Factors and Practices Associated with Self-Medicating Children among Mexican Parents
Abstract
:1. Introduction
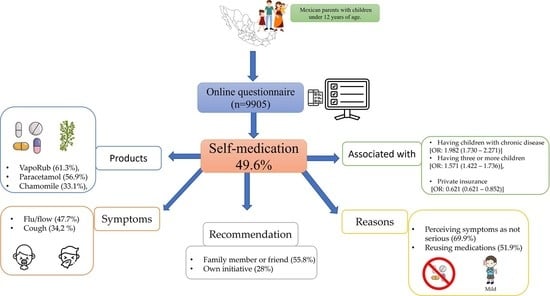
2. Results
2.1. Demographic Characteristics
2.2. Associated Factors
2.3. Predictors Factors
2.4. Products Used
2.5. Symptom Treated
2.6. Reason for Self-Medication
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Data Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Library of Medicine. Self-medication. En: MeSH Descriptor Data. Available online: https://meshb.nlm.nih.gov/record/ui?ui=D012651 (accessed on 5 July 2022).
- Pereira, F.S.; Bucaretchi, F.; Stephan, C.; Cordeiro, R. Self-medication in children and adolescents. J. Pediatr. 2007, 83, 453–458. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, The Netherlands, 26–28 August 1998; World Health Organization: Geneva, Switzerland, 1998; Available online: https://apps.who.int/iris/handle/10665/65860 (accessed on 5 July 2022).
- World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication; World Health Organization: Geneva, Switzerland, 2000; Available online: https://apps.who.int/iris/handle/10665/66154 (accessed on 5 July 2022).
- Batchelor, H.K.; Marriott, J.F. Paediatric pharmacokinetics: Key considerations. Br. J. Clin. Pharmacol. 2015, 79, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Wilfond, B.S. Pediatric Drug Labeling and Imperfect Information. Hastings Cent. Rep. 2020, 50, 3. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Temeck, J.W.; Chambers, W.; Perkins, G.; Bonnel, R.; Murphy, D. Extrapolation of efficacy in pediatric drug development and evidence-based medicine: Progress and lessons learned. Ther. Innov. Regul. Sci. 2018, 52, 199–205. [Google Scholar] [CrossRef]
- Moulis, F.; Durrieu, G.; Lapeyre-Mestre, M. Off-label and unlicensed drug use in children population. Therapie 2018, 73, 135–149. [Google Scholar] [CrossRef]
- Gore, R.; Chugh, P.K.; Tripathi, C.D.; Lhamo, Y.; Gautam, S. Pediatric Off-Label and Unlicensed Drug Use and Its Implications. Curr. Clin. Pharmacol. 2017, 12, 18–25. [Google Scholar] [CrossRef]
- Blanco-Reina, E.; Vega-Jiménez, M.A.; Ocaña-Riola, R.; Márquez-Romero, E.I.; Bellido-Estévez, I. Drug prescriptions study in the outpatient setting: Assessment of off-label uses in children. Aten. Primaria 2014, 47, 344–350. [Google Scholar] [CrossRef]
- Morales-Carpi, C.; Estañ, L.; Rubio, E.; Lurbe, E.; Morales-Olivas, F.J. Drug utilization and off-label drug use among Spanish emergency room pediatric patients. Eur. J. Clin. Pharmacol. 2010, 66, 315–320. [Google Scholar] [CrossRef]
- Ortiz, M.V.; Ruiz-Cabello, F.J.S.; Uberos, J.; Ros, A.F.C.; Ortiz, C.V.; Morales, M.C.A.; Hoyos, A.M. Self-medication, self-prescription and medicating “by proxy” in paediatrics. An. Pediatría 2017, 86, 264–269. [Google Scholar] [CrossRef]
- Du, Y.; Knopf, H. Self-medication among children and adolescents in Germany: Results of the National Health Survey for Children and Adolescents (KiGGS). Br. J. Clin. Pharmacol. 2009, 68, 599–608. [Google Scholar] [CrossRef] [Green Version]
- Oshikoya, K.A.; Njokanma, O.F.; Bello, J.A.; Ayorinde, E.O. Family self-medication for children in an urban area of Nigeria. Paediatr. Perinat. Drug Ther. 2007, 8, 124–130. [Google Scholar] [CrossRef]
- Kariyawasam, S.H.; Nanayakkara, D.N.; Mohottiarachchi, M.A.C.P.; Nandasena, Y.L.S. A descriptive cross-sectional study on mothers self-medicating children. Sri Lanka J. Child Health 2009, 34, 7–12. [Google Scholar] [CrossRef]
- Ley General de Salud (LGS). Articulo 226 (México). Available online: https://www.diputados.gob.mx/LeyesBiblio/pdf_mov/Ley_General_de_Salud.pdf (accessed on 5 July 2022).
