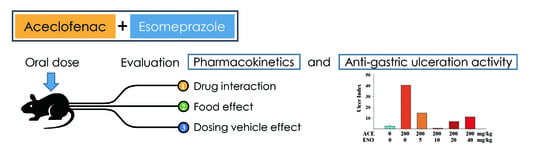
Pharmacokinetics and Anti-Gastric Ulceration Activity of Oral Administration of Aceclofenac and Esomeprazole in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Animals
2.3. Pharmacokinetic Studies
2.4. Measurement of Gastric Lesions
2.5. Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)
2.6. Non-Compartmental Analysis
2.7. Statistical Analysis
3. Results
3.1. Effects of Esomeprazole on Aceclofenac Induced Gastric Damage
3.2. Effects of Esomeprazole on Aceclofenac Pharmacokinetics
3.3. Effects of Different Dosing Vehicles on the Pharmacokinetics of Aceclofenac and Esomeprazole
3.4. Food Effects on the Pharmacokinetics of Aceclofenac and Esomeprazole
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ward, D.E.; Veys, E.M.; Bowdler, J.M.; Roma, J. Comparison of aceclofenac with diclofenac in the treatment of osteoarthritis. Clin. Rheumatol. 1995, 14, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Martin-Mola, E.; Gijon-Banos, J.; Ansoleaga, J.J. Aceclofenac in comparison to ketoprofen in the treatment of rheumatoid arthritis. Rheumatol. Int. 1995, 15, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Batlle-Gualda, E.; Figueroa, M.; Ivorra, J.; Raber, A. The efficacy and tolerability of aceclofenac in the treatment of patients with ankylosing spondylitis: A multicenter controlled clinical trial. Aceclofenac indomethacin study group. J. Rheumatol. 1996, 23, 1200–1206. [Google Scholar] [PubMed]
- Schattenkirchner, M.; Milachowski, K.A. A double-blind, multicentre, randomised clinical trial comparing the efficacy and tolerability of aceclofenac with diclofenac resinate in patients with acute low back pain. Clin. Rheumatol. 2003, 22, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Movilia, P.G. Evaluation of the analgesic activity and tolerability of aceclofenac in the treatment of post-episiotomy pain. Drugs Exp. Clin. Res. 1989, 15, 47–51. [Google Scholar] [PubMed]
- Noh, K.; Shin, B.S.; Kwon, K.I.; Yun, H.Y.; Kim, E.; Jeong, T.C.; Kang, W. Absolute bioavailability and metabolism of aceclofenac in rats. Arch. Pharm. Res. 2015, 38, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Bort, R.; Ponsoda, X.; Carrasco, E.; Gomez-Lechon, M.J.; Castell, J.V. Comparative metabolism of the nonsteroidal antiinflammatory drug, aceclofenac, in the rat, monkey, and human. Drug Metab. Dispos. 1996, 24, 969–975. [Google Scholar] [PubMed]
- Henrotin, Y.; de Leval, X.; Mathy-Hartet, M.; Mouithys-Mickalad, A.; Deby-Dupont, G.; Dogne, J.M.; Delarge, J.; Reginster, J.Y. In vitro effects of aceclofenac and its metabolites on the production by chondrocytes of inflammatory mediators. Inflamm. Res. 2001, 50, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Scheiman, J.M. Nsaids, gastrointestinal injury, and cytoprotection. Gastroenterol. Clin. North Am. 1996, 25, 279–298. [Google Scholar] [CrossRef]
- Dooley, M.; Spencer, C.M.; Dunn, C.J. Aceclofenac: A reappraisal of its use in the management of pain and rheumatic disease. Drugs 2001, 61, 1351–1378. [Google Scholar] [CrossRef] [PubMed]
