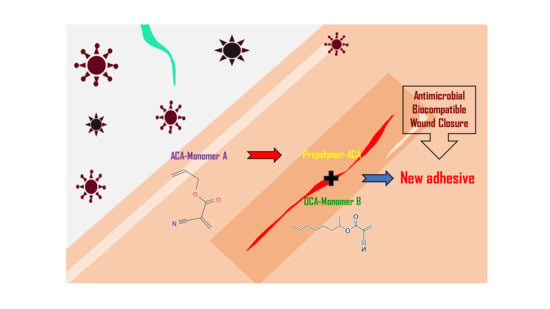
Antimicrobial Activity and Cytotoxicity of Prepolymer Allyl 2-cyanoacrylate and 2-Octyl Cyanoacrylate Mixture Adhesives for Topical Wound Closure
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Cells
2.3. Disc Diffusion Test for Antimicrobial Activity
2.4. MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium Bromide) Assay for Cytotoxicity Assessment
2.5. Determination of Formaldehyde Content in Skin Adhesive Samples
2.6. Statistical Analysis
3. Results
3.1. Antimicrobial Activity of PAC in Different Concentration
3.2. In Vitro Cytotoxicity of Skin Adhesive Samples
3.3. Quantitative Analysis of Formaldehyde from Skin Adhesive Samples
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunt, T.K.; Hopf, H.; Hussain, Z. Physiology of wound healing. Adv. Skin Wound Care 2000, 13 (Suppl. S2), 6–11. [Google Scholar] [CrossRef] [PubMed]
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.; Eccleston, G.M. Wound healing dressings and drug delivery systems: A review. J. Pharm. Sci. 2008, 97, 2892–2923. [Google Scholar] [CrossRef] [PubMed]
- Sarabahi, S. Recent advances in topical wound care. Indian J. Plast. Surg. 2012, 45, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Vanholder, R.; Misotten, A.; Roels, H.; Matton, G. Cyanoacrylate tissue adhesive for closing skin wounds: A double blind randomized comparison with sutures. Biomaterials 1993, 14, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Tseng, Y.-C.; Hyon, S.-H.; Ikada, Y.; Shimizu, Y.; Tamura, K.; Hitomi, S. In vivo evaluation of 2-cyanoacrylates as surgical adhesives. J. Appl. Biomater. 1990, 1, 111–119. [Google Scholar] [CrossRef]
- Leggat, P.A.; Smith, D.R.; Kedjarune, U. Surgical applications of cyanoacrylate adhesives: A review of toxicity. ANZ J. Surg. 2007, 77, 209–213. [Google Scholar] [CrossRef]
- Echániz, J.S.; Fernández, J.B.; Raso, S.M.; Ronco, M.A.V. Cyanoacrylates: Another way to repair wounds. An. Esp. Pediatr. 2000, 53, 288–289. [Google Scholar]
- Korde, J.M.; Kandasubramanian, B. Biocompatible alkyl cyanoacrylates and their derivatives as bio-adhesives. Biomater. Sci. 2018, 6, 1691–1711. [Google Scholar] [CrossRef]
- Valji, K. Cyanoacrylates for embolization in gastrointestinal bleeding: How super is glue? J. Vasc. Interv. Radiol. 2014, 25, 20–21. [Google Scholar] [CrossRef]
- Lim, J.I.; Kim, J.H. Enhanced biocompatibility and adhesive properties of modified allyl 2-cyanoacrylate-based elastic bio-glues. Colloids Surf. B Biointerfaces 2015, 133, 19–23. [Google Scholar] [CrossRef]
- Lim, J.I.; Lee, W.K. Enhanced biocompatibility and adhesive properties by aromatic amino acid-modified allyl 2-cyanoacrylate-based bio-glue. Colloids Surf. B Biointerfaces 2014, 122, 669–673. [Google Scholar] [CrossRef] [PubMed]
- Shivamurthy, D.M.; Singh, S.; Reddy, S. Comparison of octyl-2-cyanoacrylate and conventional sutures in facial skin closure. Natl. J. Maxillofac. Surg. 2010, 1, 15–19. [Google Scholar] [PubMed]
- Rushbrook, J.L.; White, G.; Kidger, L.; Marsh, P.; Taggart, T.F. The antibacterial effect of 2-octyl cyanoacrylate (Dermabond®) skin adhesive. J. Infect. Prev. 2014, 15, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Eiferman, R.A.; Snyder, J.W. Antibacterial effect of cyanoacrylate glue. Arch. Ophthalmol. 1983, 101, 958–960. [Google Scholar] [CrossRef]
- Lee, Y.J.; Son, H.S.; Jung, G.B.; Kim, J.H.; Choi, S.; Lee, G.-J.; Park, H.-K. Enhanced biocompatibility and wound healing properties of biodegradable polymer-modified allyl 2-cyanoacrylate tissue adhesive. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 51, 43–50. [Google Scholar] [CrossRef]
- Grisdale, J. The use of cyanoacrylates in periodontal therapy. J. Can. Dent. Assoc. 1998, 64, 632–633. [Google Scholar]
- Kilpikari, J.; Lapinsuo, M.; Törmälä, P.; Pätiälä, H.; Rokkanen, P. Bonding strength of alkyl-2-cyanoacrylates to bone in vitro. J. Biomed. Mater. Res. 1986, 20, 1095–1102. [Google Scholar] [CrossRef]
- Samakh, P.; Sitbon, M.; Girard, P. The cyanoacrylates. Inf. Dent. 1978, 60, 25–31. [Google Scholar]
- Misic, A.M.; Gardner, S.E.; Grice, E.A. The Wound Microbiome: Modern Approaches to Examining the Role of Microorganisms in Impaired Chronic Wound Healing. Adv. Wound Care 2014, 3, 502–510. [Google Scholar] [CrossRef]
- Scales, B.S.; Huffnagle, G.B. The microbiome in wound repair and tissue fibrosis. J. Pathol. 2013, 229, 323–331. [Google Scholar] [CrossRef]
- Bot, G.M.; Bot, K.G.; Ogunranti, J.O.; Onah, J.A.; Sule, A.Z.; Hassan, I.; Dung, E.D. The use of cyanoacrylate in surgical anastomosis: An alternative to microsurgery. J. Surg. Tech. Case Rep. 2010, 2, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C. Perkinelmer Application note. 2009. Available online: https://www.perkinelmer.com/lab-solutionsresources/docs/APP/FormaldehydeInToysUVVis.pdf(accessed on 10 February 2023).