- Eldalo, A.S. Saudi parent’s attitude and practice about self-medicating their children. Arch. Pharm. Pract. 2013, 4, 57–62. [Google Scholar] [CrossRef]
- Siponen, S.; Ahonen, R.; Kiviniemi, V.; Hämeen-Anttila, K. Association between parental attitudes and self-medication of their children. Int. J. Clin. Pharm. 2013, 35, 113–120. [Google Scholar] [CrossRef]
- Eldalo, A.S.; El-Hadiyah, T.M.H.; Yousif, M.A. Sudanese parents’ knowledge, attitudes and practice about self-medication to their children: Qualitative study. Saudi J. Health Sci. 2013, 2, 103–107. [Google Scholar] [CrossRef]
- Alonso-Castro, A.J.; Domínguez, F.; Ruiz-Padilla, A.J.; Campos-Xolalpa, N.; Zapata-Morales, J.R.; Carranza-Alvarez, C.; Maldonado-Miranda, J.J. Medicinal Plants from North and Central America and the Caribbean Considered Toxic for Humans: The Other Side of the Coin. Evid. -Based Complement. Altern. Med. 2017, 2017, 9439868. [Google Scholar] [CrossRef]
- Heard, K.; Bui, A.; Mlynarchek, S.L.; Green, J.L.; Bond, G.R.; Clark, R.F.; Kozer, E.; Koff, R.S.; Dart, R.C. Toxicity from repeated doses of acetaminophen in children: Assessment of causality and dose in reported cases. Am. J. Ther. 2014, 21, 174–183. [Google Scholar] [CrossRef]
- de Vries, T.W.; van Hunsel, F. Adverse drug reactions of systemic antihistamines in children in the Netherlands. Arch. Dis. Child. 2016, 101, 968–970. [Google Scholar] [CrossRef]
- Du, Y.; Wolf, I.K.; Zhuang, W.; Bodemann, S.; Knöss, W.; Knopf, H. Use of herbal medicinal products among children and adolescents in Germany. BMC Complement. Altern. Med. 2014, 14, 218. [Google Scholar] [CrossRef]
- Kantar, A.; Klimek, L.; Cazan, D.; Sperl, A.; Sent, U.; Mesquita, M. An overview of efficacy and safety of ambroxol for the treatment of acute and chronic respiratory diseases with a special regard to children. Multidiscip. Respir. Med. 2020, 15, 511. [Google Scholar] [CrossRef] [Green Version]
- Abubakar, U.; Yusuf, K.; Abdu, G.; Saidu, S.; Jamila, G.; Fatima, A. Ethnopharmacological survey of medicinal plants used for the management of pediatric ailments in Kano State, Nigeria. Res. J. Pharmacogn. 2017, 4, 29–39. [Google Scholar]
- Nalumansi, P.; Kamatenesi-Mugisha, M.; Anywar, G. Medicinal plants used in Paediatric Health Care in Namungalwe sub county, Iganga District, Uganda. Nov. J. Med. Biol. Sci. 2014, 2, 1–14. [Google Scholar] [CrossRef]
- Gardiner, P.; Adams, D.; Filippelli, A.C.; Nasser, H.; Saper, R.; White, L.; Vohra, S. A systematic review of the reporting of adverse events associated with medical herb use among children. Glob. Adv. Health Med. 2013, 2, 46–55. [Google Scholar] [CrossRef]
- Malangu, N. Contribution of plants and traditional medicines to the disparities and similarities in acute poisoning incidents in Botswana, South Africa and Uganda. Afr. J. Tradit. Complement. Altern. Med. 2014, 11, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Juárez-Vázquez, M.; Carranza-Álvarez, C.; Alonso-Castro, A.J.; González-Alcaraz, V.F.; Bravo-Acevedo, E.; Chamarro-Tinajero, F.J.; Solano, E. Ethnobotany of medicinal plants used in Xalpatlahuac, Guerrero, México. J. Ethnopharmacol. 2013, 148, 521–527. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística y Geografía (INEGI). Estadísticas a Propósito del día del niño (30 de Abril). Available online: https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2021/EAP_Nino21.pdf (accessed on 13 May 2020).