- Perez-Ruiz, F.; Alonso-Ruiz, A.; Ansoleaga, J.J. Comparative study of the efficacy and safety of aceclofenac and tenoxicam in rheumatoid arthritis. Clin. Rheumatol. 1996, 15, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Diaz, C.; Rodriguez de la Serna, A.; Geli, C.; Gras, X. Efficacy and tolerability of aceclofenac versus diclofenac in the treatment of knee osteoarthritis: A multicentre study. Eur. J. Rheumatol. Inflamm. 1996, 16, 17–22. [Google Scholar]
- Pasero, G.; Marcolongo, R.; Serni, U.; Parnham, M.J.; Ferrer, F. A multi-centre, double-blind comparative study of the efficacy and safety of aceclofenac and diclofenac in the treatment of rheumatoid arthritis. Curr. Med. Res. Opin. 1995, 13, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Torri, G.; Vignati, C.; Agrifoglio, E.; Benvenuti, M.; Ceciliani, L.; Raschella, B.F.; Letizia, G.; Martorana, U.; Tessari, L.; Thovez, G.; et al. Aceclofenac versus piroxicam in the management of osteoarthritis of the knee: A double-blind controlled study. Curr. Ther. Res. 1994, 55, 576–583. [Google Scholar] [CrossRef]
- Pasero, G.; Ruju, G.; Marcolongo, R.; Senesi, M.; Seni, U.; Mannoni, A.; Accardo, S.; Seriolo, B.; Colombo, B.; Ligniere, G.C.; et al. Aceclofenac versus naproxen in the treatment of ankylosing spondylitis: A double-blind, controlled study. Curr. Ther. Res. 1994, 55, 833–842. [Google Scholar] [CrossRef]
- Perez Busquier, M.; Calero, E.; Rodriguez, M.; Castellon Arce, P.; Bermudez, A.; Linares, L.F.; Mesa, J.; Ffernandez Crisostomos, C.; Garcia, C.; Garcia Lopez, A.; et al. Comparison of aceclofenac with piroxicam in the treatment of osteoarthritis. Clin. Rheumatol. 1997, 16, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Kornasoff, D.; Frerick, H.; Bowdler, J.; Montull, E. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis. Clin. Rheumatol. 1997, 16, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Kornasoff, D.; Maisenbacher, J.; Bowdler, J.; Raber, A. The efficacy and tolerability of aceclofenac compared to indomethacin in patients with rheumatoid arthritis. Rheumatol. Int. 1996, 15, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Villa Alcazar, L.F.; de Buergo, M.; Rico Lenza, H.; Montull Fruitos, E. Aceclofenac is as safe and effective as tenoxicam in the treatment of ankylosing spondylitis: A 3 month multicenter comparative trial. Spanish study group on aceclofenac in ankylosing spondylitis. J. Rheumatol. 1996, 23, 1194–1199. [Google Scholar] [PubMed]
- Lanza, F.L.; Chan, F.K.; Quigley, E.M. Practice Parameters Committee of the American College of, G. Guidelines for prevention of nsaid-related ulcer complications. Am. J. Gastroenterol. 2009, 104, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, N.M.; Campbell, D.R.; Safdi, M.A.; Lukasik, N.L.; Huang, B.; Haber, M.M. Superiority of lansoprazole vs ranitidine in healing nonsteroidal anti-inflammatory drug-associated gastric ulcers: Results of a double-blind, randomized, multicenter study. Nsaid-associated gastric ulcer study group. Arch. Intern. Med. 2000, 160, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.L.; Johanson, J.F.; Suchower, L.J.; Brown, K.A. Healing of gastric ulcers with esomeprazole versus ranitidine in patients who continued to receive nsaid therapy: A randomized trial. Am. J. Gastroenterol. 2005, 100, 2650–2657. [Google Scholar] [CrossRef] [PubMed]
