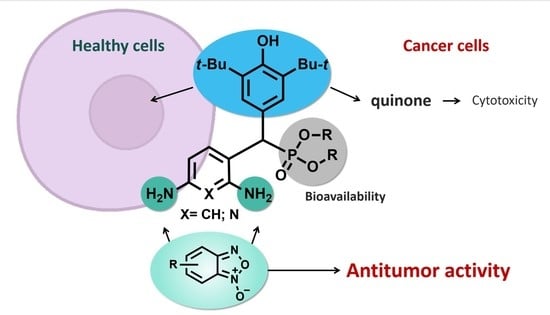
Diverse Biological Activity of Benzofuroxan/Sterically Hindered Phenols Hybrids
Abstract
:1. Introduction
2. Results and Discussion
2.1. Chemistry
2.2. Biological Evaluation
2.2.1. Anticancer Activity
2.2.2. Antimicrobial Activity
3. Materials and Methods
3.1. Chemistry













3.2. Biology
3.2.1. Cells and Materials
3.2.2. Cytotoxicity Assay
3.2.3. Flow Cytometry Assay
3.2.4. Antimicrobial Activity
3.2.5. Statistical Analysis
3.3. Biostability Studies
3.3.1. Preparation of Spikes and Samples
3.3.2. Apparatus and LC-MS/MS Conditions
3.4. Computations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Wild, C.P.; Weiderpass, E.; Stewart, B.W. (Eds.) World Cancer Report: Cancer Research for Cancer Prevention; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Gonzalez, F.J. Role of cytochromes P450 in chemical toxicity and oxidative stress: Studies with CYP2E1. Mutat. Res. Mol. Mech. Mutagen. 2005, 569, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B. Oxidative stress and cancer: Have we moved forward? Biochem. J. 2007, 401, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Policastro, L.L.; Ibañez, I.L.; Notcovich, C.; Duran, H.A.; Podhajcer, O.L. The Tumor Microenvironment: Characterization, Redox Considerations, and Novel Approaches for Reactive Oxygen Species-Targeted Gene Therapy. Antioxid. Redox Signal. 2013, 19, 854–895. [Google Scholar] [CrossRef]
- Sotgia, F.; Martinez-Outschoorn, U.E.; Lisanti, M.P. Mitochondrial oxidative stress drives tumor progression and metastasis: Should we use antioxidants as a key component of cancer treatment and prevention? BMC Med. 2011, 9, 62. [Google Scholar] [CrossRef] [Green Version]
- Popovici, V.; Musuc, A.M.; Matei, E.; Karampelas, O.; Ozon, E.A.; Cozaru, G.C.; Schröder, V.; Bucur, L.; Aricov, L.; Anastasescu, M.; et al. ROS-Induced DNA-Damage and Autophagy in Oral Squamous Cell Carcinoma by Usnea barbata Oil Extract—An In Vitro Study. Int. J. Mol. Sci. 2022, 23, 14836. [Google Scholar] [CrossRef] [PubMed]
- Milaeva, E.R.; Shpakovsky, D.B.; Gracheva, Y.A.; Antonenko, T.A.; Osolodkin, D.I.; Palyulin, V.A.; Shevtsov, P.N.; Neganova, M.E.; Vinogradova, D.V.; Shevtsova, E.F. Some insight into the mode of cytotoxic action of organotin compounds with protective 2,6-di-tert-butylphenol fragments. J. Organomet. Chem. 2015, 782, 96–102. [Google Scholar] [CrossRef]
- Milaeva, E.R.; Shpakovsky, D.B.; Dodokhova, M.A.; Kotieva, I.M.; Safronenko, A.V.; Alkhusein-Kulyaginova, M.S. Means for inhibiting metastasis in the lungs. Patent Ru 2762730, 22 December 2021. [Google Scholar]
- Milaeva, E.R.; Shpakovsky, D.B.; Dodokhova, M.A.; Kotieva, I.M.; Safronenko, A.V.; Alkhusein-Kulyaginova, M.S. Means for inhibiting metastasis in the lungs. Patent Ru 2765955, 7 February 2022. [Google Scholar]
- Edwards, C.M.; Mueller, G.; Roelofs, A.J.; Chantry, A.; Perry, M.; Russell, R.G.G.; Van Camp, B.; Guyon-Gellin, Y.; Niesor, E.J.; Bentzen, C.L.; et al. ApomineTM, an inhibitor of HMG-CoA-reductase, promotes apoptosis of myeloma cells in vitro and is associated with a modulation of myeloma in vivo. Int. J. Cancer 2007, 120, 1657–1663. [Google Scholar] [CrossRef]
