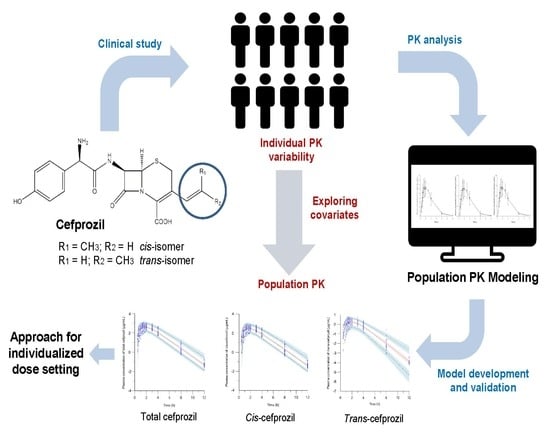
Population Pharmacokinetics of Cis-, Trans-, and Total Cefprozil in Healthy Male Koreans
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Determination of Plasma Cefprozil Concentrations
2.3. Model Development
2.4. Model Evaluation
3. Results
3.1. Subjects Characteristics
3.2. Determination of Plasma Cefprozil Concentrations
3.3. Model Development
3.4. Model Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wiseman, L.R.; Benfield, P. Cefprozil. Drugs 1993, 45, 295–317. [Google Scholar] [CrossRef] [PubMed]
- Fung-Tomc, J.C.; Huczko, E.; Stickle, T.; Minassian, B.; Kolek, B.; Denbleyker, K.; Bonner, D.; Kessler, R. Antibacterial activities of cefprozil compared with those of 13 oral cephems and 3 macrolides. Antimicrob. Agents Chemother. 1995, 39, 533–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ball, P. Efficacy and safety of cefprozil versus other beta-lactam antibiotics in the treatment of lower respiratory tract infections. Eur. J. Clin. Microbiol. Infect. Dis. 1994, 13, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Faiyaz, M.; Gupta, S.; Gupta, D. Antibiotic against gram-negative bacteria. In High Value Fermentation Products: Human Health; Saran, S., Babu, V., Chuabey, A., Eds.; John Wiley & Sons: New York, NY, USA, 2019; Volume 1, pp. 79–101. [Google Scholar]
- Parish, L.; Doyle, C.; Durham, S.; Wilber, R. Cefprozil versus cefaclor in the treatment of mild to moderate skin and skin-structure infections. The cefprozil multicenter study group. Clin. Ther. 1992, 14, 458–469. [Google Scholar] [PubMed]
- Aronovitz, G. Treatment of upper and lower respiratory tract infections: Clinical trials with cefprozil. Pediatr. Infect. Dis. J. 1998, 17, S83–S88. [Google Scholar] [CrossRef] [PubMed]
- Tewfik, T.L.; Garni, M.A. Tonsillopharyngitis: Clinical highlights. J. Otolaryngol. 2005, 34, S45–S49. [Google Scholar]
- van Eyk, A.D. Treatment of bacterial respiratory infections. S. Afr. Fam. Pract. 2019, 61, 8–15. [Google Scholar]
- Bhargava, S.; Lodha, R.; Kabra, S. Cefprozil: A review. Indian J. Pediatr. 2003, 70, 395–400. [Google Scholar] [CrossRef]
- Bilici, A.; Karaduman, M.; Cankir, Z. A rare case of hepatitis associated with cefprozil therapy. Scand. J. Infect. Dis. 2007, 39, 190–192. [Google Scholar] [CrossRef]
- Wise, R. Comparative microbiological activity and pharmacokinetics of cefprozil. Eur. J. Clin. Microbiol. Infect. Dis. 1994, 13, 839–845. [Google Scholar]
- Can, N.O. HPLC determination of cefprozil in tablets using monolithic and C18 silica columns. J. Sep. Sci. 2011, 34, 2223–2231. [Google Scholar] [CrossRef] [PubMed]
- He, G.; Mai, L.; Wang, X. Development and validation of an HPLC-MS/MS method for rapid simultaneous determination of cefprozil diastereomers in human plasma. Int. J. Anal. Chem. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.-H.; Jang, J.-H.; Cho, H.-Y.; Lee, Y.-B. Development and validation of a UPLC-ESI-MS/MS method and comparison with an HPLC-UV method for simultaneous determination of cis-, trans-cefprozil isomer in human plasma: Application to pharmacokinetics and correlation analysis. unpublished.