- Hawkey, C.; Talley, N.J.; Yeomans, N.D.; Jones, R.; Sung, J.J.; Langstrom, G.; Naesdal, J.; Scheiman, J.M.; Group, N.S.S. Improvements with esomeprazole in patients with upper gastrointestinal symptoms taking non-steroidal antiinflammatory drugs, including selective cox-2 inhibitors. Am. J. Gastroenterol. 2005, 100, 1028–1036. [Google Scholar] [CrossRef] [PubMed]
- Morgner, A.; Miehlke, S.; Labenz, J. Esomeprazole: Prevention and treatment of nsaid-induced symptoms and ulcers. Expert Opin. Pharmacother. 2007, 8, 975–988. [Google Scholar] [CrossRef] [PubMed]
- Scheiman, J.M.; Yeomans, N.D.; Talley, N.J.; Vakil, N.; Chan, F.K.; Tulassay, Z.; Rainoldi, J.L.; Szczepanski, L.; Ung, K.A.; Kleczkowski, D.; et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective nsaids and cox-2 inhibitors. Am. J. Gastroenterol. 2006, 101, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Lanas, A.; Polo-Tomas, M.; Roncales, P.; Gonzalez, M.A.; Zapardiel, J. Prescription of and adherence to non-steroidal anti-inflammatory drugs and gastroprotective agents in at-risk gastrointestinal patients. Am. J. Gastroenterol. 2012, 107, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Dries, A.M.; Richardson, P.; Cavazos, J.; Abraham, N.S. Therapeutic intent of proton pump inhibitor prescription among elderly nonsteroidal anti-inflammatory drug users. Aliment. Pharmacol. Ther. 2009, 30, 652–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrade, S.F.; Antoniolli, D.; Comunello, E.; Cardoso, L.G.V.; Carvalho, J.C.T.; Bastos, J.K. Antiulcerogenic activity of crude extract, fractions and populnoic acid isolated from austroplenckia populnea (celastraceae). Z. Naturforsch. C 2006, 61, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Adinortey, M.B.; Ansah, C.; Galyuon, I.; Nyarko, A. In vivo models used for evaluation of potential antigastroduodenal ulcer agents. Ulcers 2013, 2013, 12. [Google Scholar] [CrossRef]
- Fornai, M.; Colucci, R.; Antonioli, L.; Awwad, O.; Ugolini, C.; Tuccori, M.; Fulceri, F.; Natale, G.; Basolo, F.; Blandizzi, C. Effects of esomeprazole on healing of nonsteroidal anti-inflammatory drug (nsaid)-induced gastric ulcers in the presence of a continued nsaid treatment: Characterization of molecular mechanisms. Pharmacol. Res. 2011, 63, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Hibi, T. Novel effects other than antisecretory action and off-label use of proton pump inhibitors. Expert Opin. Pharmacother. 2005, 6, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Pastoris, O.; Verri, M.; Boschi, F.; Kastsiuchenka, O.; Balestra, B.; Pace, F.; Tonini, M.; Natale, G. Effects of esomeprazole on glutathione levels and mitochondrial oxidative phosphorylation in the gastric mucosa of rats treated with indomethacin. Naunyn Schmiedebergs Arch. Pharmacol. 