- Biemer, J.J. Antimicrobial susceptibility testing by the Kirby-Bauer disc diffusion method. Ann. Clin. Lab. Sci. 1973, 3, 135–140. [Google Scholar] [PubMed]
- Sergent, A.-P.; Slekovec, C.; Pauchot, J.; Jeunet, L.; Bertrand, X.; Hocquet, D.; Pazart, L.; Talon, D. Bacterial contamination of the hospital environment during wound dressing change. Orthop. Traumatol. Surg. Res. 2012, 98, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Hida, R.Y.; Silva, C.B.; Romero-Kusabara, I.L.; Mimica, L.M.J. Short-chain cyanoacrylates and long-chain cyanoacrylates (Dermabond) have different antimicrobial effects. BMJ Open Ophthalmol. 2021, 6, e000591. [Google Scholar] [CrossRef] [PubMed]
- Lehman, R.A.; Hayes, G.J.; Leonard, F. Toxicity of alkyl 2-cyanoacrylates. I. Peripheral nerve. Arch. Surg. 1966, 93, 441–446. [Google Scholar] [CrossRef]
- Lehman, R.A.; West, R.L.; Leonard, F. Toxicity of alkyl 2-cyanoacrylates. II. Bacterial growth. Arch. Surg. 1966, 93, 447–450. [Google Scholar] [CrossRef]
- Romero, I.L.; Malta, J.B.; Silva, C.B.; Mimica, L.M.; Soong, K.H.; Hida, R.Y. Antibacterial properties of cyanoacrylate tissue adhesive: Does the polymerization reaction play a role? Indian J. Ophthalmol. 2009, 57, 341–344. [Google Scholar] [CrossRef]
- Gefen, O.; Chekol, B.; Strahilevitz, J.; Balaban, N.Q. TDtest: Easy detection of bacterial tolerance and persistence in clinical isolates by a modified disk-diffusion assay. Sci. Rep. 2017, 7, 41284. [Google Scholar] [CrossRef]
- Jandinski, J.; Sonis, S. In vitro effects of isobutyl cyanocrylate on four types of bacteria. J. Dent. Res. 1971, 50, 1557–1558. [Google Scholar] [CrossRef]
- Lu, M.-M.; Bai, J.; Shao, D.; Qiu, J.; Li, M.; Zheng, X.; Xiao, Y.; Wang, Z.; Chang, Z.-M.; Chen, L.; et al. Antibacterial and biodegradable tissue nano-adhesives for rapid wound closure. Int. J. Nanomed. 2018, 13, 5849–5863. [Google Scholar] [CrossRef]
- Boyd, A.; Chakrabarty, A.M. Pseudomonas aeruginosa biofilms: Role of the alginate exopolysaccharide. J. Ind. Microbiol. 1995, 15, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Vena, A.; Croxatto, A.; Righi, E.; Guery, B. How to manage Pseudomonas aeruginosa infections. Drugs Context 2018, 7, 212527. [Google Scholar] [CrossRef] [PubMed]
- Menichetti, F.; Falcone, M.; Lopalco, P.; Tascini, C.; Pan, A.; Busani, L.; Viaggi, B.; Rossolini, G.M.; Arena, F.; Novelli, A.; et al. The GISA call to action for the appropriate use of antimicrobials and the control of antimicrobial resistance in Italy. Int. J. Antimicrob. Agents 2018, 52, 127–134. [Google Scholar] [CrossRef]
- Mensa, J.; Barberán, J.; Soriano, A.; Llinares, P.; Marco, F.; Cantón, R.; Bou, G.; Del Castillo, J.G.; Maseda, E.; Azanza, J.R.; et al. Antibiotic selection in the treatment of acute invasive infections by Pseudomonas aeruginosa: Guidelines by the Spanish Society of Chemotherapy. Rev. Esp. Quimioter. 2018, 31, 78–100. [Google Scholar] [PubMed]
- Ammons, M.C.B.; Ward, L.S.; Fisher, S.T.; Wolcott, R.D.; James, G.A. In vitro susceptibility of established biofilms composed of a clinical wound isolate of Pseudomonas aeruginosa treated with lactoferrin and xylitol. Int. J. Antimicrob. Agents 2009, 33, 230–236. [Google Scholar] [CrossRef]