- Mosteller, R.D. Simplified calculation of body surface area. N. Engl. J. Med. 1987, 317, 1098. [Google Scholar] [PubMed]
- Cockcroft, D.W.; Gault, M.H. Prediction of creatinine clearance from serum creatinine. Nephron 1976, 16, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Barriere, S.L. Pharmacology and pharmacokinetics of cefprozil. Clin. Infect. Dis. 1992, 14, S184–S188. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, L.L. Cefprozil versus cefaclor in the treatment of bronchitis in the elderly. Drug Investig. 1994, 8, 263–270. [Google Scholar] [CrossRef]
- Barbhaiya, R.H.; Shukla, U.A.; Gleason, C.R.; Shyu, W.C.; Wilber, R.B.; Martin, R.R.; Pittman, K.A. Phase I study of multiple-dose cefprozil and comparison with cefaclor. Antimicrob. Agents Chemother. 1990, 34, 1198–1203. [Google Scholar] [CrossRef] [Green Version]
- Fassbender, M.; Lode, H.; Schaberg, T.; Borner, K.; Koeppe, P. Pharmacokinetics of new oral cephalosporins, including a new carbacephem. Clin. Infect. Dis. 1993, 16, 646–653. [Google Scholar] [CrossRef]
- Lima-Rogel, V.; Medina-Rojas, E.L.; Del Carmen Milán-Segovia, R.; Noyola, D.E.; Nieto-Aguirre, K.; López-Delarosa, A.; Romano-Moreno, S. Population pharmacokinetics of cefepime in neonates with severe nosocomial infections. J. Clin. Pharm. Ther. 2008, 33, 295–306. [Google Scholar] [CrossRef]
- Chandorkar, G.; Xiao, A.; Mouksassi, M.-S.; Hershberger, E.; Krishna, G. Population pharmacokinetics of ceftolozane/tazobactam in healthy volunteers, subjects with varying degrees of renal function and patients with bacterial infections. J. Clin. Pharmacol. 2015, 55, 230–239. [Google Scholar] [CrossRef]
- Kawaguchi, N.; Katsube, T.; Echols, R.; Wajima, T. Population pharmacokinetic analysis of cefiderocol, a parenteral siderophore cephalosporin, in healthy subjects, subjects with various degrees of renal function, and patients with complicated urinary tract infection or acute uncomplicated pyelonephritis. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef] [PubMed]
- Shyu, W.C.; Pittman, K.A.; Wilber, R.B.; Matzke, G.R.; Barbhaiya, R.H. Pharmacokinetics of cefprozil in healthy subjects and patients with renal impairment. J. Clin. Pharmacol. 1991, 31, 362–371. [Google Scholar] [PubMed]
- Barriere, S.L. Review of in vitro activity, pharmacokinetic characteristics, safety, and clinical efficacy of cefprozil, a new oral cephalosporin. Ann. Pharmacother. 1993, 27, 1082–1089. [Google Scholar] [PubMed]
