Nanodelivery approaches for immune cell targeting and tracking. Front. Chem. 2014, 2, 105. [Google Scholar] [CrossRef] [PubMed]
- MacEwan, S.R.; Chilkoti, A. From composition to cure: A systems engineering approach to anticancer drug carriers. Angew. Chem. Int. Ed. 2017, 56, 6712–6733. [Google Scholar] [CrossRef] [PubMed]
- Popat, A.; Jambhrunkar, S.; Zhang, J.; Yang, J.; Zhang, H.; Meka, A.; Yu, C. Programmable drug release using bioresponsive mesoporous silica nanoparticles for site-specific oral drug delivery. Chem. Commun. 2014, 50, 5547–5550. [Google Scholar]
- Popat, A.; Liu, J.; Lu, G.Q.M.; Qiao, S.Z. A pH-responsive drug delivery system based on chitosan coated mesoporous silica nanoparticles. J. Mater. Chem. 2012, 22, 11173–11178. [Google Scholar] [CrossRef]
- Caillard, R.; Boutin, Y.; Subirade, M. Characterization of succinylated β-lactoglobulin and its application as the excipient in novel delayed release tablets. Int. Dairy J. 2011, 21, 27–33. [Google Scholar] [CrossRef]
- Poulin, J.-F.; Caillard, R.; Subirade, M. β-Lactoglobulin tablets as a suitable vehicle for protection and intestinal delivery of probiotic bacteria. Int. J. Pharm. 2011, 405, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Bernkop-Schnürch, A.; Dünnhaupt, S. Chitosan-based drug delivery systems. Eur. J. Pharm. Biopharm. 2012, 81, 463–469. [Google Scholar] [CrossRef]







| Initial Cancer Detection and Diagnosis | Drug Delivery Systems Used | Anti-MDR MSN-Based Systems | Reference |
|---|---|---|---|
| Imaging Contrast Agents | Utilizes the Passive delivery system | Concurrent delivery of multiple drugs | [32,33] |
| Mesoporous Silica Nano Chips | Utilizes the Active delivery system | Co-delivery of genes and anticancer drugs | [34] |
| Optical Imaging using Fluorescent Silica Nanoparticles | Utilizes the Controlled-release drug delivery systems | Multiple combination delivery systems | [35] |
| Nucleic Acid | Surface Coating | Size, nm | Cell Type Tested | Zeta Potential, mV | Reference |
|---|---|---|---|---|---|
| pDNA | PAMAM | particle: 250; pore: 2.7 | HeLa CHO | – | [111] |
| PAH | particle: 150; pore: 9.8 | PC1 | +20 | [148] | |
| mannosylated PEI | particle: 60–130; pore: not measured | RAW 264.7 HeLa | +5 to +50 | [149] | |
| aminopropyl groups | particle: 70–300; pore: 20 | – | – | [150] | |
| amino-functionalized MSN | particle: 300–400; large pore: 23; small pore: 2 | HeLa | +10 to +20 | [151] | |
| amine groups | particle: 205; pore: 2.6 | MSC PC12 HeLa CHO | +23 | [141] | |
| lipid bilayer | particle: 230; pore: 2-5 | RAW 264.7 HEK293 | +24 | [152] | |
| APTES and l-histidine | particle: 100-180; pore: 2.5 | HEK293T7 | +5 | [153] | |
| siRNA | PEI | particle: 100; pore: 2.5 | PANC-1 | – | [154] |
| PEGylated liposomes | particle: 165; pore: 23–30 | Hep3B | +12 | [112] | |
| APTES and PEG | particle: 200; pore: 23 | HeLa | +8 | [155] | |
| PEI | particle 63; pore: not measured | HeLa | +48 | [156] | |