2008, 378, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Metsugi, Y.; Miyaji, Y.; Ogawara, K.; Higaki, K.; Kimura, T. Appearance of double peaks in plasma concentration-time profile after oral administration depends on gastric emptying profile and weight function. Pharm. Res. 2008, 25, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Shin, S.; Landersdorfer, C.B.; Chi, Y.H.; Paik, S.H.; Myung, J.; Yadav, R.; Horkovics-Kovats, S.; Bulitta, J.B.; Shin, B.S. Population pharmacokinetic modeling of the enterohepatic recirculation of fimasartan in rats, dogs, and humans. AAPS J. 2015, 17, 1210–1223. [Google Scholar] [CrossRef] [PubMed]
- U.S. FDA, NDA 21-153/S-022: Nexium (esomeprazole magnesium) delayed-release capsules. 2001. Available online: http://www.accessdata.fda.gov/drugsatfda_docs/label/2006/021153s022lbl.pdf (accessed on 31 July 2018).
- Pilbrant, A.; Cederberg, C. Development of an oral formulation of omeprazole. Scand. J. Gastroenterol. Suppl. 1985, 108, 113–120. [Google Scholar] [CrossRef] [PubMed]





| Compound | Parameters | ACE 20/ESO 0 mg/kg (n = 4) | ACE 20/ESO 4 mg/kg (n = 6) | ACE 20/ESO 8 mg/kg (n = 4) |
|---|---|---|---|---|
| Aceclofenac | t1/2 (h) | 1.38 ± 0.21 | 0.94 ± 0.70 | 1.39 ± 0.72 |
| Tmax (h) | 0.23 ± 0.20 | 0.17 ± 0.07 | 0.19 ± 0.10 | |
| Cmax (μg/mL) | 3.07 ± 1.20 | 5.12 ± 1.66 | 5.72 ± 2.55 | |
| AUCall (μg·h/mL) | 2.30 ± 0.54 | 2.54 ± 0.51 | 2.79 ± 0.61 | |
| AUC∞ (μg·h/mL) | 2.36 ± 0.52 | 2.57 ± 0.51 | 2.83 ± 0.60 | |
| CL/F (mL/min/kg) | 146.80 ± 32.40 | 134.77 ± 32.32 | 121.94 ± 26.32 | |
| Diclofenac | t1/2 (h) | 3.84 ± 0.32 | 3.82 ± 1.65 | 3.24 ± 0.98 |
| Tmax (h) | 0.50 ± 0.30 | 0.28 ± 0.11 | 0.23 ± 0.08 | |
| Cmax (μg/mL) | 4.91 ± 3.19 | 10.76 ± 2.74 | 8.89 ± 4.98 | |
| AUCall (μg·h/mL) | 7.16 ± 1.98 | 9.44 ± 1.1 | 8.56 ± 3.32 | |
| AUC∞ (μg·h/mL) | 7.76 ± 2.13 | 10.1 ± 1.35 | 8.97 ± 3.24 | |
| AUCDIC/AUCACE | 3.94 ± 1.73 | 4.64 ± 1.32 | 3.63 ± 0.97 | |
| Esomeprazole | t1/2 (h) | - | 3.87 ± 2.21 | 5.67 ± 3.68 |
| Tmax (h) | - | 0.15 ± 0.14 | 0.13 ± 0.05 | |
| Cmax (μg/mL) | - | 57.14 ± 25.94 | 142.75 ± 132.71 | |
| AUCall (μg·h/mL) | - | 27.68 ± 13.39 | 64.02 ± 49.78 | |
| AUC∞ (μg·h/mL) | - | 30.91 ± 12.76 | 68.71 ± 48.72 | |
| CL/F (mL/min/kg) | - | 2442.37 ± 884.54 | 3087.76 ± 2334.25 |
| Compound | Parameters | Vehicle A (n = 5) | Vehicle B (n = 4) | Vehicle C (n = 6) | Vehicle D (n = 6) |
|---|---|---|---|---|---|
| Aceclofenac | t1/2 (h) a) | 2.13 ± 0.30 | 6.47 ± 5.59 | 0.94 ± 0.70 | 1.89 ± 1.65 |
| Tmax (h) | 0.57 ± 0.80 | 0.60 ± 0.93 | 0.17 ± 0.07 | 0.27 ± 0.21 | |
| Cmax (μg/mL) | 2.53 ± 0.57 | 0.69 ± 0.33 | 5.12 ± 1.66 | 21.69 ± 6.48 | |
| Cmax (μg/mL)/D (mg/kg) b) | 0.13 ± 0.03 | 0.03 ± 0.02 | 0.26 ± 0.08 | 0.11 ± 0.03 | |
| AUCall (μg·h/mL) | 3.35 ± 1.72 | 0.88 ± 0.82 | 2.54 ± 0.51 | 34.75 ± 9.82 | |
| AUCall (μg·h/mL)/D (mg/kg) c) | 0.37 ± 0.07 | 0.07 ± 0.06 | 0.47 ± 0.05 | 0.63 ± 0.23 | |
| AUC∞ (μg·h/mL) | 3.53 ± 1.89 | 1.42 ± 1.14 | 2.57 ± 0.51 | 38.16 ± 9.00 | |
| AUC∞ (μg·h/mL)/D (mg/kg) | 0.18 ± 0.09 | 0.07 ± 0.06 | 0.13 ± 0.03 | 0.19 ± 0.05 | |
| CL/F (mL/min/kg) | 116.07 ± 51.38 | 446.08 ± 358.98 | 134.77 ± 32.32 | 91.01 ± 23.36 | |
| Diclofenac | t1/2 (h) d) | 1.97 ± 0.35 | 3.04 ± 1.42 | 3.82 ± 1.65 | 5.57 ± 3.21 |
| Tmax (h) | 0.60 ± 0.78 | 0.69 ± 0.88 | 0.28 ± 0.11 | 1.33 ± 1.67 | |