- Shyu, W.C.; Wilber, R.B.; Pittman, K.A.; Garg, D.C.; Barbhaiya, R.H. Pharmacokinetics of cefprozil in healthy subjects and patients with hepatic impairment. J. Clin. Pharmacol. 1991, 31, 372–376. [Google Scholar] [PubMed]
- Bretschneider, B.; Brandsch, M.; Neubert, R. Intestinal transport of β-lactam antibiotics: Analysis of the affinity at the H+/peptide symporter (PEPT1), the uptake into Caco-2 cell monolayers and the transepithelial flux. Pharm. Res. 1999, 16, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, U.; Kuntz, S.; Diestel, S.; Daniel, H. PEPT1-mediated cefixime uptake into human intestinal epithelial cells is increased by Ca2+ channel blockers. Antimicrob. Agents Chemother. 2002, 46, 1375–1380. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.; Takahara, S.; Kato, S.; Kubo, Y.; Sai, Y.; Tamai, I.; Yabuuchi, H.; Tsuji, A. Involvement of multidrug resistance-associated protein 2 (Abcc2) in molecular weight-dependent biliary excretion of β-lactam antibiotics. Drug Metab. Dispos. 2008, 36, 1088–1096. [Google Scholar]
- Nakakariya, M.; Shimada, T.; Irokawa, M.; Maeda, T.; Tamai, I. Identification and species similarity of OATP transporters responsible for hepatic uptake of beta-lactam antibiotics. Drug Metab. Pharmacokinet. 2008, 23, 347–355. [Google Scholar] [CrossRef]
- Toutain, P.L.; Bousquet-Mélou, A. Volumes of distribution. J. Vet. Pharmacol. Ther. 2004, 27, 441–453. [Google Scholar]
- Park, T.-H.; Kim, J.-K.; Jee, J.-P.; Park, J.-S.; Kim, C.-K. HPLC method for simultaneous determination of cefprozil diastereomers in human plasma. J. Pharm. Biomed. Anal. 2004, 36, 243–248. [Google Scholar] [CrossRef]





| Characteristic | Median (Min, Max) | Mean ± SD |
|---|---|---|
| Age (year) | 24 (21, 27) | 24 ± 1.53 |
| Weight (kg) | 69.5 (53.1, 91.8) | 69.77 ± 9.99 |
| BSA (m2) | 1.84 (1.61, 2.16) | 1.84 ± 0.16 |
| Total proteins (g/dL) | 7.5 (6.8, 8.4) | 7.48 ± 0.37 |
| Albumin (g/dL) | 4.9 (4.4, 5.3) | 4.84 ± 0.25 |
| AST (U/L) | 18 (12, 38) | 20.31 ± 5.70 |
| ALT (U/L) | 17 (10, 42) | 19.63 ± 8.36 |
| ALP (U/L) | 66 (46, 105) | 69.83 ± 15.63 |
| Total bilirubin (mg/dL) | 0.92 (0.31, 2.23) | 1.01 ± 0.39 |
| BUN (mg/dL) | 13.3 (8.6, 22.9) | 13.55 ± 3.24 |
| Creatinine (mg/dL) | 0.9 (0.7, 1.2) | 0.91 ± 0.11 |
| CrCl (mL/min) | 124.41 (86.57, 159.05) | 124.55 ± 17.78 |
| Model | Description | nParameter | -2LL | AIC | △-2LL | △AIC |
|---|---|---|---|---|---|---|
| Total cefprozil | ||||||
| Absorption model | ||||||