- Mil’, E.M.; Erokhin, V.N.; Binyukov, V.I.; Albantova, A.A.; Volod’kin, A.A.; Goloshchapov, A.N. Apoptotic effect of the anphen sodium antioxidant in combination with H2O2 on Lewis carcinoma cells. Russ. Chem. Bull. 2019, 68, 2359–2364. [Google Scholar] [CrossRef]
- Hochdörffer, K.; Abu Ajaj, K.; Schäfer-Obodozie, C.; Kratz, F. Development of novel bisphosphonate prodrugs of doxorubicin for targeting bone metastases that are cleaved pH dependently or by cathepsin B: Synthesis, cleavage properties, and binding properties to hydroxyapatite as well as bone matrix. J. Med. Chem. 2012, 55, 7502–7515. [Google Scholar] [CrossRef]
- Orsini, F.; Sello, G.; Sisti, M. Aminophosphonic Acids and Derivatives. Synthesis and Biological Applications. Curr. Med. Chem. 2010, 17, 264–289. [Google Scholar] [CrossRef]
- Huang, X.; Huang, R.; Gou, S.; Wang, Z.; Wang, H. Anticancer Platinum(IV) Prodrugs Containing Monoaminophosphonate Ester as a Targeting Group Inhibit Matrix Metalloproteinases and Reverse Multidrug Resistance. Bioconjug. Chem. 2017, 28, 1305–1323. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.M.; Bordwell, F.G. Equilibrium acidities and homolytic bond dissociation energies of the acidic carbon-hydrogen bonds in P-substituted triphenylphosphonium cations. J. Am. Chem. Soc. 1994, 116, 968–972. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Xu, C.; Huang, J.; Wang, C.; Wang, X.; He, L.; Ling, Y. Synthesis and biological evaluation of nitric oxide-releasing hybrids from gemcitabine and phenylsulfonyl furoxans as anti-tumor agents. Medchemcomm 2015, 6, 1130–1136. [Google Scholar] [CrossRef]
- Fershtat, L.L.; Makhova, N.N. Molecular Hybridization Tools in the Development of Furoxan-Based NO-Donor Prodrugs. ChemMedChem 2017, 12, 622–638. [Google Scholar] [CrossRef]
- Aguirre, G.; Boiani, M.; Cerecetto, H.; Fernández, M.; González, M.; León, E.; Pintos, C.; Raymondo, S.; Arredondo, C.; Pacheco, J.P.; et al. Furoxan derivatives as cytotoxic agents: Preliminary in vivo antitumoral activity studies. Pharmazie 2006, 61, 54–59. [Google Scholar]
- Medana, C.; Ermondi, G.; Fruttero, R.; Di Stilo, A.; Ferretti, C.; Gasco, A. Furoxans as Nitric Oxide Donors. 4-Phenyl-3-furoxancarbonitrile: Thiol-Mediated Nitric Oxide Release and Biological Evaluation. J. Med. Chem. 1994, 37, 4412–4416. [Google Scholar] [CrossRef]
- Ghosh, P.B.; Whitehouse, M.W. Potential antileukemic and immunosuppressive drugs. Preparation and in vitro pharmacological acitivity of some benzo-2,1,3-oxadiazoles (benzofurazans) and their N-oxides (benzofuroxans). J. Med. Chem. 1968, 11, 305–311. [Google Scholar] [CrossRef]
- Whitehouse, M.W.; Ghosh, P.B. 4-nitrobenzofurazans and 4-nitrobenzofuroxans: A new class of thiol-neutralising agents and potent inhibitors of nucleic acid synthesis in leucocytes. Biochem. Pharmacol. 1968, 17, 158–161. [Google Scholar] [CrossRef]
- Ghosh, P.; Whitehouse, M. Potential Antileukemic and Immunosuppressive Drugs. II. Further Studies with Benzo-2,1,3-oxadiazoles (Benzofurazans) and Their N-Oxides (Benzofuroxans). J. Med. Chem. 1969, 12, 505–507. [Google Scholar] [CrossRef]
- Ghosh, P.B.; Ternai, B.; Whitehouse, M.W. Potential antileukemic and immunosuppressive drugs. 3. Effects of homocyclic ring substitution on the in vitro drug activity of 4-nitrobenzo-2,1,3-oxadiazoles (4-nitrobenzofurazans) and their N-oxides (4-nitrobenzofuroxans). J. Med. Chem. 1972, 15, 255–260. [Google Scholar] [CrossRef]