- Katsikogianni, M.; Missirlis, Y.F. Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. Eur. Cell Mater. 2004, 8, 37–57. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Jung, G.B.; Choi, S.; Lee, G.; Kim, J.H.; Son, H.S.; Bae, H.; Park, H.-K. Biocompatibility of a novel cyanoacrylate based tissue adhesive: Cytotoxicity and biochemical property evaluation. PLoS ONE 2013, 8, e79761. [Google Scholar] [CrossRef]
- Herro, E.M.; Friedlander, S.F.; Jacob, S.E. Bra-associated allergic contact dermatitis: P-tert-butylphenol formaldehyde resin as the culprit. Pediatr. Dermatol. 2012, 29, 540–541. [Google Scholar] [CrossRef]
- Herro, E.M.; Jacob, S.E. Allergic contact dermatitis to p-tert butylphenol formaldehyde resin in a continuous positive airway pressure strap. Dermatitis 2012, 23, 125–126. [Google Scholar] [CrossRef]
- Mak, K.; Manji, A.; Gallant-Behm, C.; Wiebe, C.; Hart, D.A.; Larjava, H.; Häkkinen, L. Scarless healing of oral mucosa is characterized by faster resolution of inflammation and control of myofibroblast action compared to skin wounds in the red Duroc pig model. J. Dermatol. Sci. 2009, 56, 168–180. [Google Scholar] [CrossRef]
- Rognoni, E.; Pisco, A.O.; Hiratsuka, T.; Sipilä, K.H.; Belmonte, J.M.; Mobasseri, S.A.; Philippeos, C.; Dilão, R.; Watt, F.M. Fibroblast state switching orchestrates dermal maturation and wound healing. Mol. Syst. Biol. 2018, 14, e8174. [Google Scholar] [CrossRef] [PubMed]
- Szende, B.; Tyihak, E. Effect of formaldehyde on cell proliferation and death. Cell Biol. Int. 2010, 34, 1273–1282. [Google Scholar] [CrossRef] [PubMed]


| Sample Name | Composition and Formulating Ratios | ||
|---|---|---|---|
| 2-Octyl Cyanoacrylate (OC) | Prepolymer Allyl 2-Cyanoacrylate (PAC) | Additives | |
| OC | 100% | 0% | 0% |
| PAC | 0% | 100% | 0% |
| PAC7 | 0% | 70% | 30% |
| PAC4 | 30% | 40% | 30% |
| PAC3 | 40% | 30% | 30% |
| Microorganisms | Skin Adhesive Samples | ||||
|---|---|---|---|---|---|
| OC | PAC | PAC7 | PAC4 | PAC3 | |
| Droplet | Droplet | Droplet | Droplet | Droplet | |
| Escherichia coli | − | + | + | − | − |
| Pseudomonas aeruginosa | − | − | − | − | − |
| Staphylococcus aureus | − | ++ | ++ | +++ | + |
| Candida albicans | − | + | + | ++ | + |
| Microorganisms | Skin Adhesive Samples | ||||
|---|---|---|---|---|---|
| OC | PAC | PAC7 | PAC4 | PAC3 | |
| Pellet | Pellet | Pellet | Pellet | Pellet | |
| Escherichia coli | − | + | + | − | − |
| Pseudomonas aeruginosa | − | − | − | − | − |
| Staphylococcus aureus | − | ++ | ++ | ++ | + |
| Candida albicans | − | + | + | + | + |
| PAC7 | PAC4 | |
|---|---|---|
| Formaldehyde conc. (ppm) | 0.026 | 0.017 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, S.; Hahm, D.-H.; Choi, Y.-B. Antimicrobial Activity and Cytotoxicity of Prepolymer Allyl 2-cyanoacrylate and 2-Octyl Cyanoacrylate Mixture Adhesives for Topical Wound Closure. Materials 2023, 16, 3427. https://doi.org/10.3390/ma16093427
Oh S, Hahm D-H, Choi Y-B. Antimicrobial Activity and Cytotoxicity of Prepolymer Allyl 2-cyanoacrylate and 2-Octyl Cyanoacrylate Mixture Adhesives for Topical Wound Closure. Materials. 2023; 16(9):3427. https://doi.org/10.3390/ma16093427
Chicago/Turabian StyleOh, Soyeon, Dae-Hyun Hahm, and Yong-Bok Choi. 2023. "Antimicrobial Activity and Cytotoxicity of Prepolymer Allyl 2-cyanoacrylate and 2-Octyl Cyanoacrylate Mixture Adhesives for Topical Wound Closure" Materials 16, no. 9: 3427. https://doi.org/10.3390/ma16093427