| 01 | No Tlag | 7 | 1547.07 | 1561.07 | ||
| 02 * | Add Tlag | 9 | 1328.15 | 1346.15 | −218.92 | −214.92 |
| Residual error model | ||||||
| 02-01 | Proportional | 9 | 1328.15 | 1346.15 | ||
| 02-02 | Additive | 9 | 1479.58 | 1497.58 | 151.42 | 151.42 |
| 02-03 * | Log additive | 9 | 23.04 | 41.04 | −1305.11 | −1305.11 |
| IIV model | ||||||
| 02-03-01 | Remove IIV V | 8 | 23.04 | 39.04 | 0.00 | −2.00 |
| 02-03-02 | Remove IIV Cl | 8 | 69.66 | 85.66 | 46.62 | 44.62 |
| 02-03-03 * | Remove IIV Ka | 8 | 0.83 | 16.83 | −22.21 | −24.21 |
| 02-03-04 | Remove IIV Tlag | 8 | 56.45 | 72.45 | 33.41 | 31.41 |
| 02-03-05 | Remove IIV V, Ka | 7 | 217.49 | 231.49 | 194.45 | 190.45 |
| Cis-cefprozil | ||||||
| Absorption model | ||||||
| 01 | No Tlag | 7 | 1478.56 | 1492.56 | ||
| 02 * | Add Tlag | 9 | 1266.71 | 1284.71 | −211.84 | −207.84 |
| Residual error model | ||||||
| 02-01 | Proportional | 9 | 1266.71 | 1284.71 | ||
| 02-02 | Additive | 9 | 1416.03 | 1434.03 | 149.32 | 149.32 |
| 02-03 * | Log additive | 9 | 33.82 | 51.82 | −1232.89 | −1232.89 |
| IIV model | ||||||
| 02-03-01 | Remove IIV V | 8 | 33.82 | 49.82 | 0.00 | −2.00 |
| 02-03-02 | Remove IIV Cl | 8 | 81.03 | 97.03 | 47.21 | 45.21 |
| 02-03-03 * | Remove IIV Ka | 8 | 12.57 | 28.57 | −21.25 | −23.25 |
| 02-03-04 | Remove IIV Tlag | 8 | 63.44 | 79.44 | 29.62 | 27.62 |
| 02-03-05 | Remove IIV V, Ka | 7 | 224.58 | 238.58 | 190.76 | 186.76 |
| Trans-cefprozil | ||||||
| Absorption model | ||||||
| 01 | No Tlag | 7 | −60.47 | −46.47 | ||
| 02 * | Add Tlag | 9 | −251.70 | −233.70 | −191.23 | −187.23 |
| Residual error model | ||||||
| 02-01 * | Proportional | 9 | −251.70 | −233.70 | ||
| 02-02 | Additive | 9 | −109.81 | −91.81 | 141.89 | 141.89 |
| 02-03 | Log additive | 9 | 188.55 | 206.55 | 440.25 | 440.25 |
| IIV model | ||||||
| 02-03-01 * | Remove IIV V | 8 | −251.70 | −235.70 | 0.00 | −2.00 |
| 02-03-02 | Remove IIV Cl | 8 | −184.37 | −168.37 | 67.33 | 65.33 |
| 02-03-03 | Remove IIV Ka | 8 | 12.11 | 28.11 | 263.81 | 261.81 |
| 02-03-04 | Remove IIV Tlag | 8 | −202.32 | −186.32 | 49.39 | 47.39 |
| Model | OFV | △OFV |
|---|---|---|
| Total cefprozil | ||
| Base model | 0.829 | |
| Total protein on clearance | 0.693 | −0.136 |
| Albumin on clearance | 0.342 | −0.487 |
| CrCl on clearance * | −6.502 | −7.331 |
| Weight on volume | −2.075 | −2.904 |
| BSA on clearance | −1.585 | −2.413 |
| Cis-cefprozil | ||
| Base model | 12.568 | |
| Total protein on clearance | 12.385 | −0.184 |