- Asociación Mexicana de Agencias de Inteligencia de Mercado y Opinión, AMAI [Mexican Association of Market Intelligence]. 2018. Available online: http://nse.amai.org/wp-content/uploads/2018/04/Cuestionario-NSE-2018.pdf (accessed on 13 May 2020).
- Reuben, R.C.; Danladi, M.; Saleh, D.A.; Ejembi, P.E. Knowledge, attitudes and practices towards COVID-19: An epidemiological survey in North-Central Nigeria. J. Community Health 2021, 46, 457–470. [Google Scholar] [CrossRef]
| Characteristic | TOTAL N = 9905 | Self-Medication Frequency (n (%)) | OR a (95% CI) | AOR b (95% CI) | |
|---|---|---|---|---|---|
| YES n = 4908 (49.6) | NO n = 4997 (50.4) | ||||
| Sociodemographic | |||||
| Years (mean ± SD) | 34.64 ± 9.29 | 35.35 + 9.26 | 33.95 + 9.26 | N/A | 0.999 (0.991–1.008) |
| Older than 35 years | 4384 (44.3) | 2364 (53.9) | 2020 (46.1) | 1.369 (1.265–1.483) * | 1.181 (1.013–1.377) * |
| 18–35 years | 5521 (55.7) | 2544 (46.1) | 2977 (53.9) | ||
| Gender | |||||
| Female | 7115 (71.8) | 3627 (51) | 3488 (49) | 1.225 (1.122–1.337) * | 1.221 (1.116–1.335) * |
| Male | 2790 (28.2) | 1281 (45.9) | 1509 (54.1) | ||
| Number of children | |||||
| 1 | 4109 (41.5) | 1802 (43.9) | 2307 (56.1) | Ref. | Ref. |
| 2 | 3266 (33) | 1712 (52.4) | 1554 (47.6) | 1.410 (1.286–1.547) * | 1.299 (1.172–1.440) * |
| 3 or more | 2530 (25.5) | 1394 (55.1) | 1136 (44.9) | 1.571 (1.422–1.736) * | 1.387 (1.223–1.572) * |
| Chronic disease in children | |||||
| Yes | 1001 (10.1) | 646 (64.5) | 355 (35.5) | 1.982 (1.730–2.271) * | 1.898 (1.652–2.180) * |
| No | 8904 (89.9) | 4262 (47.9) | 4642 (52.1) | ||
| Education | |||||
| Elementary and middle school | 1944 (19.6) | 940 (48.4) | 1004 (51.6) | Ref. | Ref. |
| High school | 2966 (29.9) | 1572 (53) | 1394 (47) | 1.204 (1.074–1.351) * | 1.328 (1.174–1.503) * |
| College-postgraduate | 4995 (50.4) | 2396 (48) | 2599 (52) | 0.985 (0.887–1.094) | 1.185 (1.040–1.351) * |
| Place of residence | |||||
| Rural | 1676 (19.9) | 817 (48.7) | 859 (51.3) | 0.962 (0.866–1.069) | 0.978 (0.875–1.092) |
| Urban | 8229 (83.1) | 4091 (49.7) | 4138 (50.3) | ||
| Employment status | |||||
| Housewife/Employed | 8177 (82.6) | 4146 (50.7) | 4031 (49.3) | 1.402 (1.244–1.581) * | 1.291 (1.137–1.466) * |
| Unemployed | 473 (4.8) | 231 (48.8) | 242 (51.2) | 1.301 (1.053–1.609) * | 1.249 (1.003–1.555) * |
| Related to the health sector | 1255 (12.7) | 531 (42.3) | 724 (57.7) | Ref. | Ref. |
| Socioeconomic status | |||||
| High | 3096 (31.3) | 1540 (49.7) | 420 (50.3) | 1.350 (1.147–1.589) * | 1.462 (1.212–1.762) * |