| Poly-l-lysine (and APTES) | particle: 100-200; pore: 28 | HeLa KHOS | PLL +2 APTES +3 | [157] | |
| Fe3O4 core with mesoporous silica shell, and coated with PEI | particle: 50; pore: 3.6 | A549 | +25 | [158] | |
| PEI | particle: 50; pore: 3.7 | A549 | – | [159] | |
| PDMAEMA | particle: 100–150; pore: 10 | HeLa-Luc | +27 | [160] | |
| cyclodextrin and PEI-functionalized MSN | particle: 105; pore: not measured | MDA-MB231 | +47 | [161] | |
| PEI | particle: 178 (without siRNA); pore: 19 | KHOS | +34 | [162] | |
| PEI, PEG and KALA peptide | particle: 50; pore: 2.6 | A549 L02 PC-3 HCCLM-3 | +23 | [163] | |
| PEI | particle: 200; pore: 11 | KHOS | +51 | [164] | |
| PEI | particle: 127; pore: 2–3 | MDA-MB435S | +44 | [165] | |
| APTES + tannic acid | particle: 150; pore: 12 | KHOS | +21 | [166] | |
| cationic block copolymer | particle: 150; pore: 4 | KB | +30 to +40 | [167] |
| Surface Coating | Size, nm | Zeta Potential, mV | Nucleic Acid | Co-Delivered Drug | Cell Type Tested | Reference |
|---|---|---|---|---|---|---|
| PAMAM | particle: 200 pore: 2.88 | – | siRNA | DOX | A2780/AD | [169] |
| PEI | particle: 100–120 pore: 2–2.5 | +30 to +35 | siRNA | DOX | KB-V1 | [174] |
| PEG-LHRH peptide (luteinizing hormone-releasing hormone) | particle: 160–180 pore: 2.83–2.99 | – | siRNA | DOX CDDP | A549 | [170] |
| Poly-l-arginine-grafted MSNs | particle: 35–60 pore: 2.6 | +20 to +32 | pDNA | DOX | HeLa A549 | [176] |
| PEI-PEG copolymer | particle: 50 pore: not measured | +25 | siRNA | DOX | MCF-7 (multi-drug resistant) | [175] |
| PEI conjugated to folic acid | particle: 185 pore: 2.6 | +28 | siRNA | DOX | HeLa (high folic acid expression) MCF-7 | [172] |
| Ethylenediamine-modified β-cyclodextrin | particle: 150 pore: 2.7 | +20 | siRNA | DOX | HeLa | [171] |
| PEI-PLL copolymer | particle: 249 pore: 2.6 | +26 | siRNA | DOX | MDA-MB-231 | [173] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kesse, S.; Boakye-Yiadom, K.O.; Ochete, B.O.; Opoku-Damoah, Y.; Akhtar, F.; Filli, M.S.; Asim Farooq, M.; Aquib, M.; Maviah Mily, B.J.; Murtaza, G.; et al. Mesoporous Silica Nanomaterials: Versatile Nanocarriers for Cancer Theranostics and Drug and Gene Delivery. Pharmaceutics 2019, 11, 77. https://doi.org/10.3390/pharmaceutics11020077
Kesse S, Boakye-Yiadom KO, Ochete BO, Opoku-Damoah Y, Akhtar F, Filli MS, Asim Farooq M, Aquib M, Maviah Mily BJ, Murtaza G, et al. Mesoporous Silica Nanomaterials: Versatile Nanocarriers for Cancer Theranostics and Drug and Gene Delivery. Pharmaceutics. 2019; 11(2):77. https://doi.org/10.3390/pharmaceutics11020077
Chicago/Turabian StyleKesse, Samuel, Kofi Oti Boakye-Yiadom, Belynda Owoya Ochete, Yaw Opoku-Damoah, Fahad Akhtar, Mensura Sied Filli, Muhammad Asim Farooq, Md Aquib, Bazezy Joelle Maviah Mily, Ghulam Murtaza, and et al. 2019. "Mesoporous Silica Nanomaterials: Versatile Nanocarriers for Cancer Theranostics and Drug and Gene Delivery" Pharmaceutics 11, no. 2: 77. https://doi.org/10.3390/pharmaceutics11020077