- Hay, M.P.; Wilson, W.R.; Moselen, J.W.; Palmer, B.D.; Denny, W.A. Hypoxia-selective antitumor agents. 8. Bis(nitroimidazolyl)alkanecarboxamides: A new class of hypoxia-selective cytotoxins and hypoxic cell radiosensitisers. J. Med. Chem. 1994, 37, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Wink, D.A.; Kasprzak, K.S.; Maragos, C.M.; Elespuru, R.K.; Misra, M.; Dunams, T.M.; Cebula, T.A.; Koch, W.H.; Andrews, A.W.; Allen, J.S.; et al. DNA deaminating ability and genotoxicity of nitric oxide and its progenitors. Science 1991, 254, 1001–1003. [Google Scholar] [CrossRef] [PubMed]
- Kessel, D.; Belton, J.G. Effects of 4-nitrobenzofurazans and their N-oxides on synthesis of protein and nucleic acid by murine leukemia cells. Cancer Res. 1975, 35, 3735–3740. [Google Scholar] [PubMed]
- Thompson, S.; Kellicutt, L. Mutagenicity of anti-cancer nitrobenzofuroxans. Mutat. Res. Mol. Mech. Mutagen. 1977, 48, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Macphee, D.G.; Robert, G.P.; Ternai, B.; Ghosh, P.; Stephens, R. Mutagenesis by 4-nitrobenzofurazans and furoxans. Chem. Biol. Interact. 1977, 19, 77–90. [Google Scholar] [CrossRef]
- Belton, J.G.; Conalty, M.L.; O’Sullivan, J.F. Anticancer agents—XI. Antitumour activity of 4-amino-7-nitrobenzofuroxans and related compounds. Proc. R. Ir. Acad. B 1976, 76, 133–149. [Google Scholar] [PubMed]
- Cerecetto, H.; Porcal, W. Pharmacological properties of furoxans and benzofuroxans: Recent developments. Mini Rev. Med. Chem. 2005, 5, 57–71. [Google Scholar] [CrossRef]
- Chugunova, E.A.A.; Gazizov, A.S.S.; Burilov, A.R.R.; Yusupova, L.M.M.; Pudovik, M.A.A.; Sinyashin, O.G.G. Benzofuroxans: Their synthesis, properties, and biological activity. Russ. Chem. Bull. 2019, 68, 887–910. [Google Scholar] [CrossRef]
- Chugunova, E.A.; Mukhamatdinova, R.E.; Sazykina, M.A.; Sazykin, I.S.; Khammami, M.I.; Akylbekov, N.I.; Burilov, A.R.; Kulik, N.V.; Zobov, V.V. Synthesis and biological activity of new hybrids compounds derived from benzofuroxanes and polyene antibiotics. Russ. J. Gen. Chem. 2016, 86, 1037–1040. [Google Scholar] [CrossRef]
- Wang, L.; Li, C.; Zhang, Y.; Qiao, C. Synthesis and Biological Evaluation of Benzofuroxan Derivatives as Fungicides against Phytopathogenic Fungi. J. Agric. Food Chem. 2013, 61, 8632–8640. [Google Scholar] [CrossRef]
- Jorge, S.D.; Masunari, A.; Rangel-Yagui, C.O.; Pasqualoto, K.F.M.; Tavares, L.C. Design, synthesis, antimicrobial activity and molecular modeling studies of novel benzofuroxan derivatives against Staphylococcus aureus. Bioorg. Med. Chem. 2009, 17, 3028–3036. [Google Scholar] [CrossRef]
- Gibadullina, E.; Nguyen, T.T.; Strelnik, A.; Sapunova, A.; Voloshina, A.; Sudakov, I.; Vyshtakalyuk, A.; Voronina, J.; Pudovik, M.; Burilov, A. New 2,6-diaminopyridines containing a sterically hindered benzylphosphonate moiety in the aromatic core as potential antioxidant and anti-cancer drugs. Eur. J. Med. Chem. 2019, 184, 111735. [Google Scholar] [CrossRef] [PubMed]
- Hammick, D.L.; Edwakdes, W.A.M.; Steiner, E.R. The constitution of benzfurazan and benzfurazan oxide. J. Chem. Soc. 1931, 0, 3308–3313. [Google Scholar] [CrossRef]