| Cmax (μg/mL) | 5.98 ± 3.06 | 0.63 ± 0.28 | 10.76 ± 2.74 | 43.69 ± 14.61 | |
| AUCall (μg·h/mL) | 7.41 ± 1.35 | 1.46 ± 1.30 | 9.44 ± 1.10 | 125.81 ± 46.49 | |
| AUC∞ (μg·h/mL) | 7.51 ± 1.38 | 1.58 ± 1.44 | 10.1 ± 1.35 | 129.86 ± 44.66 | |
| AUCDIC/AUCACE a) | 3.04 ± 1.06 | 2.03 ± 0.24 | 4.64 ± 1.32 | 4.33 ± 0.85 | |
| Esomeprazole | t1/2 (h) | 1.69 ± 0.75 | 5.14 ± 5.30 | 3.87 ± 2.21 | 3.72 ± 0.38 |
| Tmax (h) | 1.80 ± 3.47 | 0.21 ± 0.08 | 0.15 ± 0.14 | 0.21 ± 0.08 | |
| Cmax (ng/mL) | 15.43 ± 3.36 | 13.54 ± 4.08 | 57.14 ± 25.94 | 319 ± 136.81 | |
| Cmax (ng/mL)/D (mg/kg) e) | 3.86 ± 0.84 | 3.39 ± 1.02 | 14.28 ± 6.49 | 15.95 ± 6.84 | |
| AUCall (ng·h/mL) | 33.83 ± 10.1 | 27.28 ± 6.43 | 27.68 ± 13.39 | 143.85 ± 48.71 | |
| AUCall (ng·h/mL)/D (mg/kg) | 8.46 ± 2.53 | 6.82 ± 1.61 | 6.92 ± 3.35 | 7.19 ± 2.44 | |
| AUC∞ (ng·h/mL) | 42.09 ± 19.27 | 37.03 ± 11.85 | 30.91 ± 12.76 | 151.35 ± 51.65 | |
| AUC∞ (ng·h/mL)/D (mg/kg) | 10.52 ± 4.82 | 9.26 ± 2.96 | 7.73 ± 3.19 | 7.57 ± 2.58 | |
| CL/F (mL/min/kg) | 1786.9 ± 670.64 | 1910.9 ± 518.68 | 2442.37 ± 884.54 | 2356.49 ± 602.56 |
| Compound | Parameters | Fasted (n = 5) | Fed (n = 4) |
|---|---|---|---|
| Aceclofenac | t1/2 (h) * | 2.13 ± 0.30 | 0.81 ± 0.21 |
| Tmax (h) | 0.57 ± 0.80 | 0.65 ± 0.91 | |
| Cmax (μg/mL) | 2.53 ± 0.57 | 2.27 ± 1.38 | |
| AUCall (μg·h/mL) | 3.35 ± 1.72 | 2.95 ± 0.41 | |
| AUC∞ (μg·h/mL) | 3.53 ± 1.89 | 2.97 ± 0.41 | |
| CL/F (mL/min/kg) | 116.07 ± 51.38 | 114.1 ± 17.25 | |
| Diclofenac | t1/2 (h) | 1.97 ± 0.35 | 2.22 ± 0.59 |
| Tmax (h) | 0.60 ± 0.78 | 0.69 ± 0.88 | |
| Cmax (μg/mL) | 5.98 ± 3.06 | 3.12 ± 1.91 | |
| AUCall (μg·h/mL) | 7.41 ± 1.35 | 6.36 ± 1.27 | |
| AUC∞ (μg·h/mL) | 7.51 ± 1.38 | 6.56 ± 1.31 | |
| AUCDIC/AUCACE | 3.04 ± 1.06 | 2.57 ± 0.27 | |
| Esomeprazole | t1/2 (h) * | 1.69 ± 0.75 | 3.18 ± 1.02 |
| Tmax (h) | 1.80 ± 3.47 | 0.40 ± 0.29 | |
| Cmax (ng/mL) * | 15.43 ± 3.36 | 4.84 ± 0.94 | |
| AUCall (ng·h/mL) * | 33.83 ± 10.10 | 13.96 ± 4.82 | |
| AUC∞ (ng·h/mL) | 42.09 ± 19.27 | 17.26 ± 4.42 | |
| CL/F (mL/min/kg) | 1786.9 ± 670.64 | 4061.35 ± 1041.26 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, T.H.; Thapa, S.K.; Lee, D.Y.; Chung, S.E.; Lim, J.Y.; Jeong, H.M.; Song, C.H.; Choi, Y.-W.; Cho, S.-M.; Nam, K.-Y.; et al. Pharmacokinetics and Anti-Gastric Ulceration Activity of Oral Administration of Aceclofenac and Esomeprazole in Rats. Pharmaceutics 2018, 10, 152. https://doi.org/10.3390/pharmaceutics10030152
Kim TH, Thapa SK, Lee DY, Chung SE, Lim JY, Jeong HM, Song CH, Choi Y-W, Cho S-M, Nam K-Y, et al. Pharmacokinetics and Anti-Gastric Ulceration Activity of Oral Administration of Aceclofenac and Esomeprazole in Rats. Pharmaceutics. 2018; 10(3):152. https://doi.org/10.3390/pharmaceutics10030152
Chicago/Turabian StyleKim, Tae Hwan, Subindra Kazi Thapa, Da Young Lee, Seung Eun Chung, Jun Young Lim, Hyeon Myeong Jeong, Chang Ho Song, Youn-Woong Choi, Sang-Min Cho, Kyu-Yeol Nam, and et al. 2018. "Pharmacokinetics and Anti-Gastric Ulceration Activity of Oral Administration of Aceclofenac and Esomeprazole in Rats" Pharmaceutics 10, no. 3: 152. https://doi.org/10.3390/pharmaceutics10030152