| Albumin on clearance | 11.958 | −0.611 |
| CrCl on clearance * | 4.901 | −7.668 |
| Weight on volume | 9.956 | −2.612 |
| BSA on clearance | 9.287 | −3.282 |
| Trans-cefprozil | ||
| Base model * | −251.70 | |
| Total protein on clearance | −250.41 | 1.292 |
| Albumin on clearance | −254.46 | −2.763 |
| CrCl on clearance | −248.54 | 3.162 |
| BSA on clearance | −252.38 | −0.676 |
| Parameter | Estimate | SE | RSE (%) | Shrinkage (%) |
|---|---|---|---|---|
| Total cefprozil | ||||
| Base model | ||||
| tvV (mL) | 14,707.50 | 1200.54 | 8.16 | |
| tvCl (mL/h) | 17,189.00 | 451.80 | 2.63 | |
| tvTlag (h) | 0.352 | 0.013 | 3.73 | |
| tvKa (1/h) | 0.432 | 0.006 | 1.28 | |
| ω2V | 0.123 | 0.027 | 21.62 | 7.03 |
| ω2Cl | 0.018 | 0.005 | 26.15 | 9.05 |
| ω2Tlag | 0.020 | 0.007 | 32.05 | 21.43 |
| σ (μg/mL) | 0.190 | 0.017 | 9.03 | |
| Final model | ||||
| tvV (mL) | 14,713.10 | 1200.37 | 8.16 | |
| tvCl (mL/h) | 17,226.20 | 405.12 | 2.35 | |
| tvTlag (h) | 0.351 | 0.013 | 3.74 | |
| tvKa (1/h) | 0.432 | 0.006 | 1.28 | |
| dCldCrCl | 0.003 | 0.002 | 56.16 | |
| ω2V | 0.124 | 0.027 | 21.49 | 7.08 |
| ω2Cl | 0.016 | 0.004 | 25.11 | 10.39 |
| ω2Tlag | 0.021 | 0.007 | 31.96 | 21.39 |
| σ (μg/mL) | 0.189 | 0.017 | 9.02 | |
| Cis-cefprozil | ||||
| Base model | ||||
| tvV (mL) | 14,307.00 | 1182.54 | 8.27 | |
| tvCl (mL/h) | 17,111.30 | 456.71 | 2.67 | |
| tvTlag (h) | 0.352 | 0.014 | 3.91 | |
| tvKa (1/h) | 0.429 | 0.006 | 1.32 | |
| ω2V | 0.127 | 0.027 | 21.66 | 7.39 |
| ω2Cl | 0.019 | 0.005 | 26.58 | 9.02 |
| ω2Tlag | 0.021 | 0.007 | 33.09 | 21.28 |
| σ (μg/mL) | 0.193 | 0.016 | 8.41 | |
| Final model | ||||
| tvV (mL) | 14,308.10 | 1184.69 | 8.28 | |
| tvCl (mL/h) | 17,150.70 | 406.51 | 2.37 | |
| tvTlag (h) | 0.352 | 0.014 | 3.92 | |
| tvKa (1/h) | 0.429 | 0.006 | 1.33 | |
| dCldCrCl | 0.003 | 0.002 | 51.87 | |
| ω2V | 0.127 | 0.027 | 21.53 | 7.32 |
| ω2Cl | 0.016 | 0.004 | 24.57 | 10.48 |
| ω2Tlag | 0.021 | 0.007 | 33.25 | 21.23 |
| σ (μg/mL) | 0.193 | 0.016 | 8.40 | |
| Trans-cefprozil | ||||
| Final model | ||||
| tvV (mL) | 34,617.50 | 1997.67 | 5.77 | |
| tvCl (mL/h) | 17,701.80 | 598.23 | 3.38 | |
| tvTlag (h) | 0.352 | 0.018 | 5.09 | |
| tvKa (1/h) | 0.829 | 0.091 | 10.98 | |
| ω2Cl | 0.017 | 0.006 | 37.04 | 9.28 |
| ω2Tlag | 0.094 | 0.042 | 44.62 | 12.06 |
| ω2ka | 0.076 | 0.025 | 32.56 | 10.95 |
| σ | 0.232 | 0.015 | 6.61 |
| Parameter | Final Model | Bootstrap | ||
|---|---|---|---|---|
| Estimate | 95% CI | Median | 95% CI | |