- Bailey, A.S.; Case, J.R. 4:6-dinitrobenzofuroxan, nitrobenzodifuroxan and benzotrifuroxan: A new series of complex-forming reagents for aromatic hydrocarbons. Tetrahedron 1958, 3, 113–131. [Google Scholar] [CrossRef]
- Botlton, A.J.; Ghosh, P.B. Benzofuroxans. In Advances in Heterocyclic Chemistry; Katritzky, A.R., Boulton, A.J., Eds.; Academic Press: London, UK, 1969; Volume 10, pp. 1–41. ISBN 9780120206100. [Google Scholar]
- Chugunova, E.; Akylbekov, N.; Shakirova, L.; Dobrynin, A.; Syakaev, V.; Latypov, S.; Bukharov, S.; Burilov, A. Synthesis of hybrids of benzofuroxan and N-, S-containing sterically hindered phenols derivatives. Tautomerism. Tetrahedron 2016, 72, 6415–6420. [Google Scholar] [CrossRef]
- Salah Ayoup, M.; Wahby, Y.; Abdel-Hamid, H.; Ramadan, E.S.; Teleb, M.; Abu-Serie, M.M.; Noby, A. Design, synthesis and biological evaluation of novel α-acyloxy carboxamides via Passerini reaction as caspase 3/7 activators. Eur. J. Med. Chem. 2019, 168, 340–356. [Google Scholar] [CrossRef]
- Tramer, F.; Da Ros, T.; Passamonti, S. Screening of fullerene toxicity by hemolysis assay. Methods Mol. Biol. 2012, 926, 203–217. [Google Scholar] [CrossRef]
- Voloshina, A.D.; Gumerova, S.K.; Sapunova, А.S.; Kulik, N.V.; Mirgorodskaya, A.B.; Kotenko, A.A.; Prokopyeva, T.M.; Mikhailov, V.A.; Zakharova, L.Y.; Sinyashin, O.G. The structure—Activity correlation in the family of dicationic imidazolium surfactants: Antimicrobial properties and cytotoxic effect. Biochim. Biophys. Acta Gen. Subj. 2020, 1864, 129728. [Google Scholar] [CrossRef]
- Voloshina, A.D.; Sapunova, A.S.; Kulik, N.V.; Belenok, M.G.; Strobykina, I.Y.; Lyubina, A.P.; Gumerova, S.K.; Kataev, V.E. Antimicrobial and cytotoxic effects of ammonium derivatives of diterpenoids steviol and isosteviol. Bioorg. Med. Chem. 2021, 32, 115974. [Google Scholar] [CrossRef]
- Neganova, M.; Aleksandrova, Y.; Suslov, E.; Mozhaitsev, E.; Munkuev, A.; Tsypyshev, D.; Chicheva, M.; Rogachev, A.; Sukocheva, O.; Volcho, K.; et al. Novel Multitarget Hydroxamic Acids with a Natural Origin CAP Group against Alzheimer’s Disease: Synthesis, Docking and Biological Evaluation. Pharmaceutics 2021, 13, 1893. [Google Scholar] [CrossRef]
- Norris, W.P.; Chafin, A.; Spear, R.J.; Read, R.W. Synthesis and thermal rearrangement of 5-chloro-4,6-dinitrobenzofuroxan. Heterocycles 1984, 22, 271–274. [Google Scholar] [CrossRef]
- Smolobochkin, A.V.; Gazizov, A.S.; Yakhshilikova, L.J.; Bekrenev, D.D.; Burilov, A.R.; Pudovik, M.A.; Lyubina, A.P.; Amerhanova, S.K.; Voloshina, A.D. Synthesis and Biological Evaluation of Taurine-Derived Diarylmethane and Dibenzoxanthene Derivatives as Possible Cytotoxic and Antimicrobial Agents. Chem. Biodivers. 2022, 19, e202100970. [Google Scholar] [CrossRef]
- Yu Strobykina, I.; Voloshina, A.D.; Andreeva, O.V.; Sapunova, A.S.; Lyubina, A.P.; Amerhanova, S.K.; Belenok, M.G.; Saifina, L.F.; Semenov, V.E.; Kataev, V.E. Synthesis, antimicrobial activity and cytotoxicity of triphenylphosphonium (TPP) conjugates of 1,2,3-triazolyl nucleoside analogues. Bioorg. Chem. 2021, 116, 105328. [Google Scholar] [CrossRef]
- AAT Bioquest Inc. Quest GraphTM IC50 Calculator. 2022. (Version 2022). Available online: https://www.aatbio.com/tools/ic50-calculator (accessed on 25 June 2022).