| Middle | 6081 (61.4) | 3060 (50.3) | 3021 (49.7) | 1.381 (1.182–1.613) * | 1.404 (1.191–1.656) * |
| Low | 728 (7.3) | 308 (42.3) | 420 (57.7) | Ref. | Ref. |
| Social security | |||||
| Yes | 6700 (67.6) | 3316 (49.5) | 3384 (50.5) | Ref | Ref. |
| No | 2508 (25.3) | 1302 (51.9) | 1206 (48.1) | 1.102 (1.005–1.208) * | 1.174 (1.067–1.292) * |
| Private insurance | 697 (7) | 290 (41.6) | 407 (58.4) | 0.621 (0.621–0.852) * | 0.730 (0.620–0.858) * |
| Products | Used (n) | Prevalence Users % n = 4908 |
|---|---|---|
| Medications | 3732 | 76 |
| Vicks VapoRub | 3008 | 61.3 |
| Acetaminophen | 2792 | 56.9 |
| Buscapina compositum | 414 | 8.4 |
| NSAIDs | 1358 | 27.7 |
| Ibuprofen * | 1292 | |
| Ambroxol | 784 | 16 |
| Anti-flu drugs | 840 | 17.1 |
| Loratadine * | 675 | |
| Phenylephrine * | 126 | |
| Antibiotics | 488 | 9.9 |
| Amoxicillin * | 431 | |
| Metronidazole | 180 | 3.7 |
| Another | 47 | 1 |
| CAM | 2738 | 55.8 |
| Chamomile | 1627 | 33.1 |
| Honey | 1319 | 26.9 |
| Multivitamin supplements | 706 | 14.4 |
| Arnica | 686 | 14 |
| Aloe | 676 | 13.8 |
| Mint | 439 | 8.9 |
| Guava | 434 | 8.8 |
| Onion | 430 | 8.8 |
| Wormseed | 321 | 6.5 |
| Rice water | 287 | 5.8 |
| Thyme | 255 | 5.2 |
| Others | 931 | 19 |
| Palo azul (wood blue) * | 144 | |
| Peppermint * | 78 | |
| Lemon * | 77 | |
| Garlic * | 71 | |
| Ginger * | 67 | |
| Mexican mullein * | 61 | |
| Eucalypt * | 53 |
| Symptom | Treated (n) | Prevalence Users % n = 4908 |
|---|---|---|
| Flu | 2339 | 47.7 |
| Cough | 1679 | 34.2 |
| Indigestion | 857 | 17.5 |
| Diarrhea | 853 | 17.4 |
| Fever | 705 | 14.4 |
| Wounds | 567 | 11.6 |
| Insomnia | 302 | 6.2 |
| Insect bites | 252 | 5.1 |
| Vomiting | 213 | 4.3 |
| Dermatitis | 227 | 4.6 |
| Urinary infection | 110 | 2.2 |
| Another | 431 | 8.8 |
| Common Name of Medicinal Plant | Way of Preparation/Plant Part Used/Application | Symptom |
|---|---|---|
| Chamomile | Infusion of whole plant in water, oral administration | Indigestion, insomnia, and flu |
| Arnica | Maceration of whole plant in ethanol, topical administration | Wounds |
| Aloe | Decoction of whole plant, topical administration | Wounds, insect bites, and dermatitis |
| Mint | Infusion of aerial parts, oral administration | Flu, fever, cough, flu, and vomiting |
| Guava | Infusion of leaves in water, oral administration | Diarrhea, indigestion |
| Onion | Infusion of bulb in water, oral administration | Cough |
| Wormseed | Infusion of leaves and stem in water, oral administration | Indigestion |