| Total cefprozil | ||||
| tvV (mL) | 14,713.10 | 12,352.34–17,073.86 | 14,777.30 | 12,595.74–17,799.95 |
| tvCl (mL/h) | 17,226.20 | 16,429.46–18,022.94 | 17,233.30 | 16,418.17–18,051.63 |
| tvTlag (h) | 0.351 | 0.326–0.377 | 0.352 | 0.330–0.373 |
| tvKa (1/h) | 0.432 | 0.421–0.443 | 0.433 | 0.422–0.446 |
| dCldCrCl | 2.87 × 10−3 | −3.00 × 10−4–6.04 × 10−3 | 2.87 × 10−3 | −3.08 × 10−4–6.27 × 10−3 |
| ω2V | 0.124 | 0.072–0.176 | 0.121 | 0.065–0.177 |
| ω2Cl | 0.016 | 0.006–0.025 | 0.014 | 0.006–0.021 |
| ω2Tlag | 0.021 | 0.008–0.033 | 0.020 | 0.006–0.034 |
| σ (μg/mL) | 0.189 | 0.156–0.223 | 0.189 | 0.157–0.222 |
| Cis-cefprozil | ||||
| tvV (mL) | 143,08.10 | 11,978.18–16,638.02 | 14,406.04 | 12,334.79–17,164.45 |
| tvCl (mL/h) | 17,150.70 | 16,351.22–17,950.18 | 17,191.88 | 16,488.92–17,926.22 |
| tvTlag (h) | 0.352 | 0.325–0.379 | 0.354 | 0.323–0.378 |
| tvKa (1/h) | 0.429 | 0.418–0.440 | 0.429 | 0.420–0.442 |
| dCldCrCl | 3.04 × 10−3 | −6.10 × 10−5–6.15 × 10−3 | 3.06 × 10−3 | 7.24 × 10−5–6.04 × 10−3 |
| ω2V | 0.127 | 0.073–0.181 | 0.122 | 0.066–0.179 |
| ω2Cl | 0.016 | 0.006–0.026 | 0.015 | 0.007–0.023 |
| ω2Tlag | 0.021 | 0.007–0.034 | 0.021 | 0.006–0.035 |
| σ (μg/mL) | 0.193 | 0.161–0.225 | 0.193 | 0.163–0.225 |
| Trans-cefprozil | ||||
| tvV (mL) | 34,617.50 | 30,688.77–38,546.24 | 34,360.90 | 22,079.72–38,114.42 |
| tvCl (mL/h) | 17,701.80 | 16,525.29–18,878.31 | 17,636.80 | 16,492.77–18,807.66 |
| tvTlag (h) | 0.352 | 0.317–0.388 | 0.356 | 0.317–0.393 |
| tvKa (1/h) | 0.829 | 0.650–1.008 | 0.828 | 0.510–1.010 |
| ω2Cl | 0.017 | 0.005–0.029 | 0.018 | 0.001–0.035 |
| ω2Tlag | 0.094 | 0.012–0.177 | 0.108 | 0.007–0.222 |
| ω2ka | 0.076 | 0.028–0.125 | 0.071 | 0.014–0.128 |
| σ | 0.232 | 0.202–0.262 | 0.228 | 0.196–0.266 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, J.-H.; Jeong, S.-H.; Cho, H.-Y.; Lee, Y.-B. Population Pharmacokinetics of Cis-, Trans-, and Total Cefprozil in Healthy Male Koreans. Pharmaceutics 2019, 11, 531. https://doi.org/10.3390/pharmaceutics11100531
Jang J-H, Jeong S-H, Cho H-Y, Lee Y-B. Population Pharmacokinetics of Cis-, Trans-, and Total Cefprozil in Healthy Male Koreans. Pharmaceutics. 2019; 11(10):531. https://doi.org/10.3390/pharmaceutics11100531
Chicago/Turabian StyleJang, Ji-Hun, Seung-Hyun Jeong, Hea-Young Cho, and Yong-Bok Lee. 2019. "Population Pharmacokinetics of Cis-, Trans-, and Total Cefprozil in Healthy Male Koreans" Pharmaceutics 11, no. 10: 531. https://doi.org/10.3390/pharmaceutics11100531