- Available online: https://gaussian.com/citation/ (accessed on 31 January 2023).
- Zhao, Y.; Truhlar, D.G. The M06 suite of density functionals for main group thermochemistry, thermochemical kinetics, noncovalent interactions, excited states, and transition elements: Two new functionals and systematic testing of four M06-class functionals and 12 other functionals. Theor. Chem. Acc. 2008, 120, 215–241. [Google Scholar] [CrossRef] [Green Version]
- Grimme, S.; Antony, J.; Ehrlich, S.; Krieg, H. A consistent and accurate ab initio parametrization of density functional dispersion correction (DFT-D) for the 94 elements H-Pu. J. Chem. Phys. 2010, 132, 154104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marenich, A.V.; Cramer, C.J.; Truhlar, D.G. Universal Solvation Model Based on Solute Electron Density and on a Continuum Model of the Solvent Defined by the Bulk Dielectric Constant and Atomic Surface Tensions. J. Phys. Chem. B 2009, 113, 6378–6396. [Google Scholar] [CrossRef] [PubMed]







| Compounds | IC50, µM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cancer Cell Lines | Normal Cell Lines | |||||||||
| HuTu 80 | PC3 | PANC-1 | MCF-7 | M-HeLa | T98G | A549 | A375 | WI38 | Chang Liver | |
| 3 | >100 | nd | >100 | nd | 94.1 ± 8.6 | nd | nd | nd | nd | >100 |
| 2a | > 100 | nd | nd | 31.0 ± 2.6 | 16.1 ± 1.3 | nd | nd | nd | nd | >100 |
| 2b | 86.6 ± 6.8 | nd | nd | 34.2 ± 3.0 | 17.1 ± 1.3 | nd | nd | nd | nd | >100 |
| 2c | >100 | nd | nd | 21.8 ± 1.7 | 38.0 ± 2.8 | nd | nd | nd | nd | >100 |
| 2d | 63.2 ± 5.6 | nd | nd | 16.0 ± 1.2 | 7.4 ± 0.7 | nd | nd | nd | nd | 52 ± 3.5 |
| 2e | nd | nd | nd | >100 | 45.3 ± 3.2 | nd | nd | nd | nd | >100 |
| 4a | 5.2 ± 0.4 | 14.0 ± 1.2 | 20.0 ± 1.7 | 7.6 ± 0.6 | 4.2 ± 0.3 | 12.4 ± 1.2 | 13.5 ± 1.2 | 13.5 ± 1.2 | 7.2 ± 0.6 | 12.0 ± 1.2 |
| 4b | 5.4 ± 0.3 | 11.0 ± 0.8 | 5.3 ± 0.4 | 3.1 ± 0.2 | 2.9 ± 0.2 | 8.3 ± 0.7 | 9.3 ± 0.8 | 11.4 ± 0.9 | 5.3 ± 0.4 | 7.0 ± 1.5 |
| 4c | 0.9 ± 0.07 | 1.2 ± 1.0 | 11.2 ± 0.9 | 1.1 ± 0.1 | 0.9 ± 0.07 | 2.2 ± 0.1 | 0.9 ± 0.08 | 2.9 ± 0.2 | 2.0 ± 0.1 | 2.1 ± 0.7 |
| 4d | 13.1 ± 1.1 | 11.3 ± 0.9 | 11.9 ± 0.9 | 9.0 ± 0.7 | 6.3 ± 0.5 | 7.9 ± 0.7 | 9.0 ± 0.7 | 17.0 ± 1.4 | 11.3 ± 1.1 | 21.0 ± 2.4 |
| 4e | 17.1 ± 1.3 | 12.3 ± 1.1 | 17.4 ± 1.3 | 21.5 ± 1.8 | 12.0 ± 1.0 | 40.2 ± 3.1 | 48.3 ± 3.7 | 53.1 ± 4.1 | 25.7 ± 2.2 | 14.3 ± 1.3 |
| 5a | 11.0 ± 0.9 | 7.7 ± 0.6 | 13.5 ± 1.1 | 12.1 ± 1.1 | 7.7 ± 0.6 | 26.8 ± 2.2 | 48.4 ± 3.5 | 21.6 ± 1.8 | 11.4 ± 0.9 | 15.1 ± 1.7 |