| Rice water | Infusion of seeds in water, oral administration | Diarrhea and indigestion |
| Thyme | Infusion of whole plan in water, oral administration | Flu and indigestion |
| Palo azul (wood blue) | Infusion of bark in water, oral administration | Urinary infection |
| Peppermint | Infusion of leaves and branches, oral administration | Vomiting, cough, and flu |
| Lemon | Infusion of leaves in water, oral administration | Cough and flu |
| Garlic | Infusion of bulb in water, oral administration | Cough |
| Ginger | Infusion of roots, oral administration | Cough |
| Mexican mullein | Infusion of flowers in water, oral administration | Flu, fever, cough, and flu |
| Eucalypt | Infusion of leaves in water, oral administration | Cough and flu |
| Reason | n = 4908 (%) | ||
|---|---|---|---|
| Disagree | Neutral | Agree | |
| Expensive medical consultation | 1635 (33.3) | 2262 (46.1) | 1011 (20.6) |
| The medical office is away from home | 1938 (39.5) | 2082 (42.4) | 888 (18.1) |
| Expensive drugs | 1293 (26.3) | 2078 (42.3) | 1537 (31.3) |
| Reusing leftover drugs | 936 (19.1) | 1426 (29.1) | 2546 (51.9) |
| Preference for natural medicine | 803 (16.4) | 2389 (48.7) | 1716 (35) |
| Non-severe symptoms | 321 (6.5) | 115 (23.5) | 3432 (69.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alonso-Castro, A.J.; Ruiz-Noa, Y.; Martínez-de la Cruz, G.C.; Ramírez-Morales, M.A.; Deveze-Álvarez, M.A.; Escutia-Gutiérrez, R.; Carranza-Álvarez, C.; Domínguez, F.; Maldonado-Miranda, J.J.; Ruiz-Padilla, A.J. Factors and Practices Associated with Self-Medicating Children among Mexican Parents. Pharmaceuticals 2022, 15, 1078. https://doi.org/10.3390/ph15091078
Alonso-Castro AJ, Ruiz-Noa Y, Martínez-de la Cruz GC, Ramírez-Morales MA, Deveze-Álvarez MA, Escutia-Gutiérrez R, Carranza-Álvarez C, Domínguez F, Maldonado-Miranda JJ, Ruiz-Padilla AJ. Factors and Practices Associated with Self-Medicating Children among Mexican Parents. Pharmaceuticals. 2022; 15(9):1078. https://doi.org/10.3390/ph15091078
Chicago/Turabian StyleAlonso-Castro, Angel Josabad, Yeniley Ruiz-Noa, Gissela Cristel Martínez-de la Cruz, Marco Antonio Ramírez-Morales, Martha Alicia Deveze-Álvarez, Raymundo Escutia-Gutiérrez, Candy Carranza-Álvarez, Fabiola Domínguez, Juan José Maldonado-Miranda, and Alan Joel Ruiz-Padilla. 2022. "Factors and Practices Associated with Self-Medicating Children among Mexican Parents" Pharmaceuticals 15, no. 9: 1078. https://doi.org/10.3390/ph15091078