| 5c | 3.9 ± 0.3 | 6.8 ± 0.5 | 5.0 ± 0.3 | 4.5 ± 0.4 | 2.4 ± 0.2 | 7.7 ± 0.6 | 7.7 ± 0.6 | 9.0 ± 0.8 | 5.0 ± 0.4 | 4.1 ± 0.8 |
| 5d | 4.9 ± 0.3 | 5.9 ± 0.4 | 2.8 ± 0.2 (SI = 3.3) | 2.1 ± 0.1 (SI = 4.4) | 2.0 ± 0.1 (SI = 4.6) | 4.8 ± 0.4 | 5.2 ± 0.4 | 5.9 ± 0.5 | 8.4 ± 0.7 | 9.2 ± 1.9 |
| DOX | 0.2 ± 0.01 | 1.4 ± 0.1 | 2.2 ± 0.1 | 0.4 ± 0.03 | 2.1 ± 0.2 | 2.0 ± 0.1 | 0.7 ± 0.05 | 0.3 ± 0.02 | 0.4 ± 0.02 | 0.5 ± 0.04 |
| SF | 6.2 ± 0.5 | 11.3 ± 0.9 | 12.0 ± 1.1 | 27.5 ± 2.3 | 25.0 ± 1.9 | 8.6 ± 0.7 | 25.2 ± 2.2 | 6.8 ± 0.5 | 6.6 ± 0.5 | 21.7 ± 1.7 |
| Compounds | Minimum Inhibitory Concentration (MIC), µg/mL | ||||
|---|---|---|---|---|---|
| Sa | Bc | Ef | MRSA-1 | MRSA-2 | |
| 2a | - | - | - | - | - |
| 2c | - | - | - | - | - |
| 2d | - | - | - | - | - |
| 3 | - | - | - | - | - |
| 4a | - | - | - | - | - |
| 4c | - | - | - | - | - |
| 4d | - | - | - | - | - |
| 5a | 125 ± 11 | 62.5 ± 5.3 | 125 ± 10 | 250 ± 20 | 250 ± 20 |
| 5c | 31.3 ± 2.3 | 31.3 ± 2.5 | 62.5 ± 5.3 | 62.5 ± 5.5 | 250 ± 20 |
| 5d | 15.6 ± 1.2 | 62.5 ± 5.4 | 62.5 ± 5.2 | 62.5 ± 5.3 | 250 ± 19 |
| Chloramphenicol | 31.3 ± 2.2 | 62.5 ± 5.4 | 62.5 ± 5.2 | nd | nd |
| Ketoconazole | - | - | - | - | - |
| Minimum bactericidal and fungicidal concentrations (MBC), (MFC) µg/ml | |||||
| 5a | 250 ± 19 | - | - | 250 ± 21 | - |
| 5c | - | 250 ± 20 | - | - | - |
| 5d | 125 ± 10 | - | - | 250 ± 20 | 250 ± 19 |
| Chloramphenicol | - | - | - | - | - |
| Ketoconazole | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chugunova, E.; Gibadullina, E.; Matylitsky, K.; Bazarbayev, B.; Neganova, M.; Volcho, K.; Rogachev, A.; Akylbekov, N.; Nguyen, H.B.T.; Voloshina, A.; et al. Diverse Biological Activity of Benzofuroxan/Sterically Hindered Phenols Hybrids. Pharmaceuticals 2023, 16, 499. https://doi.org/10.3390/ph16040499
Chugunova E, Gibadullina E, Matylitsky K, Bazarbayev B, Neganova M, Volcho K, Rogachev A, Akylbekov N, Nguyen HBT, Voloshina A, et al. Diverse Biological Activity of Benzofuroxan/Sterically Hindered Phenols Hybrids. Pharmaceuticals. 2023; 16(4):499. https://doi.org/10.3390/ph16040499
Chicago/Turabian StyleChugunova, Elena, Elmira Gibadullina, Kirill Matylitsky, Baurat Bazarbayev, Margarita Neganova, Konstantin Volcho, Artem Rogachev, Nurgali Akylbekov, Hoang Bao Tran Nguyen, Alexandra Voloshina, and et al. 2023. "Diverse Biological Activity of Benzofuroxan/Sterically Hindered Phenols Hybrids" Pharmaceuticals 16, no. 4: 499. https://doi.org/10.3390/ph16040499